Abstract
Background
To prospectively investigate the role of Fast spin-echo T2-weighted (FSE T2-w) and diffusion-weighted imaging (DWI) in magnetic resonance imaging (MRI) for detecting spine bone marrow changes in postmenopausal women with osteoporosis (OP). A total of 101 postmenopausal women, mean age of 60.97 ± 7.41 (range 52–68) years old, who underwent dual-energy X-ray absorptiometry of the spine, were invited to this study and divided into three bone density (normal, osteopenic, and osteoporotic) groups based on T-score. After that MRI scan with both FSE T2-w and DWI of the vertebral body was done to calculate the signal-to-noise ratio (SNR) and apparent diffusion coefficient (ADC). Finally, MRI findings were compared in patients, between three groups and correlated with bone marrow density.
Results
The osteoporotic group showed significantly lower mean ADC values, compared to osteopenic and normal groups (0.58 ± 0.02 vs. 0.36 ± 0.05 vs. 0.24 ± 0.06 × 10–3 mm2/s, p < 0.001). According to these results, a significant positive correlation was found between T-scores and ADC values (r = 0.652, p < 0.001). The mean SNR in FSE T2-w images for normal, osteopenic, and osteoporotic groups was calculated 5.61 ± 0.32, 5.48 ± 0.55, and 6.63 ± 0.67, respectively. No significant correlation was found between the mean SNR and T-score for all groups (r = − 0.304, p > 0.05).
Conclusions
DWI can be used as a noninvasive, quantitative, and valuable technique for OP evaluation. While, routine MRI needs more investigation to be demonstrated as a reliable diagnostic indicator for OP.
Similar content being viewed by others
Background
Osteoporosis (OP), a systemic disease, specified by decreased bone mass and deterioration of the microstructure of bone tissue leads to an increase in bone fragility and fractures [1]. Osteoporotic patients show a growth in the amount of vertebral bone marrow fat and it can worsen progressively with age [2]. The increase of bone marrow fat can be shown as an index to measure the lost bone trabecular tissue. The most frequently utilized technique to assess bone marrow is dual-energy X-ray absorptiometry (DXA). This technique with high reliability has been known as a standard clinical tool for classifying bone mineral density (BMD) with the T-score [3]. Although, DXA is considered as a noninvasive and cost-effective method, its low sensitivity rate can be some drawback [4]. However, bone strength has been shown to depend not on BMD but on the quality of bone marrow.
Magnetic resonance imaging (MRI) with high spatial resolution and excellent soft-tissue contrast can perform as a powerful modality to track the amount of fat in the bone marrow and alterations in normal and pathologic conditions [5]. Some sequences in MRI, such as diffusion-weighted imaging (DWI) and Fast spin-echo T2-weighted (FSE T2-w) can replace or complement DXA to evaluate bone marrow quantitatively and qualitatively.
DWI evaluates the microstructure and diffusivity of the tissue by measuring the random movements of water molecules in biological tissue [6]. Apparent diffusion coefficients (ADC) map derived from DWI can be used to differentiate benign from malignant acute vertebral body compression fractures and bone lesions [7]. Although, some studies showed a correlation between ADC and OP [8, 9], it is not clear whether or not structural changes and diffusion of water molecules in bone marrow are associated with OP.
Conventional FSE T2-w protocol can be considered as a useful technique for bone marrow pathology evaluation. Fat protons show relatively different T2 relaxation, compared to red bone marrow [10]. Patients with OP show a premature conversion of red to yellow bone marrow. Fatty marrow shows higher SI than muscle and red bone marrow [11]. The present study aimed to investigate the potential of DWI and FSE T2-w protocols in assessing bone marrow changes in postmenopausal women with OP.
Methods
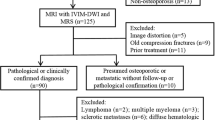
A total of 101 postmenopausal women with back pain visiting our hospital for OP care and control by DXA (DPx-pro MA, GE, USA) between June 2020 and February 2021 were invited to participate in this prospective MRI study. The researchers were blinded to the DEXA outcomes. The informed consent was obtained from patients and then patients with vertebral body fractures, hematologic and bone disorders (metastasis or severe osteoarthritis), metallic devices in their body, malignant tumors, and patients using medication that affect bone marrow physiology were excluded.
According to institutionally approved procedures and regulations, ethical approval was obtained for our study.
DXA examination
BMD data were achieved using a DXA scanner. In this procedure, patients were positioned supine. After completion of DXA scanning, the results were obtained for L1, L2, L3, and L4 of each patient and then the mean T-score was calculated for every patient. According to the World Health Organization (WHO) criteria [12] participants were divided into three groups based on DXA results: normal BMD (T ˃ − 1); osteopenia (T = − 1 to − 2.5); and OP (T ˂ − 2.5).
MRI Scan
MRI was done using a 1.5 T MRI system (Philips 2011, Achieva 1.5 Tesla) and a spinal array surface coil for signal acquisition. FSE T2-w images (TR 3500 ms; TE 100 ms; slice thickness 4 mm; ETL = 15; matrix size 240 × 320; field of view 350 mm) of the lumbar spine were obtained in the sagittal plane. These images were used to guide the position of a region of interest (ROIs) within the boundaries of the L1, L2, L3, and L4 vertebral bodies for DWI. DWI of a lumbar vertebral body in the sagittal plan was gained using a single-shot spin-echo planar sequence (TR 3000 ms; TE 80 ms; slice thickness 5 mm; field of view 150 mm; matrix size 128 × 256). DWI was obtained using three diffusion sensitivity parameters (b-values) of 0, 400, and 800 mm2/s in three planes (x, y, z).
Quantitative data analysis
For the quantitative assessment of FSE T2-w images, ROIs were placed over the bone marrow of each lumbar vertebral body on sagittal images to measure signal intensities (SIs). Measurements of noise magnitude were taken by measuring standard deviations (SDs) outside the body at four locations. After that the signal-to-noise ratio (SNR) was calculated.
For DWI assessment, ROIs were placed over vertebral bodies exactly like FSE T2-w images and SIs were achieved. The DWI with a b-value of 400 mm2/s produced images with greater quality and SIs than the b-value of 800 mm2/s. Therefore, ADC maps were generated, using b-value of 0 and 400 mm2/s.
The relationship between SNR, ADC, and BMD in all patients was evaluated, using Spearman correlation analysis. The T-score of L1, L2, L3, and L4 was used as a reference and then receiver operating characteristic (ROC) data were used as an OP indicator to estimate the diagnostic performance of MRI protocols.
Statistical analysis
Statistical analysis was done using SPSS version 25. Categorical variables were shown as frequencies and percentages. Continuous variables were introduced as (Means ± SD). Fisher's exact test was used to show the association between categorical variables. ANOVA test was used to compare means between three groups or more. A p value of ≤ 0.05 was considered significant. The accuracy, specificity, sensitivity, negative predictive value (NPV), and positive predictive value (PPV) of the DWI and T2-w techniques were calculated to diagnose osteoporosis and osteopenia.
Results
Our study involved 101 postmenopausal women, mean age of 60.97 ± 7.41 (range 52–68) years old, who underwent DXA and conventional MRI with FSE T2-w and DWI. Significant differences were found based on participants' age between normal, osteopenic, and osteoporotic groups (p < 0.05). The number of participants in normal, osteopenic, and osteoporotic groups was 18 (54.78 ± 2.34 years old), 25 (59.64 ± 4.52 years old), and 58 (63.10 ± 5.17 years old), respectively. Our study reported the mean T-score of − 0.59 ± 0.27, − 1.65 ± 0.35, and − 2.78 ± 0.61 for normal, osteopenic, and osteoporotic groups, respectively. DXA and MRI using FSE T2-w and DWI protocols were done for the L1, L2, L3, and L4 vertebral body of all patients. The DWI with a b-value of 400 mm2/s produced images with greater quality and signal intensity than the b-value of 800 mm2/s. Therefore, ADC maps were generated, using b-value of 0 and 400 mm2/s. The ADC results showed considerable differences between three groups (p < 0.05). A significant association could be considered between the age of patients and the ADC values. As shown in Table 1, a significant difference was shown between the mean ADC values for normal, osteopenic, and osteoporotic groups (0.58 ± 0.02, 0.36 ± 0.05, and 0.24 ± 0.06 × 10–3 mm2 /s, respectively, p < 0.001). Increasing the age of patients is considerably associated with lower ADC values (p < 0.001).
The mean SNR values for normal, osteopenic, and osteoporotic groups were achieved 5.61 ± 0.32, 5.48 ± 0.55, and 6.63 ± 0.67, respectively, with no significant differences between each other (p > 0.05). The association between the age and the SNR of FSE T2-w images was not found significant (p > 0.05). Figures 1 and 2 show an example of osteoporotic and osteopenic patients, respectively, with DWI, FSE T2-w, and DXA images.
66 years old postmenopausal woman with osteoporotic vertebrae. a DWI of lumbar vertebrae with different b-values (0, 400, 800 mm2/s). ADC values for L1, L2, L3, and L4 were achieved 0.26, 0.20, 0.19, and 0.17 × 10–3 mm2/s, respectively. FSE T2-w image shows inhomogeneous signal intensity in L1, L2, L3, and L4 vertebral bodies with SNR of 5.60, 6.12, 6.21, and 6.54, respectively. b DXA shows the T-score values of 0.1, − 2.0, − 3.2, and − 3.6 for L1, L2, L3, and L4, respectively
58 years old postmenopausal woman with osteopenic vertebrae. a DWI of lumbar vertebrae with different b-values (0, 400, 800 mm2/s). ADC values for L1, L2, L3, and L4 were achieved 0.16, 0.15, 0.2, and 0.18 × 10–3 mm2/s, respectively. FSE T2-w image shows inhomogeneous signal intensity in L1, L2, L3, and L4 vertebral bodies with SNR of 5.18, 5.41, 6,63, and 6.58, respectively. b DXA shows the T-score values of − 1.6, − 1.6, − 2.1, and − 1.9 for L1, L2, L3, and L4, respectively
As shown in Fig. 3, the Spearman correlation test showed a significant correlation between ADC and BMD values in all groups (r = 0.652, p = 0.001). No meaningful correlation was shown between FSE T2-w images and BMD values (r = − 0.304, p > 0.05).
Table 2 shows sensitivity, specificity, NPV, PPV, and accuracy values were achieved 73.6%, 73.6, 79.00%, 67.39%, and 73.59%, respectively, for ADC and 68.00%, 57.39%, 66.51%, 52.45%, and 57.92%, respectively, for FSE T2-w images. The area under the curve (AUC) for ADC values was higher than those of FSE T2-w images (0.82 vs.0.67).
Discussion
OP, a systemic skeletal disease, is characterized by generally reduced bone density and structural deterioration of bone with bone fragility and reducing the quality of life [13]. It has been supposed that patients with OP have decreased vertebral marrow perfusion and increased marrow fat. With aging, the composition of bone marrow is replaced by adipocytes, low osteoblast function, and high osteoclast activity, resulting in OP. The study conducted by Griffith JF et al. [14] reported the mean T-score of − 0.05 ± 0.86, − 1.82 ± 0.44, and − 3.37 ± 0.6 for normal, osteopenic, and osteoporotic groups, respectively, that were approximately similar with our study (the mean T-score of − 0.59 ± 0.27, − 1.65 ± 0.35, and − 2.78 ± 0.61 for normal, osteopenic, and osteoporotic groups, respectively).
Previous studies [12, 13] showed that, without bone fragility fracture, OP in premenopausal women could not be recognized with DXA alone. Increasing the fat content of the vertebral marrow may cause errors in DXA measurements with misrepresentation of the patient's true bone status. While, this phenomenon may affect the signal intensity of bone marrow in MRI and generate some contrast. In this study, we focused on L1–L4 and found a significant association between the mean age of the patients and the BMD that was represented by T-score as well as ADC values, in a way increasing the age of the patient was significantly associated with a lower T-score and ADC value. These findings matched to the results of previous studies [15,16,17].
Quantitative histological and spectroscopic studies [4, 15] have reported a higher quantity of fat in bone with age. Schellinger et al. [15] reported that bone marrow fat in osteoporotic patients can be measured by MRI nearly as well as BMD.
According to the change of bone marrow fat, as an important factor in OP [5], the ADC and FSE T2-w measurements can be valuable techniques to measure this disease. These two techniques are sensitive to inhomogeneities caused by susceptibility differences at the bone marrow/trabeculae interface [18]. Our study evaluated the role of ADC and FSE T2-w imaging of the vertebral bone marrow as reliable techniques for evaluating OP. We also compared the diagnostic ability of DWI and FSE T2-w sequences to that of BMD evaluations by DXA.
Increasing the fat contents within the vertebral bodies may decrease extracellular diffusion and lead to ADC values reduction. The diffusion sensitivity can be easily changed by changing the b value. Water molecules with a higher degree of motion or greater diffusion distance (like those within the intravascular space) show low signals even with small b-values (e.g., b = 50–100 mm2/s). While, the diffusivity of fat-bound water molecules is usually lower than that of watery tissue. Water molecules that have a slower degree of motion or have smaller diffusion distances will show signal attenuation with larger b-values (e.g., b = 1000 mm2/s) because these molecules display more gradual signal attenuation with increasing b-value [19].
In vertebral body and bone marrow, the ADC is sensitive to non-homogeneities caused by susceptibility differences at the of bone marrow/trabeculae interface [18]. The present study showed significant differences in ADC values between normal, osteopenic, and osteoporotic groups (0.58 ± 0.02, 0.36 ± 0.05, and 0.24 ± 0.6 × 10–3 mm2/s, respectively) that were approximately similar to previous studies [12, 17, 19]. However, the ADC value with normal BMD was higher in this study than previous studies. Abdulazeez RA et al. [19] reported 0.46 ± 0.09, 0.42 ± 0.08, and 0.39 ± 0.05 × 10–3 mm2/s for normal, osteopenic, and osteoporotic groups, respectively. Yong et al. [20] also reported the ADC value of 0.47 ± 0.03, 0.42 ± 0.02, and 0.39 ± 0.03 × 10–3 mm2/s, respectively.
Our study showed a significant positive correlation between the T-score and ADC values (r = 0.652, p = 0.001) that was approximately similar to Yong et al. [20] study (r = 0.802, p < 0.001). Tang et al. [16] also reported approximately the same correlation between the T-score and ADC values (r = 0.835, p < 0.001).
In another study, Momeni et al. [21] used an ADC map to determine bone intensity in the vertebrae. DWI sequence and BMD values showed a significant correlation. ADC results showed meaningful differences between normal, osteopenic, and osteoporotic vertebras. They reported a sensitivity of 90.90%, specificity of 83.34%, PPV of 93.75%, NPV of 76.93%, and accuracy of 88.89%, which were higher than our results (sensitivity, specificity, PPV, NPV, and accuracy values were achieved 73.6%, 73.6, 79.00%, 67.39%, and 73.59%, respectively, for ADC values). Koyama et al. [5] indicated a negative and significant correlation between ADC and BMD values that could be due to the small sample size (16 patients) of their study. However, they found a significant difference between ADC values in the normal and osteoporotic vertebral body (3.04 ± 2.42 and 6.47 ± 1.38 × 10–5 mm2/s, respectively). They reported sensitivity, specificity, PPV, and NPV of 70%, 75%, 66.7%, 77.8%, and 72.9%, respectively, for the DWI technique. These results are in agreement with our results.
FSE T2-w sequences can be useful for assessing bone marrow pathology [10]. FSE T2-w images display intermediate to high SI from yellow marrow. Both water and fat generate high SI in this sequence, while the SI from red marrow is somewhat lower than that of yellow marrow. Although, by increasing the marrow fat content we had greater SNR in osteoporotic patients, no meaningful correlation was found between DXA and FSE T2-w images (r = − 0.304, p > 0.05). This study reported a sensitivity of 68.8%, specificity of 57.5%, PPV of 66.51%, NPV of 52.45%, and accuracy of 57.92% which were comparable with the previous study [9] done by Koyama et. al with a sensitivity of 95%, specificity of 71.4%, PPV of 70.4%, NPV of 95.2%, and accuracy of 81.3%. However, they showed a remarkable difference between the SNR of normal and osteoporotic vertebrae, using the FSE T2-w sequence (5.72 ± 4.35 vs. 8.81 ± 3.32). Our study showed a significant difference between the SNR of the normal and osteoporotic vertebral bodies as well (5.61 ± 0.32 vs. 6.63 ± 0.67, p < 0.05). While SNR not only showed no significant difference between normal and osteopenic groups, but also it was lower in the osteopenic group (5.61 ± 0.32 vs. 5.48 ± 0.55, p > 0.05). Kumar et al. [11] also investigated on 50 patients with both DXA and conventional MRI. Unlike our study, they reported a negative significant correlation between DXA and SNR of T2w images (r = − 0.590, p < 0.000) which can be due to different scanner devices and other scanning conditions.
Therefore, DWI and ADC values represent a potentially powerful technique for the evaluation of early bone marrow changes in postmenopausal women. But, for conventional MRI protocols like FSE T2-w images, more studies must be done to determine their role in bone marrow changes evaluation.
Limitations of the study were: First, patients’ sample size was relatively small, and we had some bias in patient selection such as no malignant tumors or vertebral fracture and just postmenopausal women included in this study. While, a selection bias can be reduced by choosing a large number of patients. Second, as mentioned above, changing the ADC values, according to different b-values, may lead to different imaging outcomes. Therefore, solving these problems may lead to different results. Third, the conventional MRI assessment under different conditions (such as the use of other scanning conditions or other scanner manufacturers) be able to change the SNR. Therefore, the role of different scan conditions and scanner manufacturers should be investigated in imaging outcomes in future studies.
Conclusions
This study indicated a meaningful correlation between ADC and BMD values. These values were considerably different between normal, osteopenic, and osteoporotic groups. Although, this study showed ADC map can be comparable with DXA as a gold standard technique for OP diagnosis, more studies must be done on DWI as a non-radiation technique to evaluate its accuracy and correlation with DXA. However, in the future, a combination of these two techniques can provide complementary information about bone mass, microstructural deterioration, and fatty bone marrow. However, routine MRI needs more investigation to be demonstrated as a reliable diagnostic indicator for OP.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- OP:
-
Osteoporosis
- ADC:
-
Apparent diffusion coefficient
- FSE:
-
Fast spin echo
- BMD:
-
Bone mineral density
- DWI:
-
Diffusion weighted imaging
- DXA:
-
Dual X-ray absorptiometry
- MRI:
-
Magnetic resonance imaging
- FSE T2-w:
-
Fast spin echo T2-weighted
- WHO:
-
World Health Organization
- SNR:
-
Signal-to-noise ratio
- SI:
-
Signal intensity
- ROI:
-
Regions of interest
- SD:
-
Standard deviation
- AUC:
-
Area under the curve
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
References
Link TM (2016) Radiology of osteoporosis. Can Assoc Radiol J [Internet] 67(1):28–40. https://doi.org/10.1016/j.carj.2015.02.002
Chou SH, LeBoff MS (2017) Vertebral imaging in the diagnosis of osteoporosis: a clinician’s perspective. Curr Osteoporos Rep 15(6):509–520. https://doi.org/10.1007/s11914-017-0404-x
Oishi Y, Nakamura E, Murase M, Doi K, Takeuchi Y, Hamawaki JI, Sakai A (2019) Lower lumbar osteoporotic vertebral fractures with neurological symptoms might have two different pathogeneses according to early magnetic resonance images. Acta Neurochir 161(10):2211–2222. https://doi.org/10.1007/s00701-019-04045-6
Palmer W, Bancroft L, Bonar F, Choi JA, Cotten A, Griffith JF et al (2020) Glossary of terms for musculoskeletal radiology. Skeletal Radiol 49:1–33. https://doi.org/10.1007/s00256-020-03465-1
Koyama H, Yoshihara H, Kotera M, Tamura T, Sugimura K (2013) The quantitative diagnostic capability of routine MR imaging and diffusion-weighted imaging in osteoporosis patients. Clin Imaging 37(5):925–929. https://doi.org/10.1016/j.clinimag.2013.05.001
Wu HZ, Zhang XF, Han SM, Cao L, Wen JX, Wu WJ, Gao BL (2020) Correlation of bone mineral density with MRI T2* values in quantitative analysis of lumbar osteoporosis. Arch Osteoporos 15(1):1–7. https://doi.org/10.1007/s11657-020-0682-2
Luo Z, Litao L, Gu S, Luo X, Li D, Yu L, Ma Y (2016) Standard-b-value vs low-b-value DWI for differentiation of benign and malignant vertebral fractures: a meta-analysis. Br J Radiol 89(1058):20150384. https://doi.org/10.1259/bjr.20150384
Karampinos DC, Ruschke S, Dieckmeyer M, Diefenbach M, Franz D, Gersing AS, Baum T (2018) Quantitative MRI and spectroscopy of bone marrow. J Magn Reson Imaging 47(2):332–353. https://doi.org/10.1002/jmri.25769
Huang CWC, Tseng J, Yang SW, Lin YK, Chan WP (2019) Lumbar muscle volume in postmenopausal women with osteoporotic compression fractures: quantitative measurement using MRI. Eur Radiol 29(9):4999–5006. https://doi.org/10.1007/s00330-019-06034-w
Colón-Emeric CS, Saag KG (2006) Osteoporotic fractures in older adults. Best Pract Res Clin Rheumatol 20(4):695–706. https://doi.org/10.1016/j.berh.2006.04.004
Dahiya RK. Comparative Study of DEXA and 1.5 Tesla MRI in Quantitative Estimation of Bone Mineral Density in Lumbar Spine. IJRR HISTORY, 4 (2005). https://www.ijrrjournal.com/IJRR_Vol.6_Issue.8_Aug2019/Abstract_IJRR0010.html
Compston J, Bowring C, Cooper A, Cooper C, Davies C, Francis R et al (2013) Diagnosis and management of osteoporosis in postmenopausal women and older men in the UK: National Osteoporosis Guideline Group (NOGG) update 2013. Maturitas 75(4):392–396. https://doi.org/10.1016/j.maturitas.2013.05.013
Chen Y, Guo Y, Zhang X, Mei Y, Feng Y, Zhang X (2018) Bone susceptibility mapping with MRI is an alternative and reliable biomarker of osteoporosis in postmenopausal women. Eur Radiol 28(12):5027–5034. https://doi.org/10.1007/s00330-018-5419-x
Griffith JF, Yeung DK, Antonio GE, Wong SY, Kwok TC, Woo J, Leung PC (2006) Vertebral marrow fat content and diffusion and perfusion indexes in women with varying bone density: MR evaluation. Radiology 241(3):831–838. https://doi.org/10.1148/radiol.2413051858
Schellinger D, Lin CS, Lim J, Hatipoglu HG, Pezzullo JC, Singer AJ (2004) Bone marrow fat and bone mineral density on proton MR spectroscopy and dual-energy X-ray absorptiometry: their ratio as a new indicator of bone weakening. AJR Am J Roentgenol 183(6):1761–1765. https://doi.org/10.2214/ajr.183.6.01831761
Tang GY, Lv ZW, Tang RB, Liu Y, Peng YF, Li W et al (2010) Evaluation of MR spectroscopy and diffusion-weighted MRI in detecting bone marrow changes in postmenopausal women with osteoporosis. Clin Radiol [Internet] 65(5):377–381. https://doi.org/10.1016/j.crad.2009.12.011
Manenti G, Capuani S, Fanucci E, Parfait E, Masala S, Sorge R et al (2013) Diffusion tensor imaging and magnetic resonance spectroscopy assessment of cancellous bone quality in femoral neck of healthy, osteopenic and osteoporotic subjects at 3T : preliminary experience. Bone [Internet] 55(1):7–15. https://doi.org/10.1016/j.bone.2013.03.004
Leonhardt Y, Gassert FT, Feuerriegel G, Gassert FG, Kronthaler S, Boehm C et al (2021) Vertebral bone marrow T2* mapping using chemical shift encoding-based water-fat separation in the quantitative analysis of lumbar osteoporosis and osteoporotic fractures. Quant Imaging Med Surg 11(8):3715. https://doi.org/10.21037/qims-20-1373
Abdulazeez RAJ, Tawfeeq RHA, Noori FA (2017) Role of T1 Weighted and Diffusion Weighted Magnetic Resonance imaging application in the diagnosis of osteoporosis in lumbar spine in postmenopausal women. Univ Thi-Qar J Med 14(2):158–173
Yong LIU, Tang GY, Tang RB, Peng YF, Wei LI (2009) Assessment of bone marrow changes in postmenopausal women with varying bone densities: magnetic resonance spectroscopy and diffusion magnetic resonance imaging. Chin Med J 122(12):1524–1527. https://doi.org/10.3760/cma.j.issn.0366-6999.2010.12.008
Momeni M, Asadzadeh M, Mowla K, Hanafi MG, Gharibvand MM, Sahraeizadeh A (2020) Sensitivity and specificity assessment of DWI and ADC for the diagnosis of osteoporosis in postmenopausal patients. Radiol Med (Torino) 125(1):68–74. https://doi.org/10.1007/s11547-019-01080-2
Acknowledgements
Not applicable
Funding
There was no source of funding.
Author information
Authors and Affiliations
Contributions
FAA-B interpreted all images and wrote discussion section. MAT and SMAH collected data and wrote introduction as well as Material and Method. Sadegh Dehghani managed this project and edited manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been ethically approved by the ethics committee of Tehran University of Medical Sciences (ID number, IR.TUMS.SPH.REC.1400.095) and formal informed consent was waived. There was no potential risk to patients in this retrospective study.
Consent for publication
Written consent to publish this information was obtained from study participants and proof of consent to publish from study participants can be requested at any time.
Competing interests
The authors have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hammood, S.M.A., Ali Talib, M., Al-Baghdadi, F.A. et al. The role of Fast spin-echo T2-weighted and diffusion-weighted imaging for spine bone marrow changes evaluation in postmenopausal women with osteoporosis. Egypt J Radiol Nucl Med 53, 158 (2022). https://doi.org/10.1186/s43055-022-00834-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00834-9