Abstract
Background
Although cardiac calcifications are described in the literature, calcification of atria is less frequently reported. There have been few case studies about atrial wall calcification in the literature, most of which were in middle-age females and were attributable to chronic heart diseases including rheumatic heart disease and valve replacement. In majority of the reported cases, interatrial septum has been spared. Only one case of bilateral atrial wall calcification has been reported prior to the current report, which has been in a patient with renal failure, calciphylaxis and long-term haemodialysis and calcium supplement intake.
Case presentation
The patient was a 57-year-old female with history of rheumatic valvular heart disease and two prior valve replacement surgeries. She didn’t have any history of renal function impairment and haemodialysis or calcium supplements intake. Her laboratory data showed anaemia, increased cardiac biomarkers and active urinalysis. Performed echocardiography showed moderate right ventricular dilation with relatively poor contraction, normal left ventricular size and contraction, dilated right and left atria and good prosthetic valve function. On computed tomography (CT) scan, calcification of left atrial posterior and free walls, interatrial septum and right atrial free wall were noted. Evidence of hepatic congestion and cirrhosis was seen in abdominal CT scan and ultrasonography.
Conclusion
Atrial wall calcification is a rare finding but is important to report since it can complicate cardiac surgeries. It's also probable that this kind of dystrophic calcification could not be detected during routine echocardiography and CT scan should be performed in suspected cases.
Similar content being viewed by others
Background
Although cardiac calcifications are well described in the literature, calcification of atria is less frequently reported [1]. First description of left atrium calcification dates back to 1989. Depending on the different extent of calcification of left atrium, different names have been used in the literature, including “porcelain left atrium” for extensive left atrial calcification and “coconut atrium” in rare cases when interatrial septum is also calcified [2]. In addition, based on the extent of calcified components and underlying causes, a classification for left atrium calcification is proposed which includes: Type A or left atrial appendage calcification, where mitral stenosis and left atrium appendage thrombus are the underlying causes, type B or calcification of left atrial free wall and mitral valve, where advanced mitral stenosis is the underlying cause and type C or calcification of McCallum’s patch, where a small portion of left atrium posterior wall is calcified due mitral regurgitation [3].
Diagnosis of atrial wall calcification is important, since it can complicate cardiac surgeries by means of impeding atrial entrance, impaired haemostasis or embolization [1]. In addition, calcified interatrial septum is considered a contraindication for cardiac surgery since it complicates surgical operation and increases patients’ mortality [2].
In a case report and literature review by Leacock et.al, left atrial calcification was shown to have predilection for females ranging late 50 s to early 60 s, the majority of whom had chronic atrial fibrillation. According to the mentioned review, in most cases interatrial septum was spared [1].
According to Vallejo et.al, patients with massive left atrial wall calcification have usually undergone at least one cardiac surgery [4].
An unusual case of left atrial calcification without haemodynamic compromise has been reported by Jones et.al, in which the patient was a 55-year-old African American female with history of end-stage renal disease and failed renal transplant who has been on haemodialysis [5].
Appadurai et al have reported the only case of biatrial wall calcification. In their report the patient was a 34-year-old female with end-stage renal disease, history of two prior renal transplants, total of 16 years of haemodialysis and history of calciphylaxis and subtotal parathyroidectomy. Their patient had also history of regular intake of oral calcium supplement, but no history of rheumatic heart disease or previous heart surgeries. The authors report extensive calcification of both atria with relative sparing of ventricular myocardium and valves in performed echocardiography and calcification of right atrium crista terminalis and calcification of left atrium in non-contrast chest CT scan [6].
Here, we present a case of biatrial calcification in a patient with history of rheumatic valvular heart disease and mitral and tricuspid valve replacement surgery.
Case presentation
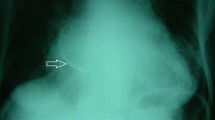
A 57-year-old female with flank pain and dyspnoea presented to our hospital and underwent axial abdominal and chest CT scan. In thoracic images of the CT scan, evidence of mitral and tricuspid prosthetic metallic valves, left and right atrial enlargement and bilateral atrial wall calcification were seen. Calcification of atria included right atrium anterior wall, left atrium posterior and free walls, left atrial appendage and interatrial septum (Figs. 1, 2). In addition, minor thickening and few scattered calcified foci were seen in right pleura. In abdominal images, dilation of IVC and hepatic veins was evident. The liver showed irregular contour with some degrees of right lobe atrophy and left lobe enlargement, suggesting cardiac cirrhosis (Figs. 3, 4). Bilateral nephrolithiasis was also noted.
A complete medical history was obtained and the patient was asked to bring all her medical records to the hospital for further evaluation. She had history of rheumatic valvular heart disease which resulted in mitral and tricuspid valves insufficiency. Subsequently, she had undergone mitral and tricuspid valve replacement surgeries 38 and 12 years ago, respectively. Ever since she has been on anticoagulative therapy with warfarin. She didn't mention taking additional calcium supplement nor having any history of renal function impairment or haemodialysis. She also had undergone diuretic renal scan with Tc-DTPA nine months before the current admission, which showed proper perfusion and function in left kidney and proper perfusion with slightly decreased function in right kidney. She also had undergone echocardiography one month prior to the current admission, which reported left atrium dilation (6.4 cm), normal left atrium appendage, moderately right atrium enlargement with relatively poor contraction, normal size left ventricle with relatively good contraction, mitral and tricuspid metallic valves with no paravalvular leakage and normal mean pressure gradient, mildly thickened aortic valve with mild aortic insufficiency but no aortic stenosis, normal pulmonic valve, normal interatrial and interventricular septa, normal aorta and normal pulmonary venous drainage, left ventricular ejection fraction = 50% and right ventricular ejection fraction = 35%. There was no mentioning of atrial wall or interatrial septal calcification in her echocardiography report. Admission lab tests showed normal calcium and phosphorus blood levels (9.3 and 4.1 mg/dl respectively), lower than normal haemoglobin (9.2 g/dl), INR = 4.3, normal troponin level, increased Pro-BNP (965 pg/ml with upper normal limit of 125 for the age), increased ESR and CRP levels, insignificant WBC and differentiation-count and UA positive for blood, protein and bacteria. Liver function tests including AST, ALT, ALP and bilirubin levels were all within normal ranges. Admission day liver ultrasound showed heterogeneous liver parenchyma with normal portal vein size and flow. Hepatic segment of inferior vena cava was increased in diameter (maximum diameter: 31 mm) and hepatic veins were dilated (mean diameter: 11 mm, measured at level 2 cm away from IVC confluence). Based on axial chest CT scan findings, the patient was diagnosed with biatrial wall and interatrial wall calcification, possibly in the setting of rheumatic valvular heart disease and mitral and tricuspid valve replacement.
The patient was referred for further workup for hepatic cirrhosis including hepatic fibro-scan.
Conclusions
Atrial wall calcification is a rare finding, and biatrial wall calcification is only once reported in the published literature. Since atrial and interatrial septal calcifications are major risk factor for complication and in some cases considered a contraindication for cardiac surgeries, it is important to detect and report these findings in clinical imaging. Most reported cases of atrial wall calcification have been middle-aged females with history of prior rheumatic valvular heart disease. Additionally, interatrial septum is spared in most of the reported cases. Similarly, our patient was female and in her late 50 s had previous rheumatic valvular heart disease with no known history of renal impairment, haemodialysis or additional calcium intake. Therefore, atrial wall calcification was only attributable to previous rheumatic valvular heart disease in this case. However, in our patient interatrial septum and right atrium anterior wall were also calcified. Calcification of interatrial septum in similar reported cases is rare, and to the best of our knowledge no case of right atrial wall calcification has been reported in the setting of rheumatic valvular heart disease.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- Tc-DTPA:
-
Technetium-diethylene-triamine-pentaacetate
- mg:
-
Milligram
- dl:
-
Deciliter
- INR:
-
International normalized ratio
- BNP:
-
Brain natriuretic peptide
- pg:
-
Picogram
- ESR:
-
Erythrocyte sedimentation ratio
- CRP:
-
C-reactive protein
- WBC:
-
White blood cell
- UA:
-
Urinalysis
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine transaminase
- ALP:
-
Alkaline phosphatase
References
Leacock K, Duerinckx AJ, Davis B (2011) Porcelain atrium: a case report with literature review. Case Rep Radiol 2011:501396
Del Campo C, Weinstein P, Kunnelis C, DiStefano P, Ebers GM (2000) Coconut atrium: transmural calcification of the entire left atrium. Tex Heart Inst J 27(1):49–51
Shaw DR, Chen JT, Lester RG (1976) X-ray appearance and clinical significance of left atrial wall calcification. Invest Radiol 11(6):501–507
Vallejo JL, Merino C, González-Santos JM, Bastida E, Albertos J, Riesgo MJ et al (1995) Massive calcification of the left atrium: surgical implications. Ann Thorac Surg 60(5):1226–1229
Jones C, Lodhi AM, Cao LB, Chagarlamudi AK, Movahed A (2014) Atrium of stone: a case of confined left atrial calcification without hemodynamic compromise. World J Clin Cases 2(5):142–145
Appadurai V, Burke MT, Frampton A, Nicolae M (2019) Marked biatrial calcification in long-term haemodialysis. Heart Lung Circ 28(7):e117–e118
Acknowledgements
Not applicable.
Funding
All expenses of the current study have been covered by the authors. No external funding source was used.
Author information
Authors and Affiliations
Contributions
AD chose the case, performed ultrasound, reported the CT scan and ultrasound and supervised manuscript preparation. MAB reviewed the published literature and wrote the case report manuscript. SAP interviewed the patient and collected the patient’s past medical records. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient. Anonymous use of patient's data was approved by the ethics committee of Hasheminejad Kidney Centre.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dadkhah, A., Borjian, M.A. & Akbarzadeh Pasha, S. Biatrial and interatrial septal calcification in the setting of rheumatic heart disease and mitral and tricuspid valves replacement. Egypt J Radiol Nucl Med 53, 156 (2022). https://doi.org/10.1186/s43055-022-00851-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00851-8