Abstract
Background
Magnetic resonance imaging (MRI) plays an important role in the differentiation of hepatic focal lesions and diagnosis of hepatic malignancy, especially hepatocellular carcinoma which is a major health problem worldwide. Diffusion imaging is a functional MRI technique that became an essential part of MRI study of the liver. Recently, diffusion tensor imaging (DTI) is diffusion variant that can provide more information than conventional diffusion imaging based on the tissue anisotropy. The aim of this study was to present the role of DTI in the assessment and differentiation between hepatic focal lesions.
Results
Fifty-one patients having 95 hepatic focal lesions who underwent dynamic MRI with conventional diffusion imaging and DTI acquisition were included in the study. A positive moderate significant correlation was found between Fractional anisotropy (FA) values and Liver Imaging Reporting and Data System (LI-RADS) category while substantial negative significant correlation and moderate negative significant correlation were found between DTI-ADC and DWI-ADC values, respectively, with the LI-RADS category. There was a significant negative correlation between DTI-ADC and FA values. DTI-ADC showed a significant role in differentiation of benign from malignant lesions with cut-off value 0.905 × 10−3 having 88.7% sensitivity and 88.3% specificity compared to 78.5% and 68.7% for DWI-ADC, respectively. Also, it was found that FA value had a significant role in differentiation between benign and malignant lesions with cut-off value 0.34 having 87.1% sensitivity and 73.9% specificity.
Conclusions
DTI can be included in liver MRI studies for better tissue characterization as it may perform better than conventional DWI with higher sensitivity and specificity of DTI-ADC and FA values than conventional DWI-ADC.
Similar content being viewed by others
Background
Triphasic CT and dynamic contrast enhanced MRI (DCE-MRI) play a crucial role in the diagnosis of suspected hepatic malignancy especially HCC which is considered a major health problem worldwide particularly in developing countries. The HCC represents the fourth common malignancy in developing countries with the number of HCC patients has increased two-folds over the last decade [1, 2].
Unfortunately, in some situation, contrast usage may not be feasible like patients with impaired renal functions; hence, unenhanced functional MRI techniques like diffusion weighted images (DWI) and diffusion tensor imaging (DTI) gained more clinical interest [3].
DTI is a diffusion variant which is used to evaluate the anisotropic tissue properties by applying motion probing gradients along multiple space directions (at least six directions) [4]. This may be helpful in the study of the malignant lesions in which diffusion properties are currently still controversial to be isotropic (not restricted to a certain direction) or anisotropic (restricted to a certain direction). Fractional anisotropy (FA) is a quantitative measure of DTI which describes the degree of anisotropy. It ranges between 0 where it represents maximum isotropy and 1 which stands for maximum anisotropy [5].
DTI has been traditionally applied to the brain, where it is extensively used in the evaluation of brain tumor, injury and degeneration [5]. On contrary, the available researches about the DTI benefits in hepatic diseases are limited with further studies are required to determine its value [6]. Few studies described the role of DTI in assessing the degree of liver fibrosis. Many of them were performed on animal models. While for characterization of hepatic focal lesions, studies are few and sparse.
For standardization of the interpretation and reporting of the liver imaging, the American College of Radiology established the Liver Imaging Reporting and Data System (LI-RADS) which based on the presence of specific imaging features representing the HCC development probability by assigning categories ranging from LR-1 (definitely benign) to LR-5 (definitely HCC) or LR-TIV (definite tumor in vein) [7,8,9].
The aim of this study was to assess the role of liver diffusion tensor imaging (L-DTI) using the FA and DTI-ADC values in the characterization and differentiation between hepatic focal lesions (HFL) based on their typical imaging features and histopathology in atypical cases.
Methods
Study population and design
A cross-sectional analytic study was approved by the research ethics community (REC) of our institution. The study was performed over a period of 18 months from December 2019 to May 2021 and included 51 patients with high risk of HCC development as defined by the LI-RADS system (Table 1). The patients had HFL diagnosed with other imaging modalities than MRI. All patients had been subjected to full clinical assessment, revision of the laboratory investigations including renal function tests, revision of the previous radiological investigations done for the patients. A written informed consent was signed by all patients.
The exclusion criteria were as follows: patients not fulfilling the LI-RADS criteria of population where it exclusively applied on (Table 1), patients underwent any interventional procedures (e.g., TACE or radiofrequency), contraindication to contrast media (i.e., renal failure or patients allergic to contrast media) and absolute MRI contraindications (i.e., claustrophobic patients and non-MRI compatible devices).
All patients included in the study underwent DCE-MRI with conventional diffusion and DTI acquisition followed by post processing to obtain DWI-ADC, DTI-ADC and FA maps.
MRI Protocol
All studies were performed on a 1.5 T magnet (Achieva, Philips medical system) using a torso phased-array coil. The study protocol included:
Pre-contrast and dynamic sequences
Table 2 summarizes the parameters of the used pre-contrast sequences and dynamic study. Dynamic imaging was obtained using THRIVE sequence. It consisted of one pre-contrast series followed by four successive post-contrast series including early arterial, late arterial, and portal phases with 19–21 s intervals (17 s for image acquisition with breath-holding and 2–4 s for rebreathing). This is followed by 3–5 min delayed phase. The contrast used was Gd-DTPA and administrated by manual bolus injection of 0.1 mmol/kg body weight.
Diffusion weighted images (DWI) and diffusion tensor images (DTI)
Table 2 summarizes the parameters used in DWI and DTI sequences. DWI and DTI were performed using respiratory triggered single-shot EPI sequences. The scan time for DTI is about 4–5 min compared to 4 min for conventional diffusion sequences. FA, DTI-ADC and DWI-ADC maps are calculated by the vendor software on a pixel-by-pixel basis.
Analysis of the MRI images
Images were sent to the workstation (Phillips Extended MR workspace) for further image processing. The images were assessed by experienced abdominal imaging radiologist with 15 years’ experience in abdominal imaging. The morphological features of each lesion were recorded including number, site, size, margins and signal intensity at T1, T2, SPAIR and DWI images. Pattern of enhancement through the dynamic series was also assessed. Finally, LI-RADS category was recorded.
ADC maps derived from the DTI and DWI sequences as well as the FA maps were assessed quantitatively by measuring ADC and FA values in each lesion. A 1 cm ROI was placed within the confines of the lesion.
Standard of reference
Obtaining histopathological confirmation in all patients was not feasible for the following reasons: 1. Most of these patients did not undergo surgery, 2. the fact that HCC is almost the only tumor that could be diagnosed by imaging only without a need for histopathological confirmation, 3. ethical concern related to biopsy of benign lesions, and 4. biopsy of small lesions may result in sampling error. So, the typical imaging features of the lesions were used as standard of reference; however, histopathological confirmation was obtained in 22 lesions which had atypical imaging features or being non-HCC malignant HFL like cholangiocarcinoma and metastasis.
Statistical analysis
Data were summarized using mean, standard deviation, median, minimum and maximum in quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. The relationship of DTI-ADC and FA values was evaluated using Pearson’s correlation. Also, the relationship of FA, DTI-ADC and DWI-ADC values of the included HFL with their LI-RADS category was evaluated using the same aforementioned test. The differences in FA, DTI-ADC and DWI-ADC values of the HFL according to their LI-RADS category and their type were evaluated using ANOVA and post-hoc Tukey test.
To evaluate the role of FA, DTI-ADC and DWI-ADC values in distinguishing the benign HFL from the malignant ones, ROC analysis was applied. The areas under the curve were calculated. Cut-off values for FA, DTI-ADC and DWI-ADC values were determined for discrimination of the benign from malignant lesions. Sensitivities and specificities with 95% confidence intervals were also calculated accordingly.
Results
-
A.
Socio-demographic and clinical data
Our study included 51 patients having 95 HFL, 27 patients had a single lesion and 24 patients had more than one lesion. The patients’ ages ranged from 27 to 77 years old (mean age was 54.5 years old). Of the 51 patients, there were 28 males and 23 females.
-
B.
Types and LI-ADS category of the included HFL
The study included 28 HCC (29.5%), 19 cysts (20%), 17 dysplastic nodules (17.9%), 11 hemangiomata (11.1%), 7 metastatic lesions (7.3%), 4 cholangiocarcinoma (4.2%), 3 regenerative nodules (3.2%), 3 FNH (3.2%), 2 hepatic abscesses (2.1%) and finally one lesion of transient hepatic intensity difference (THID) (1.1%).
According to the LI-RADS categories, the study included 22 LR-1 lesion (23.16%), 14 LR-2 lesion (14.74%), 11 LR-3 lesion (11.58%), 15 LR-4 lesion (15.79%), 18 LR-5 lesion (18.95%), 11 LR-M lesion (11.58%) and finally 4 LR-TIV lesion (4.21%).
-
III.
Descriptive analysis of the FA, DTI-ADC and DWI-ADC values of the included HFL according to their types and LI-ADS category
Tables 3 and 4 present the mean FA, DTI-ADC and DWI-ADC values among the different lesions according to LI-RADS categories.
-
IV
The relationship of the FA and the DTI-ADC values
There was a substantial negative significant correlation between DTI-ADC and FA values with \(r = - \;0.515\) and \(p_{{{\text{value}}}} < 0.001\).
E. Correlation of the FA, DTI-ADC and DWI-ADC values to the LI-RADS category
Based on the hypothesis that the malignant lesions have more restricted and more anisotropic diffusion compared to the benign ones, this will be reflected as higher FA and lower DTI-ADC values for the malignant lesions and vice versa (Figs. 1, 2, 3, 4, 5). A positive moderate significant correlation was found between FA values and the LI-RADS category with \(r = 0.386\) and \(P_{{{\text{value}}}} < 0.001\). Meanwhile, a substantial negative significant correlation was found between LI-RADS and DTI-ADC values with \(r = - \;0.639\) and \(P_{{{\text{value}}}} < 0.001\). Finally, a moderate negative significant correlation was found between LI-RADS and DWI-ADC values with r = − 0.444 and \(P_{{{\text{value}}}}\)<0.001. Also, an overall significant difference of FA, DTI-ADC and DWI-ADC values among the different LI-RADS categories was found by using ANOVA test, with the test statistic was 3.551, 16.095 and 7.195 with a significant P value of < 0.001 for the FA, DTI-ADC and DWI-ADC, respectively.
-
F.
Correlation of the FA, DTI-ADC and DWI-ADC values to the lesions’ types
A 62-year-old male patient with positive HCV and accidentally discovered HFL by US. A Axial T2 image shows a large right hepatic lobe mass (blue arrow) and a smaller one at segment IV (orange arrow). B axial diffusion and C ADC images showed restricted diffusion with ADC value 1.1 for the large lesion and 1.05 for the smaller one D Axial DTI gray scale image, E DTI-ADC map and F FA map: the ADC value is 0.66 for the large lesion and 0.61 for the smaller one which is lower than conventional ADC and the FA value was high (0.55 for the large lesion and 0.58 for the smaller one). G Non-contrast T1 H arterial phase and I delayed phase of the dynamic study showed faint heterogeneous arterial enhancement of the smaller lesion while no significant enhancement within the larger one and both show delayed wash out and enhancing capsule; also, there is an eccentric hemorrhagic area in the larger lesion, and imaging features were compatible with HCC. The large lesion was categorized as LR 4 (due to lack of arterial hyperenhancement) and the smaller lesion was categorized as LR 5. Another small subcapsular focal lesion is also noted at left lobe segment II showing arterial enhancement with no diffusion restriction or delayed wash out, this was categorized as LR 3 (probably a dysplastic nodule), the FA value was 0.36, the DTI-ADC was 0.81 and the diffusion ADC was 1.2
A 45-year-old female patient with positive HCV and history of ovarian cancer underwent abdominal ultrasonography that showed right hepatic focal lesion. A Axial T2 image shows a 4 cm segment VI focal lesion displaying low T2 signal. B axial diffusion and C ADC images show marked diffusion restriction with DWI-ADC value 0.82 D Axial DTI gray scale image, E DTI-ADC map and F FA map: the DTI-ADC value is 0.57 and the FA value was high 0.54. G non-contrast T1 H arterial phase and I delayed phase of the dynamic study showed heterogeneous enhancement of the lesions. The lesion was categorized as LR-M. True cut biopsy was done and the pathology result was metastatic adenocarcinoma
A 60-year-old male patient with positive HBV presented with jaundice. He underwent abdominal ultrasonography that showed liver cirrhosis and right hepatic lobe lesion. A Axial T2 image shows large mass lesion is seen infiltrating almost whole right lobe roughly measuring about 15.5 cm eliciting high T2 signal. B axial diffusion and C ADC images show mild diffusion restriction with DWI-ADC value 1.25 D Axial DTI gray scale image, E DTI-ADC map and F FA map: the DTI-ADC value was 1.12 (much lower than conventional ADC) and the FA value was high = 0.45. G non-contrast T1 H arterial phase and I delayed phase of the dynamic study showed heterogenous progressive delayed enhancement of the lesions. The lesion was categorized as LR-M. True cut biopsy was done and the pathology result was cholangiocarcinoma
A 40-year-old HBV positive male patient underwent routine abdominal ultrasonography that showed small left hepatic focal lesion. A A small left lobar segment II focal lesion is seen measuring about 2.3 cm eliciting high T2 signal. B axial diffusion and C ADC images show facilitated diffusion with DWI-ADC value 2.22 × 10−3 D Axial DTI gray scale image, E DTI-ADC map and F FA map: the DTI-ADC value was 2.21 and the FA value was low = 0.26 suggestive of benign nature. G non-contrast T1 H arterial phase and I delayed phase of the dynamic study showed nodular enhancement that progress into complete filling in the delayed phase, and imaging features were compatible with hemangioma. The lesion was categorized as LR-1
A 27-year-old female patient with past history of viral C hepatitis underwent routine abdominal ultrasonography that showed left hepatic focal lesion. A Axial T2 image shows A 3.7 cm left lobar segment III focal lesion eliciting high T2 signal with central hypo-intense scar. B axial diffusion and C ADC images show no diffusion restriction with DWI-ADC value 1.51 D Axial DTI gray scale image, E DTI-ADC map and F FA map: the DTI-ADC value was 1.57 and the FA value was low = 0.26 suggestive of benign nature. G non-contrast T1 H arterial phase and I delayed phase of the dynamic study showed homogenous arterial enhancement with enhancement of the central scar in the delayed phase. The lesion was categorized as LR-3. Imaging features were suggestive of FNH which is proved by histopathology
An overall significance difference of FA, DTI-ADC and DWI-ADC values among the different lesions was found by using ANOVA test; with the test statistic was 4.820, 22.318 and 6.745 with a significant P value of < 0.001 for the FA, DTI-ADC and DWI-ADC, respectively.
-
G.
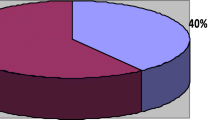
Evaluation of the FA, DTI-ADC and DWI-ADC values in the discriminations between benign and malignant lesions
Figure 6 and Table 5 show that 1. FA values had AUC of 73.7% with 95% confidence interval ranges between 61.7 and 85.8%, the sensitivity was 87.1%, and the specificity was 73.9% and cut-off value at 0.345 with a significant P value of < 0.001. 2. DTI-ADC values had AUC of 84.5%, 95% confidence interval ranges between 75.2 and 93.9%, the sensitivity was 88.7% and the specificity was 88.3% and cut-off value of 0.905 with significant P value of < 0.001. 3. DWI-ADC values had an AUC of 79.7%, 95% confidence interval ranges between 69.6 and 89.8%, the sensitivity was 78.5% and the specificity was 68.7% producing a significant Pvalue of < 0.001. We could not determine cut-off ADC value. So we concluded that DTI-ADC showed the highest sensitivity and specificity followed by the FA, while the DWI-ADC showed the lowest sensitivity and specificity which is reflecting the better act of DTI than DWI in differentiation of benign and malignant lesions.
Discussion
This cross-sectional study including 95 HFL aimed to assess the benefits of Liver DTI in the characterization and differentiation between benign and malignant focal lesions. This study showed that DTI-ADC has the highest sensitivity and specificity followed by the FA, while the DWI-ADC showed the lowest sensitivity and specificity in differentiation between benign and malignant lesions.
On searching the literature, only few researches discussed the role of DTI in characterization of HFL; moreover, we did not find similar researches that assess the relationship between diffusion and DTI parameters with LI-RADS category.
Li et al. [5] analyzed the DTI parameters of 18 cases of HCC and they found that FA and DTI-ADC values of the HCC were 0.42 and 1.30, respectively, which agreed with our results. Another larger study by Erturk et al. [10] was performed over 66 patients having 77 hepatic focal lesions including 13 cysts, 32 hemangiomas and 32 metastases. They found that the mean FA values of the cysts, hemangiomas and metastases were 0.20, 0.37 and 0.46, respectively. Meanwhile, the mean DTI-ADC values of the cysts, hemangiomas and metastases were 3.30, 2.23 and 1.62, respectively.
A substantial negative significant correlation was found between DTI-ADC and FA values which was in agreement with Erturk et al. [10] who found the relation between FA and DTI-ADC was negative, weak, and significant. Also a positive moderate significant correlation was found between FA values and the LI-RADS category while there was a substantial negative significant correlation between DTI-ADC values and the LI-RADS category and a moderate negative significant correlation between DWI-ADC values and the LI-RADS category.
Although similar studies correlating the DTI and DWI parameters with the LI-RADS category were not found, Erturk et al. [10] found that the mean FA values for metastasis were significantly higher than those of the cysts and hemangiomas, while the DTI-ADC values of metastatic lesions were significantly lower than those of cysts and hemangiomas which, to some extent, agree with our findings.
Finally, the current study showed that FA and DTI-ADC values had a significant role in differentiating benign and malignant HFL with FA cut-off value 0.345 showing 87.1% sensitivity and 73.9% specificity and DTI-ADC cut-off value 0.905 having 88.7% sensitivity and 88.3% specificity. This was partially agreed with the results of Karim et al. [11] who studied 77 hepatic focal lesions including 4 cysts, 12 hemangiomas, 12 HCC, 7 metastases, 2 cholangiocarcinoma, 1 dysplastic nodule, 1 epithelioid hemangioendothelioma. They found a cut-off FA value 0.29 with 95% sensitivity and 70% specificity and cut-off DTI-ADC value 1.42 with 95.7% sensitivity and 82.8% specificity. Also, Erturk et al. [10] found FA and DTI-ADC values had a significant role in the differentiation of the metastases from cysts and hemangiomas with FA cut-off value 0.31 having 56.2% sensitivity and 80% specificity and estimated DTI-ADC cut-off value 1.82 having 87.5% sensitivity and 84.4% specificity. Our hypothesis for the better act of DTI than conventional DWI could be explained by the more gradient directions used for DTI acquisition allowing for better averaging and more accurate ADC measurement.
Limitations of this study
The study design was a cross-sectional analytic type which limit the ability for selection of specific types of HFL. Also, the sample size was small compared to the variety and the heterogeneity of the lesions which lead to reduction of the power of statistical analysis. The standard of reference was not based on histopathology for all cases due to ethical and practical difficulties in performing biopsies in all cases. The FA and DTI-ADC maps can be noisy due to presence of physiological motion like respiration and bowel motion. Finally, a single radiologist assessed the images and calculated the ADC and FA of the different lesions yet we believed that did not affect the accuracy of the results.
Recommendations
L-DTI can be included in DCE-MRI of the liver for better tissue characterization with no much time added to the MRI scan. Further studies with larger number of cases and pathological confirmation are recommended for better assessment of the value of L-DTI and whether it can replace the conventional DWI or not.
Conclusions
Liver DTI can be included in liver MRI studies for better tissue characterization as it may perform better than conventional DWI by using the DTI-ADC and FA values which showed higher sensitivity and specificity in the differentiation between benign and malignant lesions compared to conventional DWI.
Availability of data and materials
All the datasets used and analyzed in this study are available with the corresponding author on reasonable request.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under the curve
- DTI:
-
Diffusion tensor imaging
- DWI:
-
Diffusion weighted imaging
- EPI:
-
Echo planar imaging
- FA:
-
Fraction of anisotropy
- FNH:
-
Focal nodular hyperplasia
- HFL:
-
Hepatic focal lesion
- L-DTI:
-
Liver diffusion tensor imaging
- TACE:
-
Transcatheter arterial chemoembolization
- LI-RADS:
-
Liver Imaging Reporting and Data System
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SOR:
-
Standard of reference
- THID:
-
Transient hepatic intensity difference
References
Elsayes KM, Kielar AZ, Elmohr MM, Chernyak V, Masch WR, Furlan A, Marks RM, Cruite I, Fowler KJ, Tang A, Bashir MR (2018) White paper of the society of abdominal radiology hepatocellular carcinoma diagnosis disease-focused panel on LI-RADS v2018 for CT and MRI. Abdom Radiol 43(10):2625–2642
Rashed WM, Kandeil MAM, Mahmoud MO, Ezzat S (2020) Hepatocellular carcinoma (HCC) in Egypt: a comprehensive overview. J Egypt Natl Canc Inst 32(1):1–11
Wang YT, Li YC, Kong WF, Yin LL, Pu H (2017) Diffusion tensor imaging beyond brains: applications in abdominal and pelvic organs. World J Meta-Anal 5(3):71–79
Girometti R, Maieron M, Lissandrello G, Bazzocchi M, Zuiani C (2015) Test–retest reliability of diffusion tensor imaging of the liver at 3.0 T. La Radiol Med 120(6):489–497
Li X, Liang Q, Zhuang L, Zhang X, Chen T, Li L, Liu J, Calimente H, Wei Y, Hu J (2015) Preliminary study of MR diffusion tensor imaging of the liver for the diagnosis of hepatocellular carcinoma. PLoS ONE 10(8):e0135568
Lanzman RS, Wittsack HJ (2017) Diffusion tensor imaging in abdominal organs. NMR Biomed 30(3):e3434
American College of Radiology (2018) CT/MRI LI-RADS v2018 core. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/CT-MRI-LI-RADS-v2018
Zhong X, Guan T, Tang D, Li J, Lu B, Cui S, Tang H (2021) Differentiation of small (≤ 3 Cm) hepatocellular carcinomas from benign nodules in cirrhotic liver: additive value of MRI-based radiomics analysis to LI-RADS version 2018 algorithm. BMC Gastroenterol 21(1):1–10
Barabino M, Gurgitano M, Fochesato C, Angileri SA, Franceschelli G, Santambrogio R, Mariani NM, Opocher E, Carrafiello G (2021) LI-RADS to categorize liver nodules in patients at risk of HCC: tool or a gadget in daily practice? Radiol Med (Torino) 126(1):5–13
Erturk SM, Ichikawa T, Kaya E, Yapici O, Ozel A, Mahmutoglu AS, Basak M (2014) Diffusion tensor imaging of cysts, hemangiomas, and metastases of the liver. Acta Radiol 55(6):654–660
Karim MA, Nehad MF, Tharwat M (2021) Characterization of Hepatic focal lesions by diffusion tensor imaging and how far it can predict post-treatment response? Med J Cairo Univ 89(June):1263–1273
Acknowledgements
Not applicable.
Funding
Not applicable (no funding).
Author information
Authors and Affiliations
Contributions
BEM put the idea of the study, performed the MRI assessment and manuscript editing. LIM participated in the study design and performed the MRI assessment. RMS involved in clinical assessment of the patients. MY involved in data collection, involved in MRI assessment and performed the statistical analysis. IMI participated in MRI assessment and manuscript editing. HSW is Editor of the manuscript and involved in MRI assessment. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was signed by all patients before the MRI examination. The study is approved by the medical committee of the faculty of medicine Cairo university at December 2019. Reference number: MD-169-2019.
Consent for publication
All adult patients included in this research (≥ 18 years of age) gave written informed consent to publish the data contained within this study. If the patient was younger than 18 years or unconscious and consent for publication was requested, written informed consent for the publication of data was given by his/her parent or legal guardian.
Competing interest
The authors declare that they have no financial or non-financial competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmoud, B.E., Metwally, L.I.A., Salama, R.M. et al. Does liver diffusion tensor imaging (L-DTI) has a role in differentiation of hepatic focal lesions? Analytic study for assessment of the value of L-DTI in differentiating hepatic focal lesions according to LI-RADS. Egypt J Radiol Nucl Med 53, 154 (2022). https://doi.org/10.1186/s43055-022-00830-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00830-z