Abstract
Background
The Global Initiative for Obstructive Lung Disease (GOLD) staging approach is frequently used to classify the severity of COPD by using spirometry. Recent advancements in artificial intelligence applications enable the automatic identification of COPD severity by chest computer tomography (CT). The goal of this study is to define the role of artificial intelligence in determining the severity of COPD.
Methods
We used a non-contrast CT chest and a computer-aided detection system (Coreline Soft's AVIEW), which was conducted as a descriptive cross sectional study and involved 80 cases. For the diagnosis of parenchymal disease using density mask methods such as inspiratory low attenuation area-950% (%LAA-950 HUINS) and D-value (cluster-size analysis), the spirometry-based Tiffeneau index (TI; calculated as the ratio of forced expiratory volume in the first second (FEV1) to forced vital capacity was used to assess the severity of COPD.
Results
Based on the results of the spirometry, the patients were divided into four groups: mild (n = 23), moderate (n = 39), severe (n = 17), and very severe (n = 1). Insp. LAA-950 (%) in GOLD group 3 was substantially greater than in GOLD groups 2 and 1. Additionally, when compared to groups 2 and 1, the D-value in the GOLD 3 group was significantly higher.
Conclusions
Inspiratory LAA-950% and D-value were found to be significantly related to COPD severity as measured by dyspnea scale and spirometry. Inspiratory LAA-950% was effectively capable of distinguishing between patients with severe and moderate COPD.
Similar content being viewed by others
Background
In radiography, disease evaluation is frequently relied on the training and expertise of the radiologists and can be arbitrary. In contrast to that qualitative assessment, automated quantitative assessment is provided by artificial intelligence (AI), which is superior at spotting intricate patterns in images [1].
Chronic obstructive pulmonary disease (COPD) is defined by the Global Initiative for Obstructive Lung Disease (GOLD) group as a common preventable and treatable disease which is characterized by airflow limitation that is progressive usually and combined by an enhanced chronic inflammatory response in the airways and lung to gases and noxious particles [2].
Chronic obstructive pulmonary disease which encompasses two main disorders—emphysema and chronic bronchitis—is the third greatest cause of disability and the fourth most prevalent cause of death in the USA, according to the Centers for Disease Control and Prevention (CDC) [3].
Spirometry is used to diagnose COPD when the forced expiratory volume in 1 s/ forced vital capacity (FEV1/FVC) ratio following bronchodilator test is less than 0.70. The GOLD staging system is frequently used to categorize the severity of COPD, but it cannot distinguish between its subtypes [4].
The definition of pulmonary emphysema is “dilatation of air pockets distal to the terminal bronchioles and permanent loss of airway walls.” Emphysema thus looks to be a region of relatively lower Housenfield units (HU) (lower CT attenuation).
By calculating that is lower than a specific threshold of HU, the density mask approach quantifies emphysema. These voxel regions are known as low attenuation areas (LAA), and -950 HU is the most widely used agreed value [5].
The size and number of low attenuation areas (LAA) visible in COPD on CT scan are determined by low attenuation (LA) cluster analysis (D-Value). It can provide more morphological details about LAA, possibly reproducing visual evaluation of emphysema pattern [6].
In the current investigation, we looked at how AI-based CT parameters could be used as a potential method for determining the severity of the COPD compared to PFTs.
Methods
All patients provided written informed consent for the current study authorized by the regional institutional ethics committee before taking any data or doing any investigations or imaging techniques.
The research was carried out on the CT unit—Radiology and Chest departments at Suez Canal University hospital in Ismailia, Egypt, with online remote access to a computer-aided detection (CAD) system (Coreline Soft's AVIEW).
Our study was conducted as a descriptive cross-sectional study, lasted two years, from the mid of 2020 to the June of 2022, and included 80 patients. Inclusion criteria included (a) COPD patients referred for a chest CT scan for radiological assessment of morphological disease pattern, and its severity, or patients with COPD referred to rule out coexisting malignancy, (b) Patients who were referred for a CT chest scan to determine the cause of a recent or previous history of dyspnea, wheezy chest, and chronic productive cough for more than three months were included in our study being clinically suspected to have COPD, and (c) patients with COPD clinical diagnosis (FEV1/FVC = 0.7) [7].
Exclusion criteria included (a) patients who refused to participate in the study, (b) patients with coexisting lung carcinoma, (c) patients diagnosed with pneumonia, (d) patients with suspected pulmonary nodule, and (e) patients performed CT chest with IV contrast [8].
All patients had a history taken (age, smoking index, symptoms such as dyspnea and productive cough), a spirometer evaluation, and a CT chest without IV contrast.
CT Technique
CT imaging was performed using 16 slice scanner, Activion 16 model TSX-031A-2012 with standard accessories (Toshiba Medical Systems).
-
CT Protocol:
CT scan was performed as follows:
-
In cranio-caudal direction.
-
Inspiratory CT was obtained.
-
Started from the apices of the lung to lateral costophrenic sulci.
-
Slice thickness = 1 mm.
-
120 kVp, and 80–100 mAs.
-
Reconstruction algorithms smooth & sharp.
-
Pitch ≤ 1
-
No contrast was administrated.
Patients with breathing difficulties were trained, and the scan was performed after breath hold practice.
-
-
Post-Processing:
It was carried out with the help of a pre-installed post-processing application/software, namely Coreline Soft's AVIEW platform, which is a multiplatform software application for medical imaging computing based on the deep learning convolutional neural networks algorithm (CNN). AVIEW Metric's Chest Imaging Platform is an artificial intelligence-based precision medical solution that uses a chest CT scan to plan a solution that can automatically test for COPD and its co-morbidities.
CNN algorithm was used for deep lobe segmentation and airway segmentation, saving time per case from 40 to 2 min and from 60 to 3 min, respectively (Fig. 1).
-
Image Analysis:
CT parameters for diagnosis of COPD parenchymatous subtype were automatically calculated, and an automated report was generated and saved in picture archiving and communication system (PACS).
Pulmonary parameters for COPD diagnosis:
1. Density mask methods for diagnosis of parenchymal disease (emphysema):
-
(i)
Low attenuation areas-950 (%LAA-950 HUINS)—
The emphysema component in COPD was estimated using the percentage area of lung less than -950 HU (the emphysema index, or% LAA-950) [9] (Fig. 2).
-
(ii)
D-value (Cluster-size analysis)
—This represented the emphysema's cumulative frequency size distribution and estimated the emphysematous areas that congregated to form small to large (clustered) regions of emphysema [9].
LAA-950 HUINS analysis (Emphysema index) of the whole lung, RT and LT lobes separately and segments of each lobe in illustrated table, chart and histogram as above. The green coded areas in the coronal image and chart show the lung areas with attenuation less than -950 during inspiration indicating the emphysema index and its distribution throughout the lung with total percent of 46%
In this study, cluster sizes were calculated automatically two-dimensionally (as an area [mm2] using axial CT images). There were threshold CT values available for tracking LAA. The threshold was set at -950 HU. The slopes (D-values) of these relationships with 3D techniques at these threshold CT values were used as LAA cluster analysis measurements. The smaller the LAA, the steeper the slope (increased absolute D-value) (Fig. 3).
Cluster size analysis (D-value) assessment at LAA-950 through the whole lung, RT and LT lobes separately and segments of each lobe and expressed at table, chart and size log–log plot as the cluster sizes were calculated automatically two-dimensionally (as an area [mm2].The different colors express different sizes of the clusters as those less than 1 mm not colored (transparent) (insignificant), blue colored coded for clusters ranges from 1 to 7 mm, green color for cluster size from 7 to 15 mm, and red one for those larger than 15 mm. The log–log plot shows that the steeper the slope, the smaller the cluster size
Spirometry and clinical parameters
A pulmonary function test was performed in accordance with the American Thoracic Society (ATS) guidelines to assess forced expiratory volume in one second (FEV1) and percentage predicted FEV1 (hereafter referred to as FEV1%) [10].
Each patient's dyspnea was assessed using the modified medical research council (mMRC) dyspnea scale, which is a five-point scale ranging from grade 0–4 [11].
Statistical analysis
All analyses were performed using SPSS version 22.0 (IBM, Armonk, New York, USA). Significance was observed with p value < 0.05.
Variables were tested for pattern of distribution using the Kolmogorov–Smirnov test and visual assessment of histograms. Data with normal distribution was expressed as mean ± standard deviation. Correlation between CT-based AI parameters and spirometry and dyspnea were measured using Pearson correlation coefficient for normally distributed variables. The receiver operator characteristic (ROC) curve was used to differentiate between COPD severity subtypes.
Results
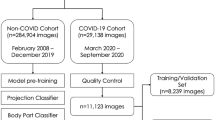
The demographic data of the included population (n = 80) revealed that the patients' mean age was 60 years old. There were almost entirely males (97.5%), with only two females (2.5%) included (Table 1). According to spirometry results, the patients were classified as GOLD 1: mild (n = 23), GOLD 2: moderate (n = 39), GOLD 3: severe (n = 17), and GOLD 4: very severe (n = 1) (Fig. 4). The severe group had a significantly higher mean age than the mild and moderate groups (73.2 versus 52.6 and 58.7 years, respectively, p < 0.0001) (Fig. 5).
The ANOVA test was used to identify significant differences between radiological parameters in relation to the severity of COPD stages. Insp. LAA-950 (%) was significantly higher in the GOLD 3 group than in the GOLD 2 and 1 groups. Furthermore, the D-value was significantly higher in the GOLD 3 group compared to groups 2 and 1 (Table 2).
Even though Insp. LAA-950 (%) had a significant negative relationship with FEV1% and positive relationship with dyspnea score, the D-value had a modest negative relationship with FEV1% and positive relationship with dyspnea score (Table 3).
For the discrimination of moderate from mild COPD, the receiver operator characteristic (ROC) curve assessment of Insp. LAA-950 (%) revealed that a threshold of ≥ 1.75 was a significant cut-off with a sensitivity of 60% and specificity of 78.3% (AUC = 0.750, p = 0.001) (Fig. 6). The threshold was ≥ 0.4 with a sensitivity of 90% but a specificity of 13% in an effort to obtain the optimum values of Insp. LAA-950 (%) (Table 4).
For the discrimination of severe from moderate COPD, the receiver operator characteristic (ROC) curve assessment of Insp. LAA-950 (%) revealed that a threshold of ≥ 19.1 was a significant cut-off with a sensitivity of 78% and specificity of 82.1% (AUC = 0.860, p < 0.0001) (Fig. 7). The threshold was ≥ 11 with a sensitivity of 88.9% but a specificity of 64.1% to obtain the optimum values of Insp. LAA-950 (%) (Table 5).
On the one hand, with a threshold of ≥ − 5.0, the (ROC) curve analysis of the D-value for differentiating between moderate and mild COPD revealed a sensitivity of 77.0% and a specificity of 48.0% (AUC = 0.573, p = 0.340) (Fig. 8). On the other hand, the threshold was ≥ − 5.3 when setting near-90% sensitivity (with 39.1% specificity), and the threshold was ≥ − 3.8 when setting near-90% specificity (with 18.0% sensitivity) (Table 6).
However, the ROC curve of D-value for the discrimination of severe from moderate COPD showed a threshold of ≥ − 4.2 with a sensitivity 77.8% and specificity 60.0% (AUC = 0.705, p = 0.013) (Fig. 9). The threshold was ≥ − 4.3 when setting near-90% sensitivity (with 54.0% specificity) and the threshold was ≥ − 3.5 when setting near-90% specificity (with 28.0% sensitivity) (Table 7).
Discussion
In general, smoking frequency increases the inflammatory and structural changes in the airways, as well as the severity of COPD [12]. Our finding shows that all patients (100%) in the severe group, 64.1% in the moderate group, and 21.7% in the mild group were heavy smokers (p < 0.0001) which emphasized this observation. Only one (4.3%) of our COPD patients did not smoke.
In our study, we observed that the inspiratory (Insp.) low attenuation areas LAA-950 (%) (or emphysema index) was a highly significant AI-based CT parameter that used for emphysema quantification. We found that the patients with severe COPD (28.5 ± 11.5%) had significantly higher values of Insp. LAA-950 (%) (cut-off value ≥ 19.1) than mild (2.9 ± 2.4%) and moderate (11.3 ± 11.2%) cases (cut-off value ≥ 1.75) (F = 37.0, p < 0.0001). In same direction, Anazawa et al. [13] reported that the values of Insp. LAA-950 (%) were significantly higher in late cases with advanced COPD (11.7 ± 8.8%) than in early cases with mild COPD (6.8 ± 10.4%) (p < 0.0001).
In Kumar et al. [14], LAA of a 12.2 cut-off value had 76.5% sensitivity and 72.7% specificity in the prediction of FEV1 < 50% (GOLD 3).
Furthermore, other studies performed by Lynch, AL-Qaisi,Ostrige and Wilkinson confirmed these findings, stating that the Insp. LAA-950 (%) is used to assess the severity of COPD [8, 15].
Tanabe et al. [16] found that Insp. LAA-950 (%) gradually increases over time in COPD patients. Several previous studies revealed that threshold levels around -950 Hounsfield units (HU) for LAA% provide strongest correlation with pathologic extent (severity) of emphysema [17, 18].
We found that Insp. LAA-950 (%) was significantly correlated with FEV1 (r = − 0.75, p < 0.0001). Several comparable studies discovered statistically significant correlations between Insp. LAA-950 (%) and FEV1 [19,20,21,22,23,24,25,26,27,28].
Additionally, there were strong links between Insp. LAA-950 (%) and COPD clinical outcomes [20, 29, 30].
However, one disadvantage of the LAA technique is that it is solely based on CT voxel attenuation and does not use morphological information provided by CT.
Emphysematous lesions exhibit fractal geometry in addition to spatial heterogeneity. This is determined by identifying emphysematous clusters, which are discrete and isolated zones of emphysema.
In our study, we assessed the cumulative frequency size distribution of emphysema and estimated the emphysematous areas that congregated to form small to large (clustered) regions of emphysema.
In the study by Fan et al. [31], cluster sizes were calculated automatically two-dimensionally (as an area [mm2] using axial CT images).
We used a 2D D-value of -950 HU in our study. The smaller the LAA, the steeper the slope (increased absolute D-value). In the current analysis, D-value was significantly correlate with FEV1(r = − 0.469, p < 0.0001).
Our study supports that D-value indicative of severity as it significantly discriminated severe from moderate COPD (cut-off ≥ − 4.2, sensitivity 77.8%, specificity 60.0%, AUC = 0.705, p = 0.013), but insignificantly discriminated moderate from mild COPD (cut-off ≥ − 5.0, sensitivity 77.0%, specificity 48.0%, AUC = 0.573, p = 0.340).
A previous study examined the clinical feasibility of Insp. LAA% -950 HU and D-values of cluster analysis at three different CT value thresholds (-856, -910, and -950 HU) in the evaluation of COPD. LAA% had a stronger correlation with FEV1% (− 0.55, p < 0.0001) than D-value (− 0.27, p < 0.0001) [6].
With the conclusion that low attenuation cluster analysis provides incremental information regarding physiologic severity of COPD, independent of LAA%, Nambu et al. found that 2D D-value-910 HU had the highest correlation coefficients with FEV1%, (r = − 0.350, p < 0.001), and 2D D-value-950 HU had marginal correlation coefficients (r = − 0.196, p = 0.053) [6].
Several earlier studies have employed cluster analysis of LAA to assess the severity of emphysema [6].
Mishima et al. discovered that COPD patients with normal LAA% had significantly lower D-values (i.e., gentler slopes, larger LAA predominant) than healthy subjects. They hypothesized that in COPD patients, small LAA coalesce to form larger LAA and D-value can become smaller without increasing LAA% [32]. Gietema HA et al. [33] confirmed that visually assessed air trapping regions had smaller cluster sizes for the same LAA% as those without air trapping. Another analysis confirmed that not only enlargement of the LAA, but also coalescence of adjoining LAA caused progression of emphysema in patients with acute exacerbation (16).
These latter reports, along with this study, reinforce the idea that cluster analysis, by estimating sizes of LAA that density mask approach cannot assess, namely LAA%, gives additional information to that technique. It is important to consider the LAA threshold level when determining the severity of emphysema.
Our study's strengths include its homogeneity by using a single CT scanner machine.
Another significant strength of our research is that we were able to generate cut-off values for quantitative CT parameters with high diagnostic accuracy, which can provide useful information to radiologists. The all-diagnostic values of the CT parameters were calculated according to a reference standard spirometry parameter (FEV1) which gives accurate results of the tested variables.
Finally, we attempted to eliminate confounding factors by excluding cases with lesions suspicious for malignancy, which can affect overall lung density and confound our findings.
This study also had some limitations, and the generalizability of our study results to the COPD population is hampered by the relatively small number of patients (n = 80), but with a sufficient representative sample in each subgroup of COPD severity (mild = 23, moderate = 39, and severe = 18).
Standardization, optimization, and simplification of methods for quantifying the various components of COPD are required.
Furthermore, quantitative CT has several limitations. The measurement of CT attenuation of the lung by different scanner models, reconstruction algorithms, and CT protocol parameters such as voxel size, tube voltage, and tube current-exposure time product vary significantly. Furthermore, variations in inspiratory and expiratory lung volumes, as well as acquisition techniques, influence CT attenuation values. However, the strong correlations found in this study suggest that the variation caused by these technical factors may be minimal.
Conclusions
Inspiratory LAA-950% and D-value were found to be significantly related to COPD severity as measured by dyspnea scale and spirometry. That can help to guide individualized management strategies and improve disease outcomes in COPD as it provide quantitative information and structural assessment which facilitate early and precise diagnoses.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AI:
-
Artificial intelligence
- CNN:
-
Convolutional neural networks
- COPD:
-
Chronic obstructive pulmonary disease
- D-Value:
-
Cluster-size analysis
- EI:
-
Emphysema index
- FEV:
-
Forced expiratory volume
- FVC:
-
Forced vital capacity
- GOLD:
-
Global initiative for obstructive lung disease
- LAA:
-
Low attenuation area
- PACS:
-
Picture archiving and communication system
References
Wang S, Summers RM (2012) Machine learning and radiology. Med Image Anal 16(5):933–951
Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A et al (2013) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187(4):347–365
WHO. Chronic obstructive pulmonary disease (COPD): WHO; 2022 [updated 20 May 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Richter DC, Joubert JR, Nell H, Schuurmans MM, Irusen EM (2008) Diagnostic value of post-bronchodilator pulmonary function testing to distinguish between stable, moderate to severe COPD and asthma. Int J Chronic Obstr Pulm Dis 3(4):693
Heussel C, Herth F, Kappes J, Hantusch R, Hartlieb S, Weinheimer O et al (2009) Fully automatic quantitative assessment of emphysema in computed tomography: comparison with pulmonary function testing and normal values. Eur Radiol 19(10):2391–2402
Nambu A, Zach J, Kim SS, Jin G, Schroeder J, Kim Y-I et al (2018) Significance of low-attenuation cluster analysis on quantitative CT in the evaluation of chronic obstructive pulmonary disease. Korean J Radiol 19:139–146
Murray CJ, Lopez AD (1996) Evidence-based health policy–lessons from the Global Burden of Disease Study. Science 274(5288):740–743
Lynch DA, Al-Qaisi ML (2013) Quantitative Ct in copd. J Thorac Imaging 28(5):284
Fan L, Zhou X, Xia Y, Guan Y, Zhang D, Li Z et al (2019) Progress in the imaging of COPD: quantitative and functional evaluation. Chin J Acad Radiol 1:1–6
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338
Launois C, Barbe C, Bertin E, Nardi J, Perotin J-M, Dury S et al (2012) The modified Medical Research Council scale for the assessment of dyspnea in daily living in obesity: a pilot study. BMC Pulm Med 12:61
Jiménez-Ruiz CA, Masa F, Miravitlles M, Gabriel R, Viejo JL, Villasante C et al (2001) Smoking characteristics: differences in attitudes and dependence between healthy smokers and smokers with COPD. Chest 119(5):1365–1370
Anazawa R, Kawata N, Matsuura Y, Ikari J, Tada Y, Suzuki M et al (2019) Longitudinal changes in structural lung abnormalities using MDCT in COPD with asthma-like features. Eur Respir Soc. https://doi.org/10.1371/journal.pone.0227141
Kumar I, Verma A, Jain A, Agarwal S (2018) Performance of quantitative CT parameters in assessment of disease severity in COPD: a prospective study. Indian J Radiol Imaging 28(01):99–106
Ostridge K, Wilkinson TM (2016) Present and future utility of computed tomography scanning in the assessment and management of COPD. Eur Respir J 48:216–228
Tanabe N, Muro S, Hirai T, Oguma T, Terada K, Marumo S et al (2011) Impact of exacerbations on emphysema progression in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 183(12):1653–1659
Madani A, Zanen J, De Maertelaer V, Gevenois PA (2006) Pulmonary emphysema: objective quantification at multi–detector row CT—comparison with macroscopic and microscopic morphometry. Radiology 238(3):1036–1043
Brillet P-Y, Fetita CI, Saragaglia A, Brun A-L, Beigelman-Aubry C, Prêteux F et al (2008) Investigation of airways using MDCT for visual and quantitative assessment in COPD patients. Int J Chronic Obstr Pulm Dis 3:97
Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M et al (2000) Computed tomographic measurements of airway dimensions and emphysema in smokers: correlation with lung function. Am J Respir Crit Care Med 162(3):1102–1108
Dransfield MT, Huang F, Nath H, Singh SP, Bailey WC, Washko GR (2010) CT emphysema predicts thoracic aortic calcification in smokers with and without COPD. COPD J Chronic Obstr Pulm Dis 7(6):404–410
Gietema HA, Zanen P, Schilham A, van Ginneken B, van Klaveren RJ, Prokop M et al (2010) Distribution of emphysema in heavy smokers: impact on pulmonary function. Respir Med 104:76–82
Pauls S, Gulkin D, Feuerlein S, Muche R, Krüger S, Schmidt SA et al (2010) Assessment of COPD severity by computed tomography: correlation with lung functional testing. Clin Imaging 34(3):172–178
Tsushima K, Sone S, Fujimoto K, Kubo K, Morita S, Takegami M et al (2010) Identification of occult parechymal disease such as emphysema or airway disease using screening computed tomography. COPD J Chronic Obstr Pulm Dis 7(2):117–125
Yamashiro T, Matsuoka S, Bartholmai BJ, Estépar RSJ, Ross JC, Diaz A et al (2010) Collapsibility of lung volume by paired inspiratory and expiratory CT scans: correlations with lung function and mean lung density. Acad Radiol 17(4):489–495
Grydeland TB, Thorsen E, Dirksen A, Jensen R, Coxson HO, Pillai SG et al (2011) Quantitative CT measures of emphysema and airway wall thickness are related to DLCO. Respir Med 105(3):343–351
Hoesein FAM, de Hoop B, Zanen P, Gietema H, Kruitwagen CL, van Ginneken B et al (2011) CT-quantified emphysema in male heavy smokers: association with lung function decline. Thorax 66(9):782–787
Mets O, Murphy K, Zanen P, Gietema H, Lammers J, Van Ginneken B et al (2012) The relationship between lung function impairment and quantitative computed tomography in chronic obstructive pulmonary disease. Eur Radiol 22:120–128
Timmins SC, Diba C, Farrow CE, Schoeffel RE, Berend N, Salome CM et al (2012) The relationship between airflow obstruction, emphysema extent, and small airways function in COPD. Chest 142(2):312–319
Wilson DO, Weissfeld JL, Balkan A, Schragin JG, Fuhrman CR, Fisher SN et al (2008) Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med 178(7):738–744
Nakajima T, Sekine Y, Yamada Y, Suzuki H, Yasufuku K, Yoshida S et al (2009) Long-term surgical outcome in patients with lung cancer and coexisting severe COPD. Thorac Cardiovasc Surg 57(06):339–342
Fan A, Grave E, Joulin A. Reducing transformer depth on demand with structured dropout. https://arxiv.org/abs/1909.11556 (2019).
Mishima M, Hirai T, Itoh H, Nakano Y, Sakai H, Muro S et al (1999) Complexity of terminal airspace geometry assessed by lung computed tomography in normal subjects and patients with chronic obstructive pulmonary disease. Proc Natl Acad Sci 96(16):8829–8834
Gietema HA, Müller NL, Fauerbach PVN, Sharma S, Edwards LD, Camp PG et al (2011) Quantifying the extent of emphysema: factors associated with radiologists’ estimations and quantitative indices of emphysema severity using the ECLIPSE cohort. Acad RADIOL 18(6):661–671
Acknowledgements
Not applicable
Funding
Funding of this research was supplied by local institutional fund and no outside industrial fund was received.
Author information
Authors and Affiliations
Contributions
All authors contributed sufficiently to the present study & all authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients provided written informed consent for the current study authorized by the regional institutional ethics committee before taking any data or doing any investigations or imaging techniques.
Consent for publication
Institutional consent form was applied to each participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saad, M.M., Bayoumy, A.A., EL-Nisr, M.M. et al. Assessment of artificial intelligence-aided chest computed tomography in diagnosis of chronic obstructive airway disease: an observational study. Egypt J Radiol Nucl Med 54, 97 (2023). https://doi.org/10.1186/s43055-023-01043-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01043-8