Abstract
Background
Accurate breast cancer size is crucial for staging and an important prognostic factor in patient management. Therapeutic decisions heavily depend on tumor size detection by radiological imaging. The purpose of our prospective comparative study is to compare the diagnostic accuracy of different sonomammographic breast imaging modalities, namely DM, DBT, CESM, 2D US and 3D US in the preoperative tumor size measurement.
Results
CESM, 3D US and 2D US achieved moderately strong correlation with the pathological size measurements, while (DM) and (DBT) showed fair correlation with the pathology. CESM showed the highest correlation coefficient (0.789), while (DBT) showed the lowest correlation coefficient (0.411). Regarding the agreement, there was good agreement of the size measured by CESM, 3D US and 2D US with the pathology as the ICC was (0.798), (0.769) and (0.624), respectively. The highest agreement with the pathology was achieved with CESM. The agreement of the size measured by (DM) and (DBT) with the pathology was moderate as the ICC was (0.439) and (0.416), respectively. The lowest agreement was achieved with the size measured by (DBT).
Conclusions
CESM and 3D US are more superior to DM, 2D US and DBT regarding preoperative size measurement. 3D US can be used as preoperative noninvasive technique, especially in patients with impaired renal function who cannot tolerate CESM.
Similar content being viewed by others
Background
Globally, breast cancer is the most common female malignancy. It was responsible for 24% of new cancer cases and 15% of cancer deaths in 2018. Africa shows the highest case fatality ratio [1].
Tailoring individualized treatment strategies for each patient is the current standard level of care. To help the treating physician and the patient reach an optimum decision regarding treatment, the tumor load and biology (pathology, biomarkers and gene expression) should be thoroughly evaluated. The tumor load is assessed through loco-regional and systemic extent. The loco-regional extent includes size, multifocality/centricity and lymph node status [2].
Accurate size measurement of cancerous breast lesions is crucial, especially when breast cancer pathology is proven. Precise lesion size measurement is important for optimal management decisions and essential for the detection of patient’s response to neoadjuvant chemotherapy and a relevant prognostic factor [3].
According to European society of Medical Oncology, digital mammography (DM) and ultrasound (US) are the standard preoperative imaging modalities for breast cancer. They are used to measure the tumor size which is an important diagnostic and prognostic factor in disease management. However, the inevitable problem of tissue overlap in mammography prevents the accurate estimation of tumor size especially in dense breasts. This can be partly rectified using two-dimensional ultrasonography (2D US). But again, the size measurement could be affected by the background parenchymal echotexture resulting in over- or underestimation of the tumor size [4, 5].
By visualizing the breast lesions in the axial and coronal planes, three-dimensional ultrasonography (3D US) allows an increased accuracy in size assessment. Moreover, it produces a tumor volume that can be saved and revisited at any time by any radiologist not just the operator. This feature overcomes the operator dependency that is encountered with 2D US examination [6].
Digital breast tomosynthesis (DBT) is a three-dimensional (3D) modification of DM. It overcomes the problem of tissue overlap by producing multiple slices of the breast that allow thorough examination of the lesions, thus allowing better assessment of tumor size and margins [7].
Contrast-enhanced spectral mammography (CESM) uses contrast material to highlight the lesions on mammography. The images are processed to produce an image with suppressed parenchymal enhancement and emphasized pathological enhancement. Therefore, it can be used, to measure tumor size, as well as to assess tumor multiplicity. It has also been proven to be especially useful in the assessment of edematous breasts [8, 9].
The objective of our study was to compare the diagnostic performance of different sonomammographic breast imaging modalities, namely DM, 2D ultrasound, DBT, CESM and handheld 3D US, in the assessment of preoperative tumor size which can alter the patient management. A preoperative evaluation of the size by imaging can help to decrease the incidence of residual and recurrent lesions.
Methods
This is a prospective comparative study comparing the role of digital mammography (DM), two-dimensional ultrasound (2D US), contrast-enhanced spectral mammography (CESM), three-dimensional ultrasound (3D US) and digital breast tomosynthesis (DBT) in the detection of the size of breast malignant lesions using postoperative histopathological analysis as the gold standard.
The study included 147 patients with 149 breast lesions (two cases have bilateral unifocal breast lesions) attended our breast imaging unit during the period from January 2020 to August 2021 with symptomatic (135) breast lesions as well asymptomatic (14) breast lesions. Breast lesions classified as BIRADS 6 were included. No specific age group selection was applied.
Patients with impaired renal functions, with multicentric or multifocal breast lesions, known allergic reaction to contrast material, and pregnant women, were excluded from our study, as well as patients receiving preoperative neoadjuvant chemotherapy.
All patients initially underwent digital mammography (DM), two-dimensional ultrasound (2D B mode US) and ultrasound-guided biopsy as the baseline imaging. Afterward, breast lesions classified as BIRADS 6 were subjected to 3D US examination followed by DBT and finally CESM. The breast lesions were assessed regarding the size measured in cms in the greatest dimension including tumor spicules. The results were compared to the postoperative pathology as the reference standard.
Ultrasound technique
2D B-mode ultrasound
2D B-mode US was performed using Philips iU22 xMatrix ultrasound system with L 12–5 transducer. The breast quadrants examination was done in a radial pattern, and skin to pectoral fascia depth was fully examined. Axillary lymph nodes were then examined.
The examination criteria included the lesion size and presence of spicules, desmoplastic reaction or calcifications if present.
3D ultrasound
3D US was performed (targeted on the affected breast) using Philips iU22 xMatrix ultrasound system twice, first using L 12-5 probe by manually sweeping the lesion for surface rendering. After that, MPR images and volume acquisition were performed using X6-1 pure wave xMatrix transducer. Lesions were viewed in the axial, sagittal and coronal planes.
Technique of DM and DBT
Patients were examined by Senographe 2000 D full-field digital mammography Essential GE Healthcare. Standard two projections (CC and MLO) views were obtained for digital mammography. Similar views were acquired for DBT in a step-and-shoot tube motion, a complete stop for each of the nine exposures per each view. SenoClaire uses ASiRDBT, an iterative reconstruction algorithm that yields full-field digital mammography (FFDM)-like images. Images are then seen through tomosynthesis planes and slabs where dedicated tools to review tomosynthesis data sets such as cine loop and V-Preview reconstructed images were used.
Technique of CESM
The examination consists of an intravenous injection of an iodinated contrast agent (Omnipaque, 300 mg I/ml) at a dose of 1.5 ml/kg (maximum dose of 120 ml) through a catheter introduced in the ante-cubital vein. This is followed by a 2-min wait, and afterward, both breasts are imaged in the standard mammographic views. Each view is obtained in low- and high-energy images. Low-energy images were acquired at peak kilovoltage values ranging from 26 to 31 kVp, which is below the k-edge of iodine, and they resemble standard mammography. High-energy images were acquired at 45–49 kVp, which is above the k-edge of iodine. Subtraction of both high and low images suppresses the background parenchyma and highlights the areas of contrast uptake.
Image analysis
A subjective assessment using Image Diagnostic Mammography Workstation was done. The type of findings depicted on mammography, DBT were reported as regards the size of the pathological lesions, extension and calcifications.
The subtracted CESM images were reviewed using reading criteria based on the size of the mass/non-mass enhancement.
The ultrasound images were reviewed to detect the size of the lesions taking into consideration the long spicules as well as the extension and calcifications.
All techniques were performed by two experienced consultant’s radiologists, with more than 10 years of experience in breast imaging. The definitions of the statistical terms provided in the ACR BIRADS glossary were adopted in this study.
Sample size and statistical methods
The software was used for sample size calculation: G*power version 3.0.10. According to Yamakanamardi and Hiremath (XX), the MMG combined with SMG had a sensitivity of 90.4% and specificity of 82.4%. Assuming a disease prevalence of 50%, an alpha error of 5% and an acceptable precision of 10%, the calculated sample size was 125 patients with accounting for 10% dropout rate.
Data were coded and entered using the statistical package for the Social Sciences (SPSS) version 26 (IBM Corp., Armonk, NY, USA). Data were summarized using mean, standard deviation, median, minimum and maximum in quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. Correlations between quantitative variables were done using Spearman correlation coefficient [10]. Testing for agreement between size measured by pathology and by different methods was done using the intraclass coefficient (ICC) and Cronbach’s alpha reliability coefficient with their 95% confidence interval (95%CI) [11]. P values less than 0.05 were considered as statistically significant.
Value of ICC | Strength of agreement |
|---|---|
< 0.20 | Poor |
0.21–0.40 | Fair |
0.41–0.60 | Moderate |
0.61–0.80 | Good |
0.81–1.00 | Very good |
Results
The current study included 147 patients with 149 suspicious unifocal breast lesions; two patients have bilateral unifocal breast lesions. Out of the 149 lesions, 80 lesions were in the left breast and 69 lesions were in the right breast.
Age of the patients ranged from 25 to 70 years with mean age 49.7 ± 11.5 SD. The most prevalent pathology was IDC (n = 123/149, 82.6%), followed by ILC (n = 18/149, 12.1%), mixed (n = 6/149, 4%), and finally mucinous carcinoma (n = 2/149, 1.3%).
Out of the 149 breast lesions in the 147 patients, (n = 14/149, 9.4%) were incidentally discovered during screening and (n = 135/149, 90.6%) were discovered during diagnostic study. [(127/149, 85.2%) were palpable masses, (2/149, 1.3%) were recurrent masses, and (6/149, 4.1%) were masses for follow-up.]
All the patients underwent digital mammography (DM), 2D and 3D ultrasound (US), contrast-enhanced spectral mammography (CESM) and digital breast tomosynthesis (DBT). Size of the breast lesion was measured in cms in the greatest dimension including tumor spicules and compared to the postoperative pathology.
The range, mean and SD of the size of the breast lesions as measured by the different imaging modalities compared to the postoperative pathology are shown in Table 1.
The mean of the size measured by DM was 6.37 ± 2.28 SD, the mean of the size measured by DBT was 6.31 ± 2.08 SD, the mean of the size measured by CESM was 4.64 ± 1.97 SD, the mean of the size measured by 2D US was 3.38 ± 1.96 SD, and the mean of the size measured by 3D US was 3.23 ± 1.89 SD. The mean of the postoperative pathology size was 4.78 ± 2.38 SD.
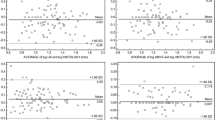
Correlation with pathology
Comparison of the lesion size by different modalities of imaging versus pathology showed that CESM, 3D US and 2D US achieved moderately strong correlation with the pathological size measurements, while (DM) and (DBT) showed fair correlation with the pathology. CESM showed the highest correlation coefficient (0.789), while (DBT) showed the lowest correlation coefficient (0.411), and all the modalities showed statistically significant results with p value < 0.001 (Figs. 1, 2 and 3). The results are shown in Table 2.
A 64-year-old female patient presented with left breast lump. a and b Digital mammography of the left breast in CC and MLO views showed a LOQ spiculated mass with maximum dimension of 2.4 cm. c 2D US showed 3–4 O’clock spiculated, hypoechoic solid mass lesion, and maximum dimension of 1.53 cm. d 3D US in coronal plane revealed the irregularity and spiculations. Maximum dimension of the tumor was 1.57 cm. e and f DBT in CC and MLO views showed a spiculated lesion, and maximum dimension is 3.06 cm because of the extended spicules anteriorly and posteriorly. g and h CESM in MLO and CC views showed a single lesion of faint heterogeneous enhancement (the spicules did not show any enhancement) and maximum dimension of 1.8 cm. Postoperative pathology revealed IMC with maximum dimension of 1.5 cm
A 53-year-old patient presented with right breast lump. a and b DM in CC and MLO views showed UIQ irregular mass and maximum dimension of 3.6 cm. c 2D US revealed a spiculated mass lesion with marked desmoplastic reaction and maximum dimension of 2.1 cm. d 3D US revealed spiculated lesion and maximum dimension of 2.7 cm. e and f DBT in CC and MLO views revealed spiculated lesion and maximum dimension of 4 cm. g and h CESM revealed heterogeneously enhancing mass lesion and maximum dimension of 2.7 cm. Postoperative pathology revealed a single tumor, IDC, with maximum dimension of 2.5 cm
Agreement with the pathology (Table 3)
There was good agreement of the size measured by CESM, 3D US and 2D US with the pathology as the ICC was (0.798), (0.769) and (0.624), respectively. The highest agreement with the pathology was achieved with CESM. The agreement of the size measured by (DM) and (DBT) with the pathology was moderate as the ICC was (0.439) and (0.416), respectively. The lowest agreement was achieved with the size measured by (DBT).
Discussion
Together with clinical examination, DM and 2D US are used as the basis for initial diagnosis and staging of breast cancer. Although very useful in fatty breasts, its results can be compromised in dense breasts where tissue overlap can mask an underlying lesion. Limiting factors of 2D US include operator dependency and difficulty of accurate size measurement in the AP plane especially in lesion with strong posterior acoustic shadowing [3, 12].
In the current work, we compared the diagnostic performance of five different breast imaging modalities in the preoperative tumor size measurement in 149 breast lesions. We compared the correlation and agreement of tumor size—as measured by DM, 2D US, 3D US, DBT and CESM—to the postoperative pathology.
Our results showed that highest correlation and agreement were achieved by CESM. It showed the highest correlation coefficient (0.798) and highest ICC (0.789). Several studies discussed the role of CESM in the preoperative staging of breast cancer especially in size measurement. In concordance with our results, Youn et al. [13] concluded that CESM achieved higher agreement with the size than MG, with ICC 0.907 compared to 0.820, respectively. This was especially highlighted in the CC view.
In agreement with this study’s results, Lobbes et al. [14] and another study conducted in 2014 [15] achieved the highest pathology size correlation with CESM. Although other studies suggested that sizes measured by both CESM and MG were comparable, MG resulted in more overestimation of tumor size [16].
Bozzini et al. [17] suggested that both CESM and 2D US can measure tumor size in concordance with pathology 64.6% and 62%, respectively, and both were significantly better than MG (45.2%) in size measurement. These results are keeping with our work, where both CESM and 2D US performed better than MG.
Another small study performed on 22 patients came to the conclusion that CESM was more accurate than 2D US in preoperative tumor size measurement [18].
These results are also consistent with our work. We also suggest CESM performed better than 2D US regarding size measurement, showing better correlation and agreement with the pathology size.
In our study, the lowest correlation and agreement were noticed with DBT which tended to overestimate the size. These results may differ from previous studies that showed good correlation between DBT and pathology size [19,20,21]. A possible explanation in our study is that the tumor spicules—that are more evident on DBT—were included in size measurement.
A more recent study performed by Girometti et al. [22] compared the performance of CESM to DM + DBT in the preoperative setting. In concordance with our results, they concluded that although both CESM and DM + DBT showed comparable size performance, CESM still showed higher agreement with the pathology size, especially in less experienced readers.
In our study, the correlation coefficient and ICC by 2D US was (0.617) and (0.624).
On comparing 2D US to MG, our results showed better agreement with 2D US. Similar findings were suggested by Leddy et al. [12] who suggested US allowed more accurate tumor size measurement than DM and MRI.
In our study, close results to CESM were achieved by 3D US with correlation coefficient (0.782) and ICC (0.769). Few studies discuss the role of 3D US in the preoperative tumor size assessment.
Clauser et al. [23] measured the greatest dimension and the volume of the preoperative tumor using 2D and 3D US as well as MRI. Similar to our study, they concluded that both 2D and 3D US show good concordance with the pathology at 0.79 for 3D US and 0.82 for 2D US.
Helal et al. [24] compared the diagnostic performance of CESM and 3D US in preoperative staging including size, multiplicity and peritumoral stromal invasion. According to their work, both CESM and 3D US were the most accurate regarding size measurement. However, 3D US showed the highest correlation.
Our study had few limitations. First is the small number of patients with the poor representation of different breast cancer pathologies, especially ILC. Second, the inter-reader variability was not measured.
Conclusions
Preoperative tumor size measurement is an important decision-making information. Although DM and 2D US are the baseline imaging modalities used to measure preoperative tumor size, better results could be reached through other modalities. CESM and 3D US are more superior to DM, 2D US and DBT regarding size measurement. 3D US can be used as preoperative noninvasive technique, especially in patients with impaired renal function who cannot tolerate CESM.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACR:
-
American College of Radiology
- BIRADS:
-
Breast Imaging Reporting and Data System
- CC:
-
Craniocaudal
- CESM:
-
Contrast-enhanced spectral mammography
- Cm:
-
Centimeter
- DBT:
-
Digital breast tomosynthesis
- DM:
-
Digital mammography
- ICC:
-
Intraclass coefficient
- IDC:
-
Invasive ductal carcinoma
- IMC:
-
Invasive micropapillary carcinoma
- MG:
-
Mammography
- MLO:
-
Mediolateral oblique
- SD:
-
Standard deviation
- 2D US:
-
Two-dimensional ultrasound
- 3D US:
-
Three-dimensional ultrasound
References
Heer E, Harper A, Escandor N, Sung H, McCormack V, Fidler-Benaoudia MM (2020) Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob Heal 8(8):e1027–e1037. https://doi.org/10.1016/S2214-109X(20)30215-1
Cardoso F et al (2019) Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 30(8):1194–1220. https://doi.org/10.1093/annonc/mdz173
Wienbeck et al (2019) Breast lesion size assessment in mastectomy specimens, Correlation of cone-beam breast-CT, digital breast tomosynthesis and full-field digital mammography with histopathology. Medicine 98:37
Mokhtar O, Mahmoud S (2014) Can contrast enhanced mammography solve the problem of dense breast lesions? Egypt J Radiol Nucl Med 45(3):1043–1052. https://doi.org/10.1016/j.ejrnm.2014.04.007
Ko KH, Son EJ, Kim IW (2018) Accuracy of ultrasound for preoperative assessment of tumor size in patients with newly diagnosed breast cancer: is it affected by the background parenchymal echotexture? J Ultrasound Med 37(11):2621–2630. https://doi.org/10.1002/jum.14622
Candelaria RP, Hwang L, Bouchard RR, Whitman GJ (2013) Breast ultrasound: current concepts. Semin Ultrasound CT MRI 34(3):213–225. https://doi.org/10.1053/j.sult.2012.11.013
Svahn TM et al (2012) Breast tomosynthesis and digital mammography: a comparison of diagnostic accuracy. Br J Radiol. https://doi.org/10.1259/bjr/53282892
Badr S, Laurent N, Régis C, Boulanger L, Lemaille S, Poncelet E (2014) Dual-energy contrast-enhanced digital mammography in routine clinical practice in 2013. Diagn Interv Imaging 95(3):245–258. https://doi.org/10.1016/j.diii.2013.10.002
ElSaid NAE, Farouk S, Shetat OMM, Khalifa NM, Nada OM (2015) Contrast enhanced digital mammography: is it useful in detecting lesions in edematous breast? Egypt J Radiol Nucl Med 46(3):811–819. https://doi.org/10.1016/j.ejrnm.2015.04.002
Chan YH (2003) Biostatistics 104: correlational analysis. Singap Med J. 44(12):614–619
Rankin G, Stokes M (1998) Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehab 12(3):187–99
Leddy R et al (2016) Comparative accuracy of preoperative tumor size assessment on mammography, sonography, and MRI: is the accuracy affected by breast density or cancer subtype? J Clin Ultrasound 44(1):17–25. https://doi.org/10.1002/jcu.22290
Youn I et al (2019) Contrast enhanced digital mammography versus magnetic resonance imaging for accurate measurement of the size of breast cancer. Br J Radiol. https://doi.org/10.1259/bjr.20180929
Lobbes MBI et al (2015) The quality of tumor size assessment by contrast-enhanced spectral mammography and the benefit of additional breast MRI. J Cancer 6(2):144–150. https://doi.org/10.7150/jca.10705
Fallenberg EM et al (2014) Contrast-enhanced spectral mammography: does mammography provide additional clinical benefits or can some radiation exposure be avoided? Breast Cancer Res Treat 146(2):371–381. https://doi.org/10.1007/s10549-014-3023-6
Luczyńska E, Heinze-Paluchowska S, Dyczek S, Blecharz P, Rys J, Reinfuss M (2014) Contrast-enhanced spectral mammography: comparison with conventional mammography and histopathology in 152 women. Korean J Radiol 15(6):689–696. https://doi.org/10.3348/kjr.2014.15.6.689
Bozzini A et al (2020) Clinical performance of contrast-enhanced spectral mammography in pre-surgical evaluation of breast malignant lesions in dense breasts: a single center study. Breast Cancer Res Treat 184(3):723–731. https://doi.org/10.1007/s10549-020-05881-2
Blum KS, Rubbert C, Mathys B, Antoch G, Mohrmann S, Obenauer S (2014) Use of contrast-enhanced spectral mammography for intramammary cancer staging. Acad Radiol 21(11):1363–1369. https://doi.org/10.1016/j.acra.2014.06.012
Krammer J et al (2017) Value of additional digital breast tomosynthesis for preoperative staging of breast cancer in dense breasts. Anticancer Res 37(9):5255–5261. https://doi.org/10.21873/anticanres.11950
Förnvik D et al (2010) Breast tomosynthesis: accuracy of tumor measurement compared with digital mammography and ultrasonography. Acta radiol 51(3):240–247. https://doi.org/10.3109/02841850903524447
Luparia A et al (2013) Accuracy of tumour size assessment in the preoperative staging of breast cancer: comparison of digital mammography, tomosynthesis, ultrasound and MRI. Radiol Medica 118(7):1119–1136. https://doi.org/10.1007/s11547-013-0941-z
Girometti R et al (2021) Multireader comparison of contrast-enhanced mammography versus the combination of digital mammography and digital breast tomosynthesis in the preoperative assessment of breast cancer. Radiol Medica 126(11):1407–1414. https://doi.org/10.1007/s11547-021-01400-5
Clauser P, Londero V, Como G, Girometti R, Bazzocchi M, Zuiani C (2014) Comparison between different imaging techniques in the evaluation of malignant breast lesions: can 3D ultrasound be useful? Radiol Medica 119(4):240–248. https://doi.org/10.1007/s11547-013-0338-z
Helal MH, Mansour SM, Salaleldin LA, Alkalaawy BM, Salem DS, Mokhtar NM (2018) The impact of contrast-enhanced spectral mammogram (CESM) and three-dimensional breast ultrasound (3DUS) on the characterization of the disease extend in cancer patients. Br J Radiol. https://doi.org/10.1259/bjr.20170977
Acknowledgements
We are really grateful because of our cooperation in managing this study. This study cannot be completed without the help and effort from this group members. We would thank all the patients included in this study.
Funding
The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NK and AH analyzed and interpreted the patient data regarding the breast lesions size measurement in the greatest dimension including tumor spicules. LH and SG revised all the data interpreted by other authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study had been approved by Kasr El-Aini Hospital, Research and Ethical committee.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in the figures.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kandil, N.M.M., Hashem, L.M.B., Gareer, S.W.Y. et al. Accuracy of different sonomammographic imaging modalities in assessment of breast tumor size. Egypt J Radiol Nucl Med 53, 133 (2022). https://doi.org/10.1186/s43055-022-00804-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00804-1