Abstract
Background
Magnetic resonance imaging (MRI) is an effective imaging tool for diagnosing spinal disorders. With a high degree of sensitivity and specificity, it gives vital information on the spinal cord, nerve roots, intervertebral discs, and ligamentous structures inside the spine. Dynamic MRI may image patients in flexed and extended postures, showing abnormalities undetected by static MRI studies. It allows for a more complete investigation of each patient and a better knowledge of the real nature of the pathology. Imaging the spine in extension and flexion, or putting the spine in pain, may help spine surgeons improve their diagnostic accuracy. We aimed to assess the diagnostic value of flexion–extension sagittal T2 (Dynamic MRI) for patients with cervical spondylodegenerative diseases.
Results
We found that more spinal canal stenosis levels were detected on extension position MRI compared to a neutral position (128 vs. 133 MUHLE classification system grade 0, 38 vs. 63 MUHLE grade 1, 31 vs. 13 MUHLE grade 2, 13 vs. 1 MUHLE grade 3), which was statistically significant according to MUHLE among total disc levels, with p value < 0.05. While more spinal canal stenosis levels were detected on flexion position MRI than in neutral position (134 vs. 133 MUHLE grade 0, 49 vs. 63 MUHLE grade 1, 23 vs. 13 MUHLE grade 2, 4 vs. 1 MUHLE grade 3), which was statistically insignificant according to MUHLE among total disc levels (p value > 0.05).
Conclusions
Flexion and extension MR imaging demonstrates additional information using a non-invasive technique concerning the dynamic factors in the pathogenesis of cervical spondylodegenerative diseases. DMRI identifies a significant percentage of increased spinal stenosis especially at extension position more than at neutral and flexion positions. So, we recommend to include extension DMRI in investigations for diagnosis and management plans of cervical spondylodegenerative diseases.
Similar content being viewed by others
Background
As the population ages, cervical spinal degeneration becomes increasingly common. Degeneration of the intervertebral discs often develops in men in their second decade of life and in women in their third decade. Degeneration arises at the facet joints posteriorly, leading in impaired mechanical function of the disc and, eventually, spinal instability and clinical symptoms [1].
Magnetic resonance imaging (MRI) is a useful imaging technique for detecting spinal problems. It provides vital data on the spinal cord, nerve roots, intervertebral discs, and ligamentous structures inside the spine with a high degree of sensitivity and specificity [2].
Dynamic MRI may image patients in flexed and extended postures, showing abnormalities undetected by static MRI studies. It allows for a more complete investigation of each patient and better data of the real nature of the pathology. Imaging the spine in extension and flexion may help spine clinicians improve their diagnostic accuracy and treatment plans [3].
We aimed to assess the diagnostic value of flexion–extension sagittal T2 (Dynamic MRI) for patients with cervical spondylodegenerative diseases.
Patients and methods
This prospective cross-sectional study was conducted in our radio-diagnosis department for 2 years (January 2021–January 2023) on 35 patients referred from neurosurgery department, their ages ranging from 30 to 59 years with mean ± SD of 44.03 ± 7.82. There was male predominance with 19 males and 16 females.Weight ranged from 60 to 120 kg with mean ± SD of 88.09 ± 14.07.
Inclusion criteria This study included patients either male or female with ages ranging from 30 to 59 years old suffering from: neck pain, upper limb pain and\or numbness.
Exclusion criteria patients with cervical spine trauma, tumors, infection, prior cervical spine surgery, contraindications to MRI (e.g.: claustrophobia, pacemakers), or inability to tolerate dynamic examination.
Ethical considerations participants were fully informed about the procedures and gave their consent to participate. The research did not put participants in a situation where they might be at risk of harm as a result of their participation. The research guaranteed the participant's confidentiality.
Study tools and procedures
Patient preparation for MRI unit
The procedure was explained to the patients.
Patients were asked to remove things that might affect the magnetic imaging such as Jewellery, Hairpins, eyeglasses, Watches, Dentures, or Hearing aids.
Procedure
The 1.5 T Philips Achieva MRI (Philips Medical Systems, Eindhoven, Netherlands) was used for all cervical spine MRI scans. First, patients underwent a static cervical spine MRI in the supine posture (T1 and T2 weighted sagittal images and T2 weighted axial images); then, a dynamic cervical spine MRI was done (sagittal T2 during flexion and extension positions). We performed the dynamic MRI at the patient's maximum neck flexion and extension angles without any neurologic worsening in side a device consisting of a movable support for the head and a stationary frame attached to the patient’s table. This allowed examination of the cervical spine in positions ranging from 50° of flexion to 30° of extension by increments of 5–10°. For signal reception, a 16 cm circular flexible receive surface coil was placed on the posterior surface of the patient’s neck so that it encircled the cervical spine, allowing free and unrestricted motion at flexion and extension. To shorten the scanning time, T2WI sagittal images only were taken of each neck position for the dynamic MRI. We considered the patients’ pain and aggravation of clinical symptoms since the dynamic MRI required them to stay in fixed neck flexion and extension for an extended period of time (10 min).
Imaging protocol
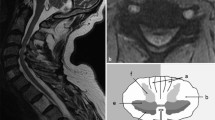
Consisted of a sagittal T1-weighted spin-echo sequence with parameters of 600/20/2 (TR/TE/excitations), a 256 3 192 matrix, and a 25-cm field of view; a sagittal turbo spin-echo T2-weighted sequence with parameters of 4700/112/2 (TR/TE/excitations), a 256 3 192 matrix, and a 25-cm field of view; an axial T2*-weighted gradient-echo sequence in the neutral position (0°) with parameters of 630/15/2 with a 15° flip angle, a 205 3 256 matrix, and a 16-cm field of view; and a sagittal T2-weighted turbo spin-echo sequence at maximum flexion and extension of the neck with parameters of 4700/112/2 (TR/TE/excitations) a 256 3 192 matrix, and a 25-cm field of view. A 3-mm section thickness and 0.5-mm intersection gap were used for all MR images (Figs. 1, 2, 3 and 4).
Image interpretation
All MRI images were analyzed by three experienced radiologists, with at least 10 years of experience each (Figs. 5, 6 and 7).
The MRI images were evaluated for the presence and extent of disc bulge on the cervical cord using the MUHLE classification system. He classified each segment as: 0 = normal, 1 = partial obliteration of the anterior or posterior subarachnoid space, 2 = complete obliteration of subarachnoid space and 3 = cervical cord compression or displacement [4].
Statistical analysis
Recorded data were analyzed using the statistical package for social sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage. Inter observer agreement was determined using the weighted kappa (k) statistic.
-
k value > 0.8 indicating good agreement.
-
k value = 0.8 to 0.6 indicating moderate agreement.
-
K value = 0.6 to 0.2 indicating fair agreement.
-
K value < 0.2 indicating poor agreement.
The following tests were done
-
Chi-square (x2) test of significance was used in order to compare proportions between qualitative parameters.
-
The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p value was considered significant as the following:
-
Probability (P value)
-
P value ≤ 0.05 was considered significant.
-
P value ≤ 0.001 was considered highly significant.
-
P value > 0.05 was considered insignificant.
-
Results
This was a prospective cross-sectional study conducted on 35 patients (each patient had 6 disc levels, making 210 total disc levels). Ages ranged from 30 to 59 years with mean ± SD of 44.03 ± 7.82. As regards sex distribution, there was male predominance with 19 males with a percentage of 54.3% and 16 females with a percentage of 45.7%. Weight ranged from 60 to 120 kg with mean ± SD of 88.09 ± 14.07 (Tables 1, 2 and 3).
All included patients had several clinical findings that correlate with radiological findings either in static MRI or DMRI.
Our imaging was classified using the MUHLE classification system and studied in three positions neutral, flexion, and extension (there were 35 patients; each patient had 6 disc levels, making 210 total disc levels) (Tables 4, 5 and 6).
MUHLE of neutral position imaging among our patients, there were 133 disc levels (63.3%) with "Grade 0," 63 disc levels (30%) with "Grade 1," 13 disc levels (6.2%) with "Grade 2," and one-disc level (0.5%) with "Grade 3" of the neutral position.
MUHLE of flexion position imaging among our patients, there were 134 disc levels (63.8%) with "Grade 0," 49 disc levels (23.3%) with "Grade 1," 23 disc levels (11%) with "Grade 2," and 4 disc levels (1.9%) with "Grade 3" of flexion position.
MUHLE of extension position imaging among our patients group,128 disc levels (61%) had "Grade 0," 38 disc levels (18.1%) had "Grade 1," 31 disc levels (14.8%) had "Grade 2," and 13 disc levels (6.2%) had "Grade 3" of extension position.
In our study, more spinal canal stenosis levels were detected on extension position compared to the neutral position (128 vs. 133 MUHLE grade 0, 38 vs. 63 MUHLE grade 1, 31 vs. 13 MUHLE grade 2, 13 vs. 1 MUHLE grade 3), which was statistically significant according to MUHLE staging among total disc levels, with p value < 0.05.
In our study, more spinal canal stenosis levels were detected on flexion position than in neutral position (134 vs. 133 MUHLE grade 0, 49 vs. 63 MUHLE grade 1, 23 vs. 13 MUHLE grade 2, 4 vs. 1 MUHLE grade 3), which was statistically insignificant according to MUHLE among total disc levels (p value > 0.05).
All MRI images were analyzed with a 90% degree of agreement by three experienced radiologists, with at least 10 years of experience each with k value > 0.8 which indicates good agreement.
Discussion
Despite the fact that dynamic variables are known to play a part in the pathogenesis of cervical spondylodegenerative diseases, the use of MRI in flexion and extension positions for such individuals to evaluate spinal cord compression is unusual. However, it can provide useful information about the compressive pressures that occur during normal everyday cervical mobility. Several prior studies have shown that more stenosis can occur with both cervical flexion and extension positions [5].
Dynamic MRI may reveal the flexional and extensional positions of the cervical spine, which are more similar to the normal state of the cervical spine. Some spinal cord compression might be undetected by static MRI but seen in Dynamic MRI [6].
We conducted our study on 35 patients (each patient had 6 disc levels, making 210 total disc levels), with ages ranging from 30 to 59 years old to assess the diagnostic value of flexion–extension sagittal T2 (Dynamic MRI) for patients with cervical spondylodegenerative diseases in contrast to data obtained from static MRI.
We used MUHLE classification for analyzing degenerative disease of the cervical spine examined with MRI. This classification system classified each segment as: 0 = normal, 1 = partial obliteration of the anterior or posterior subarachnoid space, 2 = complete obliteration of subarachnoid space and 3 = cervical cord compression or displacement [4].
We demonstrated that 63.3% in neutral position versus 61% in extension was Grade 0, 30% in neutral position versus 18% in extension was Grade 1, 6.2% in neutral position versus 14.8% in extension was Grade 2, and 0.5% in neutral position versus 6.2% in extension was Grade 3 which was statistically significant.
Our results were supported by a study on 38 patients that demonstrated that cervical cord compression is more provoked during neck extension. They demonstrated that 42.7% in neutral position versus 28.4% in extension was Grade 1, 53.12% in neutral position versus 64.2% in extension was Grade 2, and 4.18% in neutral position versus 7.4% in extension was Grade 3 which was statistically significant [7].
We demonstrated that more compression levels were detected with dynamic MRI in flexion, however this was statistically insignificant. We demonstrated that 63.3% in neutral position versus 63.8% in flexion was Grade 0, 30% in neutral position versus 23.3% in flexion was Grade 1, 6.2% in neutral position versus 11% in flexion was Grade 2, and 0.5% in neutral position versus 1.9% in flexion was Grade 3.
Actually our findings were contrasted with the study that examined the changes of the spinal canal diameter during neck flexion and extension by looking at the MUHLE grades which revealed that Contrary to several existing reports on the topic, MUHLE grades remained constant or increased in both flexion and extension compared to the neutral neck position [8].
Our results were supported by a study that demonstrated that an investigation of extension MRI revealed an increased number of compression levels in 72% of patients when compared to static MRI findings [9].
Another study agreed with our results as it demonstrated that higher stages of spinal cord compression were found in the extension position compared with the stage in the neutral and flexion positions, upon reviewing the DMRI results, the number of potential levels needing decompression was significantly increased in comparison to static MRI results which supported our results and reinforced the need to add extension dynamic MRI during investigations of cervical spondylodegenerative diseases [10].
Our results were supported by a study that showed that the radiological severity of the spinal canal stenosis increases significantly with extension and decreases significantly with flexion; however, these findings in flexion were contrasted with our findings [11].
Our results agreed with previous studies using dynamic MRIs that had univocally revealed that cervical cord compression is more likely during neck extension [12, 13]. Rather, some research revealed that with neck flexion, the spinal canal width increases [14, 15].
Also, our results were comparable to data from the study conducted on 81 patients that showed that increased cervical cord impingement was seen in 27% (22 of 81) to 31% (19 of 62) of extension MR images and in 3% (two of 62) to 5% (four of 81) of flexion MR images [4].
Conclusions
Flexion and extension MR imaging demonstrates additional information using a non-invasive technique concerning the dynamic factors in the pathogenesis of cervical spondylodegenerative diseases. DMRI identifies a significant percentage of increased spinal stenosis especially at extension position more than at neutral and flexion positions. So, we recommend to include extension DMRI in investigations for diagnosis and management plans of cervical spondylodegenerative diseases.
Limitations
-
Larger sample size and multicenter experience are all necessary to accurately figure out the accuracy of dynamic MRI in cervical spine pathology.
-
We recommend doing dynamic MRI in sagittal and axial planes as, the dynamic MRI protocol in our study did not include axial images so, stenosis was only evaluated in the sagittal plane.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- DMRI:
-
Dynamic MRI
- MUHLE:
-
MUHLE classification system
References
Lao L-F, Zhong G-B, Li Q-y, Liu Z-d (2014) Kinetic magnetic resonance imaging analysis of spinal degeneration: a systematic review. Orthop Surg 6(4):294–299
Ha JH, Lee J-H, Lee JH (2021) Coexisting spine lesions on whole spine T2 sagittal MRI in evaluating spinal degenerative disease. J Korean Med Sci 36(7):e48
Hayashi T, Daubs MD, Suzuki A, Phan K, Shiba K, Wang JC (2014) Effect of Modic changes on spinal canal stenosis and segmental motion in cervical spine. Eur Spine J 23:1737–1742
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH et al (1998) Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol 19:1763–1771
Alkosha HMA, El Adalany MA, Elsobky H, Zidan AS, Sabry A, Awad BI (2022) Flexion/extension cervical magnetic resonance imaging: a potentially useful tool for decision-making in patients with symptomatic degenerative cervical spine. World Neurosurg 164:e1078–e1086
Xu N, Wang S, Yuan H, Liu X, Liu Z (2017) Does dynamic supine magnetic resonance imaging improve the diagnostic accuracy of cervical Spondylotic myelopathy? A review of the current evidence. World Neurosurg 100:474–479
Nigro L, Donnarumma P, Tarantino R, Rullo M, Santoro A, Delfini R (2017) Static and dynamic cervical MRI: two useful exams in cervical myelopathy. J Spine Surg 3(2):212–216. https://doi.org/10.21037/jss.2017.06.01
Park D, Kim B et al (2021) Diagnostic role of flexion-extension central motor conduction time in cervical spondylotic myelopathy. Spine 46(22):1564–1571
Kim CH, Chung CK, Kim KJ et al (2014) Cervical extension magnetic resonance imaging in evaluating cervical spondylotic myelopathy. Acta Neurochir 156:259–266
Xu N, Zhang Y, Zhou G et al (2020) The value of dynamic MRI in the treatment of cervical spondylotic myelopathy: a protocol for a prospective randomized clinical trial. BMC Musculoskelet Disord 21:83. https://doi.org/10.1186/s12891-020-3106-y
Lee Y, Kim SY, Kim K (2018) A dynamic magnetic resonance imaging study of changes in severity of cervical spinal stenosis in flexion and extension. Ann Rehabil Med 42(4):584–590
Bartlett RJ, Rigby AS, Joseph J et al (2013) Extension MRI is clinically useful in cervical myelopathy. Neuroradiology 55:1081–1088
Zeitoun D, El Hajj F, Sariali E et al (2015) Evaluation of spinal cord compression and hyperintense intramedullary lesions on T2-weighted sequences in patients with cervical spondylotic myelopathy using flexion-extension MRI protocol. Spine J 15:668–674
Dalbayrak S, Yaman O, Firidin MN et al (2015) The contribution of cervical dynamic magnetic resonance imaging to the surgical treatment of cervical spondylotic myelopathy. Turk Neurosurg 25:36–42
Xiong C, Daubs MD, Scott TP et al (2017) Dynamic evaluation of the cervical spine and the spinal cord of symptomatic patients using a kinetic magnetic resonance imaging technique. Clin Spine Surg 30:E1149–E1155
Acknowledgements
The author thanks all the study participants for their patience and support.
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
MAA: collected and analyzed the data, wrote the manuscript, prepared cases, performed required measurements and statistical analysis, and prepared figures and tables. SMD: suggested the research idea, shared in data collection and analysis, reviewed literature, statistical analysis, and manuscript editing. MHS: reviewed the manuscript and statistical analysis. HMS: reviewed the manuscript and statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent for participate
Approval of the ethical committee of the ‘Radiology department, Faculty of Medicine, Ain Shams University’ was granted before conducting this prospective study; Local institutional review board approval was granted before conducting this cross-sectional study, and written informed consent was obtained from all patients.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdalhak, M.A.M., Sakr, H.M., Shalaby, M.H. et al. Added value of dynamic MRI in assessment of cervical spondylodegenerative diseases. Egypt J Radiol Nucl Med 54, 100 (2023). https://doi.org/10.1186/s43055-023-01046-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01046-5