Abstract
Background
The first description of right pulmonary artery-to left atrium communication was done by Friedlich and coauthors in 1950. The right pulmonary artery and left atrium are directly connected by the right pulmonary artery to left atrial fistula through a thin-walled aneurysm. Here, we describe a female adult patient who underwent investigation for dyspnea and had Type 1 right pulmonary artery to left atrium connection.
Case presentation
Twenty-two-year-old female presented with history of breathlessness (New York Heart association classification grade III) for 3 years. On initial examination, her saturation was 60% with no clinical evidence of cyanosis. Initial radiographic examination and CT pulmonary angiogram revealed a dilated communication between the right inferior pulmonary artery and left atrium. The patient was then referred for cardiac MRI. The MR imaging showed the following findings: Dilated right ventricle and atrium with Ostium secundum type of atrial septal defect. Large focal outpouching was noted arising from the right inferior pulmonary artery whose inferomedial portion appeared to communicate with left atrium. The final diagnosis was right pulmonary artery to left atrial fistula-Type I with ostium secundum type atrial septal defect. Midline sternotomy was performed for ligation of this fistula with septal correction. Post surgery, patient began to improve clinically and her saturation in room air increased to 92%
Conclusions
Right pulmonary artery to left atrial fistula is different from the pulmonary AV fistula and its rarity directs the need for imaging to diagnose the condition and for management selection. The fistulous connection, which most frequently originates from the posterior wall of the descending branch of RPA and inserts into the LA, is readily seen on CT/catheter angiography. Due to the rarity of this entity and much fewer evidences in imaging, we have reported a type 1 right pulmonary artery to left atrium connection.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The first description of right pulmonary artery-to left atrium communication was done by Friedlich and coauthors in 1950 [1]. The right pulmonary artery and left atrium are directly connected by the right pulmonary artery to left atrial fistula through a thin-walled aneurysm. They act as direct right-to-left shunts resulting in central cyanosis, clubbing, exertional dyspnea and polycythemia. Bypassing the pulmonary filtration process also results in passage of emboli and bacteria to the systemic circulation causing stroke, cerebral abscess, cerebral and systemic emboli.
De Souza e Silva et al. [2] categorized three types of communications based on the presence or absence of an aneurysm in the fistula and on the anatomy of pulmonary venous drainage pattern.
-
Type I is a normal pulmonary venous pattern
-
Type II is an absent right inferior pulmonary vein with fistulous connection at the normal site of its ostium
-
Type III is when all the pulmonary veins are connected to the aneurysmal pouch.
The fourth type was later added by Ohara et al. [3].
-
Type IV is a right inferior pulmonary vein replaced by three small veins connected to the aneurysmal pouch. The left-sided pulmonary veins join the left atrium directly
Case presentation
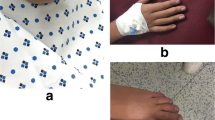
Twenty-two years old female presented with history of breathlessness (New York Heart association classification grade III) for 3 years. On initial examination, her saturation was 60% with no clinical evidence of cyanosis. Initial radiographic examination revealed a right hilar mass with no other significant changes in bilateral lung fields (Additional file 1: Fig 1). CT pulmonary angiogram performed in GE Optima CT 660 SE 128 CT scanner for the evaluation of the right hilar mass revealed a dilated communication between the right inferior pulmonary artery and left atrium (Additional file 1: 2, 3, 4). The patient was then referred for cardiac MRI. The magnetic resonance imaging was performed in 3 T magnetic resonance scanner (Siemens Healthineers, Erlangen, Germany). Standard institute cardiac MR protocol with TRUFISP (white blood) images and HASTE (dark blood) axial and coronal sections was done for morphologic imaging. The MR imaging showed the following findings: dilated right ventricle and atrium with Ostium secundum type of atrial septal defect measuring approximately 16.3 mm. Large focal outpouching was noted arising from the right inferior pulmonary artery whose inferomedial portion appeared to communicate with left atrium which was responsible for the right-to-left shunting and hypoxia. The diameter of the communication measures 23 mm (Additional file 1: Fig 5, 6). The final diagnosis was right pulmonary artery to left atrial fistula-Type I with ostium secundum type of septal defect. Midline sternotomy was performed for ligation of this fistula with septal correction. After surgery, the condition of the patient got better.
Discussion
Patients present with symptoms right from infancy to late adulthood. Those who present later have a milder clinical course than those who present in infancy [4]. The following symptoms and signs combined point toward the diagnosis: central cyanosis, clubbing of fingers, exertional dyspnea, silent precordium, normally split second heart sound, nonspecific murmur over left or right axillary region, and an abnormal radiographic density in the right or left pulmonary hilum. Because of the rarity of this entity, the diagnosis by clinical symptoms and signs remain a remote possibility [5]. Hence, imaging plays a vital role in its identification. The referring physician requires its exact location and the type of the fistula for planning the management as it ranges from simple ligation to transcatheter closure of the fistula and also for deciding the requirement of extracorporeal circulation. Diagnosis of right pulmonary artery to left atrium communication is difficult. It was possible to diagnose this fistula on a contrast echocardiogram by filling an aneurysmal sac behind the left atrium and communicating to it after three beats of contrast filling to right-sided structures. This suggested right pulmonary artery to left atrium communication in this situation. The most conclusive method to validate this uncommon diagnosis and precisely delineate the anatomical characteristics is still cardiac catheterization with selective angiography. A precise diagnosis can also be made using high-resolution CT, which provides a clear image of cardiovascular features [6]. The fistulous connection, which most frequently originates from the posterior wall of the descending branch of RPA and inserts into the LA, is readily seen on CT angiography. The conventional course of treatment involves performing a median sternotomy to surgically ligate the aberrant connection. With this procedure, there is a high risk of severe trauma and several consequences, including aneurysmal communication rupture, systemic embolism, infective endarteritis, and cerebral abscess. For type I fistulas, straightforward ligation or division via median sternotomy seems appropriate. For type II fistulas, a right or left posterolateral thoracotomy may be the best option. Extracorporeal circulation may be more appropriate for treating type III and type IV fistulas when dissecting the abnormal artery is technically challenging or when complex intracardiac repairs are necessary. Additionally, isolated case reports of transcatheter fistula closure have been published [7]. Right pulmonary artery to left atrial fistula is different from the pulmonary AV fistula and its rarity [8] directs the need for imaging to diagnose the condition and for management selection. The fistulous connection, which most frequently originates from the posterior wall of the descending branch of RPA and inserts into the LA, is readily seen on CT/catheter angiography. To avoid prolonged arterial hypoxia, systemic thromboembolic consequences, congestive heart failure, shunt-derived pulmonary hypertension, and brain abscess, early surgical intervention is indicated.
Conclusions
Right pulmonary artery to left atrial fistula is different from the pulmonary AV fistula and its rarity directs the need for imaging to diagnose the condition and for management selection. The fistulous connection, which most frequently originates from the posterior wall of the descending branch of RPA and inserts into the LA, is readily seen on CT/catheter angiography. To avoid prolonged arterial hypoxia, systemic thromboembolic consequences, congestive heart failure, shunt-derived pulmonary hypertension, and brain abscess, early surgical intervention is indicated. Due to the rarity of this entity and much fewer evidences in imaging, we have reported a type 1 right pulmonary artery to left atrium connection with CT angiography and MR.
Availability of data and materials
Not applicable.
Abbreviations
- TRUFISP:
-
True fast imaging with steady state precession
- HASTE:
-
Half Fourier Single-shot Turbo spin-Echo
References
Friedlich A, Bing RJ, Blount SG Jr (1950) Physiological studies in congenital heart disease. IX. Circulatory dynamics in the anomalies of venous return to the heart including pulmonary arteriovenous fistula. Bull Johns Hopkins Hosp 86:20–57
de Souza e Silva NAS, Giuciani ER, Ritter DG, Davis GD, Pluth JR (1974) Communication between right pulmonary artery and left atrium. Am J Cardiol 34:857–863
Ohara H, Ito K, Kohguchi N et al (1979) Direct communication between the right pulmonary artery and the left atrium: a case report and review of the literature. J Thorac Cardiovasc Surg 77:742–747
Zeebregts CJ, Nijveld A, Lam J, van Oort AM, Lacquet LK (1997) Surgical treatment of a fistula between the right pulmonary artery and the left atrium: presentation of two cases and review of literature. Eur J Cardiothorac Surg 11:1056–1061
Krishnamoorthy K (2001) Pulmonary artery to left atrial fistula. Eur J Cardiothorac Surg 20:1052–1053
Zhu J, Xi EP, Yan M, Zhu SB (2015) Right pulmonary artery to left atrial fistula confirmed by 320-slice computerized tomography. Chin Med J 128:2549–2550
Zanchetta M, Rigatelli G, Pedon L et al (2003) Transcatheter Amplatzer duct occluder closure of direct right pulmonary to left atrium communication. Catheter Cardiovasc Interven 58:107–110
Chowdhury UK et al (2005) Right pulmonary artery to left atrium communication. Ann Thorac Surg 80:365–370
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Prof. Dr. BPS analyzed and interpreted the patient data regarding the clinical history and of the imaging modality. Dr. FN was the major contributor in data collection, literature search and writing the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient’s consent to publish was obtained before the publication.
Competing interests
The authors declare that we have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Right pulmonary artery to left atrial fistula.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Naghath, F., Sathyanathan, B.P. A rare case of pulmonary artery to left atrium fistula. Egypt J Radiol Nucl Med 54, 41 (2023). https://doi.org/10.1186/s43055-023-00986-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-00986-2