Abstract
Background
Whole-body diffusion-weighted magnetic resonance is being developed as a tool for assessing tumor spread. Patients with known primary tumors require meticulous evaluation to assess metastasis for better staging; we attempted to detect bony metastasis without radiation exposure. Our study's goal was to use whole-body diffusion-weighted imaging with background body signal suppression (WB-DWBIS) to evaluate bony metastasis in confirmed patients who have primary tumors.
Results
Our study included 90 patients with known primary cancer, 10 patients were excluded as they had no bony metastasis, from 80 patients: 36 (45.0%) having one site of metastasis, 36 (45%) having two sites of metastasis, and 8 (10.0%) having three sites of metastasis. 56 (70.0%) of the metastasis sites were bony metastasis, and 76 were mixed both bony and non-bony, including 32(40.0%) lung, 16 (20.0%) liver, and 28 (35%) lymph nodes. Sensitivity of bone scanning in detecting metastasis was as follows: 95.1% sensitivity and 92.0% accuracy, while that of whole-body diffusion-weighted image with background signals suppression was 94.8% sensitivity and 91.7% accuracy, WB-DWBIS inter-observer agreement in the detection of bony metastatic deposits in cancer patients was good (0.7 45, agreement = 93.2%).
Conclusions
Using WB-DWBIS images, bone lesion identification and characterization (site and number) were improved, producing outcomes similar to bone scanning without the use of ionizing radiation.
Similar content being viewed by others
Background
A viable malignant tumor exhibits high signal intensity on diffusion weighted image (DWI) because of its high cellularity, where water movement in tissues is constrained, which is different from conventional MRI in that it measures water mobility within tissues to generate contrast in images. An increasing number of studies indicate that this distinctive DWI signal can be used as an imaging biomarker to describe the pathophysiology of malignant tumors. With the aid of DWI, the reader can quickly identify cancerous tissue and gather descriptive data about the lesion. The evaluation of pathological conditions across the body is made easier by WB-DWBIS [1].
Early detection of metastasis in cancer patients is an essential step for timely management and a positive outcome. Extra-osseous metastasis can affect the liver, lung, and lymph nodes, while osseous metastasis can be spinal or appendicular [2,3,4,5]. Different imaging modalities are used for the detection of osseous and extra-osseous metastasis. The imaging techniques used for cancer patient staging varied depending on the local expertise and availability. The detection of osseous metastases is done using whole-body imaging. Due to false negatives and low sensitivity of some studies, they cannot be ruled out by various imaging modalities [4,5,6]
Diffusion-weighted imaging, which provides useful functional information about tumor cellularity, could easily be added to conventional imaging. Diffusion-weighted imaging is used because malignant tumors exhibit restricted diffusion and have higher cellular densities than normal tissue. Diffusion-weighted magnetic resonance imaging (MR) is used to evaluate osseous lesions as well as other lesions like liver, breast, and chest tumors as well as soft and bony tissue [7,8,9,10]. The use of whole-body MR imaging with diffusion-weighted imaging for the detection of metastases has recently attracted increasing interest [9, 10]. Whole-body MR imaging has been significantly enhanced by the introduction of the diffusion-weighted imaging with background body signal suppression (WB-DWBIS) technique [9,10,11,12]. The potential use of whole-body diffusion-weighted imaging (WB-DWBIS) with background body signal suppression for the detection of cancer has not been extensively studied.
WB-DWI was widely used in oncology [13].The currently accepted uses of WB-DWI are in the diagnosis and follow-up of lymphoma patients [14].It is also utilized to identify chemotherapy side effects in lymphoma patients [15].WB-DWI was widely utilized in TMN staging and the Metastasis Reporting and Data System for Prostate Cancer for lymph nodes (regional and non-regional), bone, and visceral metastases [16]. Moreover, multiple myeloma patients were diagnosed, monitored, and managed extensively using WB-DWI [17].
The fact that we evaluated bony metastases in cancer patients and comparing the result with bone scanning is a distinctive feature of our work together with lack of ionizing radiation and contrast media or isotope injection.
Our study's objective was to evaluate bony metastasis in confirmed patients with primary tumors (either by pathology or by other imaging modalities) using whole-body diffusion-weighted imaging with background body signal suppression (WB-DWIBS).
Methods
Our prospective non-randomized study was conducted between January 2019 and February 2022 at Radiodiagnosis and medical imaging department. Our study included 90 patients, of whom 10 were found to have non-bony metastasis and were excluded from the study. There was no preference based on gender or age. The study was approved by our university ethical committee. Written authorization and an extensive medical history were obtained. Patients with primary neoplasm volunteered for the MR scan and were able to understand and sign an informed consent informing them that: The examination was not required but may help to understand or stage their disease in future; the study required no contrast media injection; the study lasted 40 min; and no ionizing radiation would be used. They had no contraindications to MRI as certified by the specific MRI questionnaire. We excluded patients that were subjected to previous chemo or radiotherapy, patients with non-metastatic neoplasm, brain Aneurysm Clips, implanted cardiac pacemaker or defibrillator, Cochlear implant or any other MRI contraindications. The patients were prepared for the MRI study; every patient changed to MR gown and removed any clothing with any metal before the examination. The primary malignant tumors are distributed in Table 1
All examinations were performed on closed superconductive 1.5 T magnet (MAGNETOM Aera, Siemens Healthcare and GE), body coil was used, with the patient positioned feet first on an extended anatomical coverage table based on “rolling-table” technology.
WB-DWIBS was collected using the T2WI STIR (short inversion-time inversion recovery) fat suppression method. DWIBS was done in the axial plane with a 7-mm slice thickness and the following parameters: diffusion gradient encoding in three orthogonal directions; b value = 0 and 1000 s/mm2; TR/TE/flip angle, 3500–4500/60/95; field of view, 360-mm; matrix size, 512,512. For DWIBS, each patient required 4–5 positions to scan the entire body. Each position took about 4 min, and 4–5 positions were repeated, with T1WI of anatomical images added for image superposition. GRAPPA parallel imaging (generalized autocalibrating partially parallel acquisitions) was used in DWI/DWIBS. In DWIBS, the receiver bandwidth of the EPI readout was 2488 (Hz/Pixel). Each DWI slice was taken six times to determine the average. The total examination time was approximately 30–45 min. DWIBS were done in axial plane for three separate areas: 1—head, neck, chest and proximal upper limb 2—chest, abdomen, upper limb, and dorso-lumber spine; 3—pelvis, thighs, femur, knee joint, and proximal tibia, axial images were reconstructed on a coronal plane for each part and fused to reach to the final coronal DWI images.
Acquired images were bound to each other using post-processing software (the workstation SYNGO MR E11). The WB-DWIBS image sequence was independently reviewed by two radiologists with more than ten years of experience in MRI imaging. The bone scanning was reported by a nuclear medicine physician with 20 years’ experience. The radiologists were completely blinded to the clinical information and outcomes of bone scanning. Only WB-DWIBS images were reviewed and compared by findings of a bone scan by another two radiologists with more than five years of MRI expertise, and the results resulted in consensus. Images analyzed in different settings at different times. The goal of image interpretation was to find osseous metastases. Every site of abnormal or focal increase in signal intensity on WB-DWIBS images and showed diameter more than 1 cm and restricted diffusion on DWI that did not correspond to a normal anatomic structure or that experienced an unexpected increase in signal intensity was regarded as positive for bony metastases [18].
All data were acquired during free breathing. No contrast agent applied. The reference standard for comparing the finding was the bone scanning.
Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, and standard deviation, median and interquartile range (IQR). Significance of the obtained results was judged at the 5% level. Chi-square test was used for categorical variables, to compare between different groups and Fisher’s Exact was used for correction for chi-square when more than 20% of the cells have expected count less than 5. Cohen's kappa coefficient was used (0.00–0.20 poor agreement; 0.21–0.40 fair; 0.41–0.60 moderate; 0.61–0.80 good; 0.81–1.00 excellent), to assess the inter-observer agreement in WB-DWIBS interpretation, and to compare WB-DWIBS, DWI,and bone scanning as a reference standard; a p value of 0.05 was considered statistically significant.
Results
Our study included eighty patient with known primary cancer; Breast cancer 16/80(20.0%), Prostatic tumor 12/80(15.0%), Lymphoma 8/80(10.0%), Pancreatic tumor8/80(10.0%), Osteosarcoma 4/80(5.0%), Rectal carcinoma 4/80(5.0%), Bronchogenic carcinoma 4/80(5.0%), Anorectal carcinoma 4/80(5.0%), Endometrial carcinoma 4/80(5.0%), Ovarian tumor 4/80(5.0%), Psoas m. mass 4/80(5.0%), Cervical tumor 4/80(5.0%), hepatocellular carcinoma 4/80(5.0%), with 36 (45.0%) having one bony site of metastasis, 36 (45%) having two bony sites of metastasis, and 8 (10.0%) having three or more bony sites of metastasis. 56 (70.0%) of the metastasis sites were bony, and 76 were mixed of both bony and non-bony, including 32 (40.0%) lung, 16 (20.0%) liver, and 28 (35%) LNs (Figs. 1, 2, 3).
A female patient, 52 years old with a history of breast cancer, was sent to the MRI unit for a follow-up. A: Axial DWI at the level of the liver showed multiple restricted hepatic focal lesions. B Axial DWI at the iliac crest revealed a right iliac crest restricted lesion. C A coronal cut of whole-body diffusion with short tau inversion recovery revealed multiple hepatic focal lesions as well as a right iliac bony lesion (blue arrow) (metastatic). D: Coronal WBDWMS showed a right iliac bony lesion, multiple variable-sized hepatic focal lesions that appeared to have high signal intensity (restricted diffusion), and the right scapula (red arrow), which also showed a focal area of high signal intensity (restricted diffusion)
A 48-year-old male patient with a known history of osteosarcoma of the left femur was sent for a metastatic workup. A A DWI axial cut at the level of the chest shows a left humeral head bony lesion with high signal intensity (orange arrow); B A DWI axial cut at the level of the sacrum shows high signal intensity at the first sacral vertebra (metastases) (red arrow); C A WBDW MRI coronal cut with short tau inversion recovery showed high SI (restricted diffusion) at the left femur and another similar lesion at the right femur
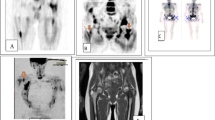
A Axial cuts of MRI DWI at the level of the chest show right and left sided bony lesions with high signal intensity (restricted diffusion) (white arrow); B axial cuts at the level of the chest show a hyperintense area at the dorsal vertebrae (white arrow), C coronal cuts of whole-body diffusion MRI WBDWI with background signal suppression reveal a right humeral head bony lesion, a right femoral bony lesion, and a dorsal vertebrae bony lesion (black arrows), as well as multiple ribs with focal areas of restricted diffusion (blue arrows)
The pathological subtypes of the cases studied were 36 (45.0%) adenocarcinoma, 16 (20%) squamous cell carcinoma, twelve patients with intraductal carcinoma, eight (10.0%) Hodgkin lymphoma, four patients with lobular carcinoma, and four patients with osteoblastic carcinoma.
Table 2 demonstrated WB-DWBIS inter-observer agreement in the detection of bony deposits in cancer patients was good (0.7 45, agreement = 93.2%).
The diagnostic parameters of conventional MRI were: 90.5%, 71.2%, 90.2%, 62.8% and 89.8%. The DWI were: 89.9%, 71.0%, 89.9%, 62.3%, and 89.25%, while that of WBDWSI were: 94.8%, 76.2%, 92.8%, 66.1%, and 91.7% (Sensitivity%, Specificity %, PPV%, NPV% and accuracy %, respectively) as discussed in Table 2.
Discussion
The results of this pilot study showed that WB-DWBIS could be used to detect bony metastasis. WB-DWBIS enabled more precise identification of the primary tumor site and more accurate detection of bony metastasis comparable to bone scan, conventional MRI and DWI with an excellent inter-observer agreement (k = 0.827).
As this study considered as preliminary study in our institution. It included a diverse group of patients with various pathologies; each pathology was represented by a small number of patients. This study attempted to compare the conventional MRI, DWI and WB-DWIBS with bone scanning with the goal of early detection of site and number of bony metastasis with reduced cost and radiation of bone scan, which also reduces the risk of radiation as cancer patients require successful imaging as routine follow-up and in pregnant patients. This technique uses no contrast injection and is therefore suitable for patients with renal impairment.
The overall sensitivity of the WB-DWIBS when compared to other imaging diagnostic modalities was nearly the same of bone scan and more accurate than conventional MRI and DWI, while combined WB-DWIBS, DWI and conventional T1 WI carried more accuracy (92.8%) in detection of bone metastasis compared to bone scan as shown in Table 2
The inter-observer agreement in WB-DWIBS interpretation was excellent, with a K = 0.827. The two readers were discordant in just two out of 80 cases, in which one of the radiologists missed the vertebral locations of the disease.
The inter-observer agreement of conventional T1WI was moderate K = 0.499, while that of DWI was good K = 0.612, and of combined with WB-DWIBS was excellent (slightly higher than each technique alone K = 0.899.
Many studies cleared out the role of DWI in detection of metastasis, but few studies discussed the role of WB-DWIBS as promising imaging tool in diagnosis of bony metastasis.
Our study also matched with the study of Wenping et al. [19], who study a total of 213 metastatic bone segments among 39 patients combined with their ADC values. They found the sensitivity, specificity, overall accuracy, positive predictive value, and negative predictive value were 93.0%, 87.8%, 89.6%, 79.8%, and 96.0%, respectively, for WB DWIBS. They concluded that WB-DWIBS coupled with ADC analysis at 3 T was effective for detecting bone metastases.
WB-DWIBS findings in our study had 94.8%, 76.2%, 92.8%, 66.7%, 92.8% sensitivity, specificity, overall accuracy, positive predictive value, and negative predictive value with higher accuracy when combined WB-DWIBS, T1WI, and DWI. These findings were helpful in proper staging of cancer patients with advantage of reconstructed multi-planar images, faster interpretation and easier visual assessment. This technique employed free breathing, allowing for thin axial section acquisition and multiple signal averaging, as well as fat suppression, which highlighted areas of diffusion restriction [20].
WB-DWIBS was used in our study to diagnose bony metastasis of breast, prostate, lymphoma, pancreatic, osteosarcoma, rectal, bronchogenic, anorectal, endometrial, ovarian, psoas muscle mass, cervical, and HCC. This finding matched with Alessandro et al. [21] who stated that WB-DWI seemed to be a promising method of imaging in the detection of bony metastases.
Eighty percent of bone metastases are caused by primary tumors of the prostate, breast, and lung. Whole-body bone imaging is frequently required in cancer management for these patients, and the use of WB-DWI is increasingly used [22].
Nakanishi et al. [23] who studied the role of WB-DWIBS in diagnosis of bony metastasis form prostatic cancer, he asserted that WB-MRI was the most reliable technique for detecting prostate cancer bony metastasis. It offered the benefit of detecting lesions that were missed by traditional imaging modalities like CT and BS. It could also be used to monitor the effectiveness of treatments due to its repeatability.
Few studies compared WB-DWI with PET/CT in diagnosis of bone marrow infiltration in patients with lymphoma, they concluded that the WB-MRI and FDG-PET/CT were useful techniques to evaluate bone marrow infiltration, and that WB-MRI is a non-invasive approach which did not require radiation exposure or the administration of contrast. It could be used as a guide for BMB in suspected cases, avoiding dangerous false negative samplings [24, 25].
Our study results matched with Michael A. Jacobs et al. [26] who confirmed that WB-MRI is useful for oncologic staging to identify bony and visceral metastasis in breast, prostate, pancreatic, and colorectal cancers. WB-MRI can be developed for a comprehensive evaluation for staging and response during treatment.
Our study's limitations included a small sample size and a long time of examination; we recommended further study comparing PET-CT as golden imaging modality with WB-DWIBS.
Conclusions
WB-DWIBS is a promising tool for oncology patients' tumor surveillance and metastatic workup, with excellent diagnostic accuracy in detecting bony metastatic lesions. It is a viable option for single-step non-invasive cancer staging with good reader reproducibility, and it improves the efficacy of standard imaging techniques for locating metastases, particularly with frequent follow-up.
Availability of data and materials
All data generated or analyzed during our study are included in this published article.
Abbreviations
- WBDWIBS:
-
Whole-body diffusion-weighted image with background signal suppression
- TSE:
-
Turbo spin echo
- STIR:
-
Short tau inversion recovery
- PET-CT:
-
Positron emission tomography
- DWI:
-
Diffusion weighted image
- WB-DWI:
-
Whole-body diffusion-weighted imaging
References
Yoshida S, Takahara T, Arita Y et al (2021) Whole-body diffusion-weighted magnetic resonance imaging: diagnosis and follow up of prostate cancer and beyond. Int J Urol 28(5):502–513. https://doi.org/10.1111/iju.14497. (PMID: 33676376)
Bezerra ROF, Recchimuzzi DZ, Dos Santos Mota MM et al (2019) Whole-body magnetic resonance imaging in the oncology setting: an overview and update on recent advances. J Comput Assist Tomogr 43:66–75. https://doi.org/10.1097/RCT.0000000000000772
Barnes A, Alonzi R, Blackledge M et al (2018) UK quantitative WB-DWI technical workgroup: consensus meeting recommendations on optimisation, quality control, processing and analysis of quantitative whole-body diffusion-weighted imaging for cancer. Br J Radiol 91:20170577. https://doi.org/10.1259/bjr.20170577
Morone M, Bali MA, Tunariu N et al (2017) Whole-body MRI: current applications in oncology. AJR Am J Roentgenol 209:W336-349. https://doi.org/10.2214/AJR.17.17984
Han SN, Amant F, Michielsen K et al (2018) Feasibility of whole-body diffusion-weighted MRI for detection of primary tumour, nodal and distant metastases in women with cancer during pregnancy: a pilot study. Eur Radiol 28:1862–1874. https://doi.org/10.1007/s00330-017-5126-z
Petralia G, Padhani AR, Pricolo P et al (2019) Whole-body magnetic resonance imaging (WB-MRI) in oncology: recommendations and key uses. Radiol Med 124:218–233. https://doi.org/10.1007/s11547-018-0955-7
Razek AA (2012) Diffusion magnetic resonance imaging of chest tumors. Cancer Imaging 12:452–463. https://doi.org/10.1102/1470-7330.2012.0041
Razek AA, Gaballa G, Denewer A et al (2010) Diffusion weighted MR imaging of the breast. Acad Radiol 17:382–386. https://doi.org/10.1016/j.acra.2009.10.014
Lecouvet FE (2016) Whole-body MR imaging: musculoskeletal applications. Radiology 279:345–365. https://doi.org/10.1148/radiol.2016142084
Koh DM, Blackledge M, Padhani AR et al (2012) Whole-body diffusion- weighted MRI: tips, tricks, and pitfalls. AJR Am J Roentgenol 199:252–262. https://doi.org/10.2214/AJR.11.7866
Padhani AR, Koh DM, Collins DJ (2011) Whole-body diffusion-weighted MR imaging in cancer: current status and research directions. Radiology 261:700–718. https://doi.org/10.1148/radiol.11110474
Kwee TC, Takahara T, Ochiai R et al (2008) Diffusion-weighted whole-body imaging with background body signal suppression (DWIBS): features and potential applications in oncology. Eur Radiol 18:1937–1952. https://doi.org/10.1007/s00330-008-0968-z
Albano D, Stecco A, Micci G et al (2021) Whole-body magnetic resonance imaging (WB-MRI) in oncology: an Italian survey. Radiol Med 126(2):299–305. https://doi.org/10.1007/s11547-020-01242-7. (Epub 2020 Jun 22 PMID: 32572763)
Galia M, Albano D, Tarella C et al (2018) Whole body magnetic resonance in indolent lymphomas under watchful waiting: the time is now. Eur Radiol 28:1187–1193. https://doi.org/10.1007/s00330-017-5071-x
Albano D, Patti C, La Grutta L et al (2017) Osteonecrosis detected by whole body magnetic resonance in patients with Hodgkin Lymphoma treated by BEACOPP. Eur Radiol 27:2129–2136. https://doi.org/10.1007/s00330-016-4535-8
Padhani AR, Lecouvet FE, Tunariu N et al (2017) METastasis reporting and data system for prostate cancer: practical guidelines for acquisition, interpretation, and reporting of whole-body magnetic resonance imaging-based evaluations of multiorgan involvement in advanced prostate cancer. Eur Urol 71(1):81–92. https://doi.org/10.1016/j.eururo.2016.05.033
Meletios AD, Jens H, Saad U et al (2015) Role of magnetic resonance imaging in the management of patients with multiple myeloma: a consensus statement. J Clin Oncol 33(6):657–664. https://doi.org/10.1200/JCO.2014.57.9961
Albano D, Patti C, La Grutta L et al (2016) Comparison between whole-body MRI with diffusion-weighted imaging and PET/CT in staging newly diagnosed FDG-avid lymphomas. Eur J Radiol 85(2):313–318. https://doi.org/10.1016/j.ejrad.2015.12.006]
Wenping S, Sun M, Yifeng G et al (2020) Diagnostic value of whole-body DWI with background body suppression plus calculation of apparent diffusion coefficient at 3 T versus 18F-FDG PET/CT for detection of bon metastasis. AJR 214:446–454
Manenti G, Cicciò C, Squillaci E et al (2012) Role of combined DWIBS/ 3D-CE-T1w whole-body MRI in tumor staging: comparison with PET-CT. Eur J Radiol 81:1917–1925. https://doi.org/10.1016/j.ejrad.2011.08.005
Alessandro S, Alessandra T, Eleonora Soligo S (2018) Whole-body MRI with diffusion-weighted imaging in bone metastases: a narrative review. Diagnostics 8(3):45. https://doi.org/10.3390/diagnostics8030045
DeSouza NM, Liu Y, Chiti A, Oprea-Lager D et al (2018) Strategies and technical challenges for imaging oligometastatic disease: recommendations from the European organisation for research and treatment of cancer imaging group. Eur J Cancer 91:153–163
Nakanishi K, Tanaka J, Nakaya Y et al (2022) Whole-body MRI: detecting bone metastases from prostate cancer. Jpn J Radiol 40(3):229–244. https://doi.org/10.1007/s11604-021-01205-6. (Epub 2021 Oct 25. PMID: 34693502; PMCID: PMC8891104)
Albano D, Patti C, Lagalla R et al (2017) Whole-body MRI, FDG-PET/CT, and bone marrow biopsy, for the assessment of bone marrow involvement in patients with newly diagnosed lymphoma. J Magn Reson Imaging 45:1082–1089. https://doi.org/10.1002/jmri.25439
Adams HJA, Kwee TC, Vermoolen MA et al (2013) Whole-body MRI for the detection of bone marrow involvement in lymphoma: prospective study in 116 patients and comparison with FDG-PET. Eur Radiol 2013(23):2271–2278. https://doi.org/10.1007/s00330-013-2835-9
Jacobs MA, Macura KJ, Zaheer A, Antonarakis ES et al (2018) Multipara metric whole-body MRI with diffusion-weighted imaging and ADC mapping for the identification of visceral and osseous metastases from solid tumors. Acad Radiol 25(11):1405–1414. https://doi.org/10.1016/j.acra.2018.02.010
Acknowledgements
Staff member of Tanta University hospital especially radiology department.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
HT correlated the study concept and design and had the major role in analysis. SA collected data in all stage of manuscript and performed data for analysis. RA supervised the study with significant contribution to design the methodology, manuscript revision and preparation, and NM correlated the finding with clinical finding and managed the cases. All authors have and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consents taken from the patients; the study approved from ethical committee of faculty of medicine Tanta University number 18/1/32042.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eltonbary, H.T.A.I., Elmashad, N.M., Khodair, S.A. et al. Suppression of background body signals in whole-body diffusion-weighted imaging for detection of bony metastases: a pilot study. Egypt J Radiol Nucl Med 54, 65 (2023). https://doi.org/10.1186/s43055-023-01012-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01012-1