Abstract
Background
Myelin oligodendrocyte glycoprotein antibody-associated disease is usually associated with optic neuritis, acute disseminated encephalomyelitis or transverse myelitis. We are presenting a rare case report wherein myelin oligodendrocyte glycoprotein antibody seropositivity was associated with hemorrhagic longitudinally extensive transverse myelitis. To our knowledge, no such cases were found to be published.
Case presentation
A 15-year-old female came with complaints of sudden onset paraparesis. MRI was performed within 48 h from the episode of paraparesis, which revealed a long-segment, intramedullary, expansile and heterogeneously enhancing spinal cord lesion extending from T1 vertebral level up to conus medullaris. Few foci of blooming were also noted within the spinal cord on gradient sequences. Laboratory evaluation of cerebrospinal fluid analysis revealed no significant abnormality. Neuromyelitis optica antibodies were negative, and myelin oligodendrocyte glycoprotein antibodies (MOG) showed seropositivity. The patient was started on methylprednisolone and plasmapheresis for the same after which the patient gradually improved and regained her ability to walk. Follow-up MRI was performed after 4 weeks, which revealed significant reduction in the extent of the intramedullary lesion described earlier.
Conclusions
Hemorrhagic longitudinally extensive transverse myelitis without any involvement of optic nerves and brain may show MOG seropositivity, and it should be considered as one of the differential diagnosis in acute myelopathy.
Similar content being viewed by others
Background
MOGAD is most commonly seen in children and young adults [1]. Optic neuritis is one of the most common clinical presentation of MOGAD and is usually seen bilaterally [2, 3]. Spinal cord findings in MOGAD include abnormal T2 hyperintensity, centrally located involving both gray and white matter [2]. Dubey et al. [4] described a characteristic MRI finding in MOGAD, which was sagittal T2 hyperintense line surrounded by more hazy T2 hyperintense signal involving the anterior and posterior gray matter horns. The spinal cord presentation of MOGAD may be in the form of: a) longitudinally extensive transverse myelitis (involving three or more vertebral segments) or b) short lesions involving less than two vertebral segments [5, 6]. The involvement of conus medullaris is observed more in MOGAD spectrum more than any other reported demyelinating disorders [4, 6, 7].
The hemorrhagic longitudinally extensive transverse myelitis as a standalone finding without the involvement of brain and optic nerves was not reported in any of the MOGAD spectrum of disorders.
Case presentation
Clinical profile
A 15-year-old female came with complaints of sudden onset paraparesis. Patient had history of urinary retention 8 days before the episode of paraparesis. There was no history of trauma/fever/recent vaccination/hereditary disorders/previous history of similar episodes.
Blood investigations
Routine complete blood counts and cerebrospinal fluid evaluations were normal. Serum myelin oligodendrocyte glycoprotein (MOG) antibodies showed seropositivity, while the neuromyelitis optica antibodies (NMOs) were negative.
MRI findings
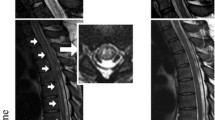
MRI was performed within 48 h of the onset of paraparesis, which revealed a long-segment, intramedullary, expansile, heterogeneously enhancing spinal cord lesion extending from T1 vertebral level till conus medullaris. Few foci of blooming were also noted in the spinal cord on gradient sequences (Fig. 1a–f). Brain and orbit MRI evaluation was normal. Although consideration was given for spinal tumors like ependymoma and astrocytoma, the acute presentation of the symptoms made them clinically less likely. A diagnosis of MOGAD-associated hemorrhagic longitudinally extensive transverse myelitis was made.
a T2 W sagittal image and b FLAIR sagittal image showing a long-segment T2 hyperintense signal (orange arrow) extending till conus medullaris, with few hypointense areas (blue arrows) in between. c Gradient sagittal image showing few areas of blooming within the spinal cord(blue arrows). d I–IV T2 W axial images at T8, T10, T11 and T12 levels, respectively, showing expansile T2 hyperintense spinal cord lesion with few hypointense areas within. e T1 fat-saturated pre-contrast sagittal image. f T1 fat-saturated post-contrast sagittal image showing heterogeneous areas of post-contrast enhancement (white arrows)
Treatment
The patient was started on IV methylprednisolone 1 g/day for 5 days followed by 5 cycles of plasmapheresis on alternate days.
Follow-up
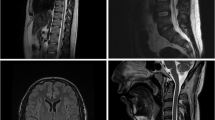
Four weeks following treatment, the patient gradually improved and regained her ability to walk and follow-up MRI revealed significant decrease in the spinal cord lesion (Fig. 2a–c) suggesting good response to the treatment and establishing the diagnosis of MOGAD-positive hemorrhagic longitudinally extensive transverse myelitis.
Follow-up MRI images after 28 days. a: T2 sagittal image showing significant reduction in the T2 hyperintensities within the spinal cord (green arrows), b: Pre-contrast T1 fat-saturated sagittal image, c: Post-contrast T1 fat-saturated sagittal image showing significantly reduced heterogeneous post-contrast enhancement (black arrow) within the spinal cord as compared to previous MRI
Conclusions
Hemorrhagic longitudinally extensive transverse myelitis as a standalone finding without any involvement of optic nerves and brain may show MOGAD seropositivity and should be considered as one of the differential diagnosis in cases of acute myelopathy.
Availability of data and materials
The data and materials supporting the findings of this study are available on request from the corresponding author.
Abbreviations
- MOG:
-
Myelin oligodendrocyte glycoprotein
- MOGAD:
-
Myelin oligodendrocyte glycoprotein antibody-associated disease
- MRI:
-
Magnetic resonance imaging
- IV:
-
Intra-venous
- NMO:
-
Neuromyelitis optica
References
Reindl M, Rostasy K (2015) MOG antibodyassociated diseases. Neurol Neuroimmunol Neuroinflamm 2:e60
Shahriari M, Sotirchos ES, Newsome SD, Yousem DM (2021) MOGAD: how it differs from and resembles other neuroinflammatory disorders. Am J Roentgenol 216(4):1031–1091
Pröbstel AK, Rudolf G, Dornmair K et al (2015) Anti-MOG antibodies are present in a subgroup of patients with a neuromyelitis optica phenotype. J Neuroinflammation 12(1):1–7
Dubey D, Pittock SJ, Krecke KN et al (2019) Clinical, radiologic, and prognostic features of myelitis associated with myelin oligodendrocyte glycoprotein autoantibody. JAMA Neurol 76(3):301–309
Jarius S, Ruprecht K, Kleiter I, Cooperation with the Neuromyelitis Optica Study Group (NEMOS) et al (2016) MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 2: epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J Neuroinflamm 13(1):280. https://doi.org/10.1186/s12974-016-0718-0
Kitley J, Waters P, Woodhall M, Leite MI et al (2014) Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA Neurol 71(3):276–283
Kitley J, Leite MI, Küker W et al (2013) Longitudinally extensive transverse myelitis with and without aquaporin 4 antibodies. JAMA Neurol 70(11):1375–1381
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AN, SM, DP, BB and NS analyzed and interpreted the case study. AN and DP were major contributors in writing the case report and review of literature. JS decided the management protocol. All authors contributed to the writing and review of the manuscript and approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by institution ethical committee. Written informed consent was taken from the patient and parents of the patient.
Consent for publication
All authors read and approved the final manuscript. The patient and parents of the patient included in this study gave written and informed consent to publish the data and materials contained within the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nerlekar, A., Malvadkar, S., Patil, D. et al. A rare presentation of myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) as acute hemorrhagic longitudinally extensive transverse myelitis. Egypt J Radiol Nucl Med 54, 189 (2023). https://doi.org/10.1186/s43055-023-01126-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01126-6