Abstract
Aim of study
To evaluate the role of diffuse tensor imaging (DTI) in detecting structural alterations following TBI with persistent symptoms without findings on conventional structural imaging.
Methods
This was a prospective study that enrolled a total of 30 individuals (12 females and 18 males), 6 control with no history of trauma and 24 with previous history of trauma. All subjects underwent conventional brain MRI and DTI. The eigenvalues of the genue and splenium of corpus callosum (CC), superior longitudinal fasciculus (SLF), inferior longitudinal fasciculus (ILF), corticospinal tract (CS), arcuate fasciculus (AF) were measured bilaterally in all cases using suitable region of interest and the fraction anisotropy (FA), mean diffusivity (MD), were calculated. FA and MD values were compared between patients and control subjects. Diagnostic accuracy was calculated for FA, MD and combined. Sensitivity and Specificity were determined from the curve and PPV, NPV and accuracy underwent calculation through cross-tabulation.
Result
As compared with controls, FA was significantly decreased and MD was significantly increased in genue and splenium of CC and CS. For the Combined FA & MD in differentiating cases with trauma there was statistically significant difference in SLF, AF, genue, splenium, ILF and CS as p value < 0.05.
Conclusions
DTI parameters is a promising tool in the detection of subtle brain parenchymal changes in patients with TBI who have persistent symptoms and no evident abnormalities on conventional MRI. Furthermore combined use of FA and MD shows better diagnostic accuracy in differentiation between control and trauma patient.
Similar content being viewed by others
Background
Over 27 million persons are affected by TBI (traumatic brain injury) worldwide annually. TBI usually results in cognitive and functional impairments, impaired daily life activities and poor quality of life [1]. Defects in attention, processing speed, memory, language, executive function, or other cognitive functions commonly occur as TBI sequelae [2].
In TBI patients, CT is often performed as the first radiological technique during the acute treatment. CT can be done rapidly, and it can detect the pathological changes which are essential for the early treatment of brain trauma, including hemorrhages, cerebral edema, and midline shift [3]. CT, however, has a limited role. Numerous studies demonstrated that magnetic resonance imaging (MRI) is better as compared with the CT in the detection of intraparenchymal traumatic lesions, both in the acute and chronic stages, and irrespective of injury severity, particularly brainstem and traumatic axonal injuries are much better visualized using MRI [4].
The pathological changes of DAI (diffuse axonal injury) after TBI include by diffuse axonal injury in brainstem, parasagittal white matter (WM) of cerebral cortex, and CC [5]. The most common DAI sites include CC, mainly the splenium, hemispheric WM, brainstem, as well as cerebellum. CT and MRI were shown to be associated with an underestimation of the extent of DAI after TBI [6, 7], thus the utilization of advanced MRI methods, like DTI, can detect white matter injury and its related symptoms after TBI [8, 9]. Significant evidence does exist regarding the susceptibility of WM bundles near the midline, including the fornix and cingulum, to shearing forces after TBI [10, 11].
DTI can qualitatively and quantitatively detect the pathological changes not visualized by other methods and is, thus, a significant tool in both the research and clinical settings [12], two DTI scalars—MD and FA characterize the degree of water diffusion and anisotropy, respectively, for each voxel. Furthermore, axial (parallel to long axis of fiber) and radial (perpendicular) diffusivity are given by corresponding eigenvector values [13, 14]. An alteration of DTI-based parameters in the subacute post-injury stage proposes different levels of WM injury [15, 16].
Our aim is to assess the role of DTI in the detection of structural changes following TBI with persistent symptoms without findings on conventional structural imaging.
Methods
The current study obtained its approval from the local ethics committee and an informed consent was taken from every participant. A total of 32 subjects were enrolled, 26 patients who had past history of head trauma and 6 control healthy subjects. The inclusion criteria were; (1) patients with past history of head trauma, (2) persistent symptoms, (3) no evident white matter abnormalities on conventional MRI. We excluded two patients from the study because one patient had cerebral contusions and corpus callosum abnormal SI and the other one showed multiple abnormal SI in WM. The final patients included were 24 patients (9 females and 15 males), and 6 control with no history of trauma. They were 5–52 years old (mean age = 26 years).
MRI technique
Technique was carried out by a 1.5 Tesla scanner (Ingenia, Philips). dStream HeadNeck 20 channel coil was used.
The next conventional MR sequences were used during the imaging:
2D sagittal T1-weighted spin-echo localizer (500/8/1 [TR/TE/excitations], 90° flip angle, 24_24-cm field of view [FOV], 256_256 imaging matrix, 20 sections, 5-mm section thickness with 1.5-mm skip). 2D axial T2-weighted multiplanar prepared gradient-recalled acquisition in the steady state (800/25/1, 20° flip angle, 22_22-cm FOV, 256_256 imaging matrix, 23 sections, 5-mm section thickness with 2-mm skip).2D axial T1-weighted spin-echo (500/8/1, 90° flip angle, 24_24-cm FOV, 256_256 imaging matrix, 20 sections, 5-mm section thickness with 1.5-mm skip).
DTI was carried out using a modified 2D spin-echo sequence, with an echo planar imaging acquisition window and a pair of diffusion gradients symmetrically positioned around the 180° radio-frequency pulse. The imaging parameters were 4500/71.8/1, 24_24-cm FOV, 21 contiguous sections, 3-mm section thickness.
Then images were taken to offline workstation for post-processing.
Post-processing
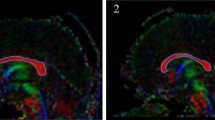
DICOM images underwent transfer to workstation (extended MR Workspace 2.6.3.5, Philips medical systems Nederland BV). At first, automated registration of DTI data was performed to remove eddy-current artifacts, after that fiber tracking advanced tools started. The eigenvalues (primary, secondary and tertiary) of the genue and splenium of CC, SLF, ILF, CS and AF were bilaterally measured using the appropriate region of interest and FA and MD, underwent calculation.
Statistical analysis
Data were analyzed by IBM SPSS Corp. Released 2013. IBM SPSS Statistics for Windows, V 22.0. Armonk, NY: IBM Corp. Qualitative data were represented as numbers and percents. Quantitative data were represented as means and standard deviations for parametric data and medians (min. and max.) for nonparametric data following testing normality by Kolmogrov–Smirnov test. Significance of results was set at the (0.05) level. Student t test was utilized for comparing two independent groups and Receiver Operating Characteristic (ROC) curve analysis, diagnostic precision ROC curve analysis is used to evaluate a test’s diagnostic performance or its ability to accurately distinguish between people with and without an illness. Cross-tabulation calculations were used to calculate PPV, NPV and accuracy while the ROC curve was used to estimate sensitivity and specificity.
Results
Twenty four patients with head trauma and 6 age- and gender-matched normal control subjects were enrolled in the study.
Baseline characteristics
The patient group consisted of 9 females and 15 males (median age 26, range 5–52 years) while the control group included 3 males and 3 females (median age 27, range 6–53 years) with no significant difference between both groups.
Patients came with history of head trauma from 3 days to one month. They were subjected for MRI brain with diffusion tensor imaging. According to the mode of trauma 15 patients (50%) came in road traffic accidents, 6 of them (20%) falling from height and 3 patients (10%) came in street fight. 30 subjects showed GCS (Glasgow Coma Scale) variation from 8 (sever traumatic brain injury) to 15 control cases and cases with mild trauma.
The conventional MR did not detect any abnormalities in controls. For the trauma group, 15 patients (62.5%) showed no abnormalities, while the other 9 cases (37.5%) showed abnormalities in the form of: 5 cases showed right subdural hemorrhage, subarachnoid hemorrhage seen in 3 cases, and one case showed small right parietal subgaleal hematoma; however, none of these nine cases showed evident white matter abnormalities on conventional MRI.
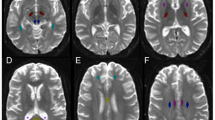
DTI parameters in TBI patients and control
A significant difference was sound between both groups in the measurement of means of FA and MD (10−3 mm2/s) in genue, splenium and CS as p value < 0.05 as demonstrated in Tables 1 and 2.The mean FA in genue of the trauma patients (0.52 ± 0.127on the right) and (0.516 ± 0.140 on the left) was significantly lower than the controls (0.7975 ± 0.07 on the right) and (0.771 ± 0.091 on the left), while the mean MD (0.809 ± 0.081 on the right) and (0.842 ± 0.111 on the left) was significantly greater compared with controls (0.407 ± 0.267 on the right) and (0.633 ± 0.07 on the left). Mean FA in the splenium of the trauma group (0.537 ± 0.151 on the right) and (0.544 ± 0.168 on the left) was significantly lower than controls (0.863 ± 0.06 on the right) and (0.858 ± 0.06 on the left) also the mean MD (0.836 ± 0.075 on the right) and (0.814 ± 0.082 on the left) was significantly greater compared to the control group (0.677 ± 0.065 on the right) and (0.630 ± 0.039 on the left). As regard to the CS the mean FA was significantly lower in the trauma group (0.524 ± 0.121 on the right) and (0.530 ± 0.116 on the left) than the control (0.671 ± 0.07 on the right) and (0.699 ± 0.076 on the left) the mean MD was significantly higher in trauma group (0.797 ± 0.094 on the right) and (0.803 ± 0.097 on the left) than the control group (0.669 ± 0.07on the right) and (0.639 ± 0.056 on the left) (Fig. 1).
Male patient aged 25 years old with trauma since 2 weeks came with drowsiness, came with GCS 15. No detected any abnormalities in conventional MRI images T2 and FLAIR (A and B). DTI image C of both genue and splenium of corpus callosum show affection of genue on right side mean FA less than 0.751 and ADC more than 0.706 and affection right side splenium as FA less than 0.82 and ADC more than 0.743
ROC curve analysis
At ROC curve for genue the AUC (Area under curve) of FA values utilized to differentiate trauma cases from control subjects were (0.944) on right side and (0.896) on left side with cutoff point (0.7505) on right side and (0.682) on left side. The sensitivity, specificity, PPV and NPV were (91.7%, 83.3%, 95.7%, 71.4%), respectively, on right side and (87.5%, 83.3%, 95.5%, 62.5%), respectively, on left side, as shown in Table 3 (Fig. 2). The AUC of MD values used to differentiate trauma cases from control subjects were (0.913) on right side and (0.979) on left side with cutoff point (0.706) on right side and (0.722) on left side. The sensitivity, specificity, PPV and NPV were (91.7%, 83.3%, 95.7%, 71.4%), respectively, on right side and (95.8%, 83.3%, 95.8%, 83.3%), respectively, on left side, as shown in Table 4 (Fig. 3).
For the splenium of corpus callosum, at ROC curve, the AUC of FA values utilized to differentiate trauma cases from control subjects were (0.972) on right side and (0.938) on left side with cutoff point (0.8152) on right side and (0.820) on left side. The sensitivity, specificity, PPV and NPV were (95.8%, 83.3%, 95.8%, 83.3%), respectively, on right side and (91.7%, 83.3%, 95.7%, 71.4%), respectively, on left side, as shown in Table 3 (Fig. 2).The AUC of MD values utilized to differentiate trauma cases from control subjects were (0.972) on right side and (0.958) on left side with cutoff point (0.743) on right side and (0.680) on left side. The sensitivity, specificity, PPV and NPV values were (91.7%, 83.3%, 95.7%, 71.4%), respectively, on right side and (91.7%, 83.3%, 71.4%, 90%), respectively, on left side, as shown in Table 4 (Fig. 3).
At ROC curve, the AUC of CS tract, the FA values used to differentiate trauma cases from controls were (0.854) on right side and (0.875) on left side with cutoff point (0.600) on right side and (0.646) on left side. The sensitivity, specificity, PPV and NPV were (79.2%, 83.3%, 95%, 50%), respectively, on right side and (83.3%, 66.7%, 90.9%, 50%), respectively, on left side, as demonstrated in Table 3 (Fig. 2). While the AUC of MD values used to differentiate trauma cases from controls were (0.882) on right side and (0.938) on left side with cutoff point (0.7065) on right side and (0.712) on left side. The sensitivity, specificity, PPV and NPV were (91.7%, 66.7%, 91.7%, 66.7%), respectively, on right side and (87.5%, 83.3%, 95.5%, 62.5%), respectively, on left side, as shown in Table 4 (Fig. 3).
For combined FA and MD, the AUC of genue and splenium was higher than individual FA and MD alone, while in CS combined FA and MD was slightly higher or might be near equal the individual FA and MD (Table 5) (Fig. 4).
Correlations between GCS and DTI parameters in trauma patients
There was significant negative association between GCS and combined FA and MD values in AF (r-0.434, p-value 0.017), ILF (r-0.463, p-value 0.010), as well as CS tract (rs-0.492, p-value 0.006). No correlations were found for combined FA and MD value with GCS in SLF, splenium and genue (Table 6).
Discussion
The key finding of the our study is altered DTI parameters in genue, splenium and CS tract in trauma patients and control, furthermore combined use of FA and MD showed better diagnostic accuracy in differentiation between trauma patients and control.
DTI is an advanced MRI that came into existence in the mid-1980s and is able to provide rich information on the brain’s neuroanatomical connectome [17, 18].
In normal brain, the degree of diffusion is restricted by the microstructural organization of white matter tracts [19]; leading to decreased MD/ADC values. However, this could be increased after a TBI because of injury/changes to the white matter microstructure, which previously reduced diffusion [15]. This concept was revealed in this study, as the mean MD demonstrated a statistically significant increase in the cases with TBI as compared with control subjects in the following regions; genu, splenium and CS (on both the right and left side) and of the SLF on the right side only.
Reduced FA (particularly at the anterior corona radiata, cingulum bundle, and e uncinate fasciculus) and increased MD values were found among TBI subjects indicating more isotropic (i.e., less limited) diffusion due to white matter injury and enhanced diffusion perpendicular to the predominant orientation of axonal fibers due to myelin injury [20]. Meanwhile, increased FA values and reduced MD values are detected in CC and many left-hemisphere tracts in semi-acute mTBI (mild traumatic brain injury) cases, in comparison with control persons [21]. In this study, the mean FA demonstrated a statistically significant reduction in the cases with TBI in comparison with the control subjects in the following regions; genu, splenium and CS (on both the right and left side). In agreement with our results, in the study by Hanks and his colleagues, not only were FA values showed significant reduction in TBI patients in comparison with controls across the imaged regions, their study also significantly supported the validity of FA values in the body of CC in relation to clinical outcomes after TBI [22]. Also, in accordance with the current findings, a meta-analysis of DTI studies on mTBI subjects demonstrated significantly low FA in the CC in comparison with control subjects. Furthermore, a subanalysis showed a significantly low FA in the splenium, a marginal decrease in FA in the midbody and no alterations in FA in the genue of CC, while in our study there were changes in genue of CC [23].
MRI has now been utilized in investigating the heads of injured patients for many years and has been found to have high sensitivity compared with CT especially for smaller lesions as are often seen in diffuse axonal injury. MRI has also been utilized in many smaller series of TBI patients [24]. None of our 24 cases showed evident white matter abnormalities on conventional MRI studies but they showed altered DTI parameters (Fig. 1)., and this was evidenced by study conducted by Teramaya and his colleagues that recovery might be predicted by DTI in TBI cases. This is especially relevant to mild TBI that causes axonal injury, usually in the context of normal CT/MRI. The capacity of DTI to detect subclinical DAI neuropathologic alterations clarifies the excitement regarding such modality [25, 26].
In the current study, by using the ROC curve analysis, both FA and MD in the genue, splenium and corticospinal tract showed high validity in differentiating cases with TBI in comparison with controls. Also, the validity of combined FA & MD in differentiating cases with trauma are statistically significance in SLF, AF, genue, splenium, ILF and CS.
In addition, Kennedy et al. [27] found long-term (mean = 7 years) reductions in FA and increased MD in the centrum semiovale, and the superior and inferior frontal WM following severe TBI.
Our results also agreed with [28] who investigated Dentatorubrothalamic tract (DRTT) injuries in subjects who had post-traumatic tremors in at least one extremity after mild TBI. Dentatorubrothalamic tract FA values showed significant reduction in patient's limbs as compared to controls (P < 0.05). On the other hand, no significant difference existed in ADC of the DRTT between patient group and controls (P > 0.05).
On the other hand, Bazarian and his colleagues [29] reported high FA of the posterior CC of mTBI patients within 3 days after injury and also reduced ADC. Mayer and his colleagues [21] also reported increased FA in mTBI patients 12.5 ± 5.4 days after injury.
Limitations
The current study has few limitations, as it a single center study and enrolled a relatively small sample size of the patients. Also, the study didn’t compare the different DTI parameters according to the severity of TBI. At last, we didn’t report the changes after follow-up which is a matter of a debate between studies, but it hadn’t been illustrated here. Future study with follow-up MRI is recommended to evaluate the prognostic role of DTI in early detection of WM abnormalities.
Conclusions
DTI parameters is a promising tool in the detection of early brain parenchymal changes in TBI patients with persistent symptoms and no evident abnormalities on conventional MRI. Further more combined use of FA and MD shows better diagnostic accuracy in differentiation between control and trauma patient.
Availability of data and materials
Not applicable.
Abbreviations
- DTI:
-
Diffusion tensor imaging
- TBI:
-
Traumatic brain injury
- MD:
-
Mean diffusivity
- ADC:
-
Apparent diffusion coefficient
- FA:
-
Fractional anisotropy
- SLF:
-
Superior longitudinal fasciculus
- AF:
-
Arcuate fasciculus
- CL:
-
Corpus callosum
- ILF:
-
Inferior longitudinal fasciculus
- CS:
-
Corticospinal
References
Marklund N, Bellander BM, Godbolt AK, Levin H, McCrory P, Thelin EP (2019) Treatments and rehabilitation in the acute and chronic state of traumatic brain injury. J Intern Med 285(6):608–623
Rabinowitz AR, Levin HS (2014) Cognitive sequelae of traumatic brain injury. Psychiatr Clin North Am 37(1):1–11
Bigler ED (2011) Structural Imaging. In: Silver JM, McAllister TW, Yudofsky SC (eds) Textbook of traumatic brain injury, 2nd edn. American Psychiatric Publishing, Washington, pp 73–90
Barr RM, Gean AD, Le TH (2012) Craniofacial trauma. In: Brant WE, Helms CA (eds) Fundamentals of diagnostic radiology, 3rd edn. Lippincott Williams & Wilkins.pp, Philadelphia, pp 55–85
Meythaler JM, Peduzzi JD, Eleftheriou E, Novack TA (2020) Current concepts: diffuse axonal injury-associated traumatic brain injury. Arch Phys Med Rehabil 82(10):1461–1471
Huisman TA, Schwamm LH, Schaefer PW, Koroshetz WJ, Shetty-Alva N, Ozsunar Y, Wu O, Sorensen AG (2004) Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. AJNR Am J Neuroradiol 25(3):370–376
Holshouser BA, Tong KA, Ashwal S (2005) Proton MR spectroscopic imaging depicts diffuse axonal injury in children with traumatic brain injury. AJNR Am J Neuroradiol 26(5):1276–1285
Newcombe V, Chatfield D, Outtrim J, Vowler S, Manktelow A, Cross J, Scoffings D, Coleman M, Hutchinson P, Coles J, Carpenter TA, Pickard J, Williams G, Menon D (2011) Mapping traumatic axonal injury using diffusion tensor imaging: correlations with functional outcome. PLoS ONE 6(5):e19214
Mohammadian M, Roine T, Hirvonen J, Kurki T, Posti JP, Katila AJ, Takala R, Tallus J, Maanpää HR, Frantzén J, Hutchinson PJ, Newcombe VF, Menon DK, Tenovuo O (2020) Alterations in microstructure and local fiber orientation of white matter are associated with outcome after mild traumatic brain injury. J Neurotrauma 37(24):2616–2623
Zhang J, Tian L, Zhang L, Cheng R, Wei R, He F, Li J, Luo B, Ye X (2019) Relationship between white matter integrity and post-traumatic cognitive deficits: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 90(1):98–107
Zhang J, Wei RL, Peng GP, Zhou JJ, Wu M, He FP, Pan G, Gao J, Luo BY (2017) Correlations between diffusion tensor imaging and levels of consciousness in patients with traumatic brain injury: a systematic review and meta-analysis. Sci Rep 7(1):2793
Hulkower MB, Poliak DB, Rosenbaum SB, Zimmerman ME, Lipton ML (2013) A decade of DTI in traumatic brain injury: 10 years and 100 articles later. AJNR Am J Neuroradiol 34(11):2064–2207
Conturo TE, McKinstry RC, Akbudak E, Robinson BH (2013) Encoding of anisotropic diffusion with tetrahedral gradients: a general mathematical diffusion formalism and experimental results. Magn Reson Med 35(3):399–412
Shimony JS, McKinstry RC, Akbudak E, Aronovitz JA, Snyder AZ, Lori NF, Cull TS, Conturo TE (2018) Quantitative diffusion-tensor anisotropy brain MR imaging: normative human data and anatomic analysis. Radiology 212(3):770–784
Shenton ME, Hamoda H, Schneiderman J, Bouix S, Pasternak O, Rathi Y, Vu M-A, Purohit MP, Helmer K, Koerte I (2012) A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav 6(2):137–192
Veeramuthu V, Narayanan V, Kuo TL, Delano-Wood L, Chinna K, Bondi MW, Waran V, Ganesan D, Ramli N (2015) Diffusion tensor imaging parameters in mild traumatic brain injury and its correlation with early neuropsychological impairment: a longitudinal study. J Neurotrauma 32(19):1497–1509
Golby AJ, Kindlmann G, Norton I, Yarmarkovich A, Pieper S, Kikinis R (2011) Interactive diffusion tensor tractography visualization for neurosurgical planning. Neurosurgery 68(2):496–505
Gong G, He Y, Concha L, Lebel C, Gross DW, Evans AC, Beaulieu C (2009) Mapping anatomical connectivity patterns of human cerebral cortex using in vivo diffusion tensor imaging tractography. Cereb Cortex 19(3):524–536
Niogi SN, Mukherjee P (2010) Diffusion tensor imaging of mild traumatic brain injury. J Head Trauma Rehabil 25(4):241–255
Yoo R-E, Choi SH (2021) The emerging role of fast MR techniques in traumatic brain injury. Investig Magn Reson Imaging 25(2):76–80
Mayer A, Ling J, Mannell M, Gasparovic C, Phillips J, Doezema D, Reichard R, Yeo R (2010) A prospective diffusion tensor imaging study in mild traumatic brain injury. Neurology 74(8):643–650
Hanks R, Millis S, Scott S, Gattu R, O’Hara NB, Haacke M, Kou Z (2019) The relation between cognitive dysfunction and diffusion tensor imaging parameters in traumatic brain injury. Brain Inj 33(3):355–363
Klimova A, Korgaonkar MS, Whitford T, Bryant RA (2019) Diffusion tensor imaging analysis of mild traumatic brain injury and posttraumatic stress disorder. Biol Psychiatry Cognit Neurosci Neuroimaging 4(1):81–90
Puig J, Ellis MJ, Kornelsen J, Figley TD, Figley CR, Daunis-i-Estadella P, Mutch WAC, Essig M (2020) Magnetic resonance imaging biomarkers of brain connectivity in predicting outcome after mild traumatic brain injury: a systematic review. J Neurotrauma 37(16):1761–1776
Terayama Y, Meyer JS, Kawamura J et al (1993) Cognitive recovery correlates with white-matter restitution after head injury. Surg Neurol 39:177–186
Ahuja A, Verma S, Chaudhary AN (2018) Outcome of traumatic head injury in unknown patients. Int Surg J 5(2):633–637
Kennedy MR, Wozniak JR, Muetzel RL, Mueller BA, Chiou H-H, Pantekoek K, Lim KO (2009) White matter and neurocognitive changes in adults with chronic traumatic brain injury. J Int Neuropsychol Soc 15(1):130–136
Jang SH, Do Lee H (2020) Injury of the dentatorubrothalamic tract in patients with post-traumatic tremor following mild traumatic brain injury: a case-control study. Neural Regen Res 15(11):2063
Bazarian JJ, Zhong J, Blyth B, Zhu T, Kavcic V, Peterson D (2007) Diffusion tensor imaging detects clinically important axonal damage after mild traumatic brain injury: a pilot study. J Neurotrauma 24(9):1447–1459
Acknowledgements
Not applicable.
Funding
No funding was obtained in this study.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It was a verbal consent, the patient was informed about the maneuver and the timing and it was not invasive and we did not use contrast for our study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsorogy, L.G., Abdelrazek, A.M., Awad, H.A. et al. Altered diffusion tensor imaging (DTI) parameters in brain parenchyma after traumatic brain injury. Egypt J Radiol Nucl Med 53, 251 (2022). https://doi.org/10.1186/s43055-022-00929-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00929-3