Abstract
Background
Magnetic resonance imaging is regarded as one of the most important markers for multiple sclerosis. It can detect lesions in order to establish dissemination in time and space, which would aid in the diagnosis. Two-dimensional FLAIR is a standard sequence in MS routine imaging because it suppresses cerebrospinal fluid signal, increasing contrast between lesions and CSF and improving white matter lesion detection. Newer 3D FLAIR sequences are expected to offer even more benefits, such as improved MS lesions detection and higher resolution due to thinner slice thickness. We aimed to compare the role of 3D Cube FLAIR imaging (versus standard 2D FLAIR) in the assessment of white matter lesions in MS patients, as well as to test the convenience of using maximum intensity projection (MIP) on 3D FLAIR images for faster and easier evaluation.
Results
This study included 160 MS patients. A 1.5 T routine brain MRI scan was performed, which included a 2D FLAIR sequence, followed by a 3D-FLAIR sequence. All images were analyzed after 3D-FLAIR images were reformatted into axial MIP images. Lesions were counted in each sequence and classified into supra-tentorial (periventricular, deep white matter, and juxta-cortical), and infra-tentorial lesions, with the relative comparison of lesions numbers on 3D-FLAIR and MIP versus 2D-FLAIR expressed as a percentage increase or decrease. 3D FLAIR can significantly improve MS lesion detection in all areas of the brain when compared with 2D FLAIR results. At 2 mm reformatting, there is no difference in MS lesion detection between sagittal 3D FLAIR and axial MIP reconstruction, implying that the MIP algorithm can be used to simplify lesion detection by reducing the number of images while maintaining the same level of reliability.
Conclusion
3D FLAIR sequences should be added to conventional 2D FLAIR sequences in the MRI protocol when MS is suspected.
Similar content being viewed by others
Background
MS is a common cause of neurological disorders developing in early to middle adulthood which has a complex etiology including both genetic and environmental elements [1]. The diagnosis of MS relies on neurological symptoms and signs, alongside evidence of the dissemination of CNS lesions in space and time. MRI is usually enough to confirm the diagnosis when characteristic lesions accompany a typical clinical presentation [2]. Sizes, shapes, and locations of MS lesions have great versatility. However, typically, they have an oval shape, a diameter greater than or equal to 3 mm, and gather close to the ventricles and in the corpus callosum, although juxta-cortical and infra-tentorial regions are also common sites of involvement [3].
MS lesions are typically presented with a high T2 signal. FLAIR is a T2-weighted sequence with CSF signal was removed; therefore, it increases the contrast between the lesions and the CSF and improves white matter lesion detection. For these properties, it has become a standard sequence for MS imaging [4].
FLAIR is a single-slab fast spin-echo (FSE) T2 FLAIR sequence. Modulated flip angle refocusing radiofrequency pulses are used to generate lengthy echo trains. This leads to slower signal decay when compared to conventional FSE sequences with constant flip angles of 180°. Thus, many more echoes can be used to generate the T2 image without causing extensive blurring and artifacts [5].
Newer MR sequences like three-dimensional (3D) FLAIR merge two positive imaging features, nullifying the signal of the cerebrospinal fluid to improve the detection of white matter lesions and providing better resolution due to smaller slice thickness [6]. Also, there is the additional advantage of multi-planar reformatting while using the 3D acquisition [7].
We aimed to compare the role of 3D Cube FLAIR imaging (versus standard 2D FLAIR) in the assessment of white matter lesions in MS patients, as well as to test the convenience of using maximum intensity projection (MIP) on 3D FLAIR images for faster and easier evaluation
Methods
Study designed
This study was designed as a prospective intra-individual comparative study (Intraindividual because we assessed the patients at two different situation 2D and 3D FLAIR). The study protocol approval by the ethical committee of our institution. All underlying MR images of the study were saved in the PACS of the authors institution. Patients: One hundred and sixty patients with MS (124 females and 36 males) with ages ranged between 17 and 50 years with a mean age of 31.5 years referred by neurologists to our radio-diagnosis department. The duration of the study was approximately 2 years, starting from December 2019 to October 2021 with definite MS diagnosed by International Panel on the diagnosis of multiple sclerosis (McDonald Criteria (revised)8). Any patients with pervious vascular, malignant or other CNS immunological disease were excluded from the study. Each patient underwent detailed history taking and examination to determine the disease duration and disabilities caused by MS. Expanded Disability Status Scale (EDSS) that represent the level of disability scores caused by MS at time of MRI examination were collected from the patient's records. As seen in Table 1 [9].
MRI imaging
All studies were done on a 1.5 T MRI unit with 20- channel-head-coils (GE healthcare, US). No special preparation is needed for the imaging except instructing the patient to remove any metal items like jewelry. Patient was in Supine position with headfirst., no contrast media injection is needed for this study unless indicated by the physician. Routine MRI brain study was performed including axial T1WI, axial, sagittal and coronal T2 WI. 2D FLAIR (repetition time (ms): 8000.echo time (ms): 120.inversion time (ms): 2000 plane: axial, with 5.5 mm slice thickness. acquisition time (min) 2.10). Single slab 3D cube FLAIR sequence (which is a single-slab FSE T2 FLAIR sequence, repetition time (ms): 6000 echo time (ms): 126 inversion time (ms), 1864 slice thickness (mm),1.6 continuous lane, sagittal acquisition time (min), 5.21) were added. Sequences parameters are listed in Table 2. Reformatting techniques were applied on 3D FLAIR sagittal images to produce the axial FLAIR MIP images using Radi Ant Dicom Viewer software (version 2020.2.3) with 2 mm reconstruction thickness for easier and faster comparison with axial 2D FLAIR imaging results. The details of the imaging done, its technique and any expected risks were explained to the patients and an informed consent was obtained. Approval by the ethical committee for research before initiating this study. (NO: 33393/10/19).
Image analysis
Images analysis were independently done by two neuroradiologist with 10 and 12 years of experience in neuroradiology, respectively. Observers were blinded by EDSS scoring. Lesions detected in both axial T2 D and its 3D MIP images were counted and classified into: Infra-tentorial lesions which located in or along the surface of the cerebellum and brain stem, Supra-tentorial lesions either periventricular lesions which touching the ventricles, deep white matter lesions (DWM) or juxta-cortical lesions which were within the subcortical white matter immediately adjacent to the grey matter and hyper intense lesions were only counted once they appear on multiple contiguous slices with a size equal or more than 2 mm.
Statistical analysis
The analysis of brain lesions on the different pulse sequences were performed as the numbers of lesions were expressed as range, mean, standard deviation and median. The comparison of the numbers of lesions on 2D FLAIR versus 3D FLAIR were expressed as percentage increase or decrease in the number of detected brain lesions. All calculations were performed by the SPSS software package. P values ≤ 0.05 were considered as statistically significant. Wilcoxon signed-rank test was also applied which is a non- parametric test that is used when the tested data were not normally distributed. Inter-observer reliability was analyzed using two-way mixed single measure intraclass correlations (ICC).
Results
This study included 160 patients diagnosed with MS according to their clinical presentation and the typical conventional MRI findings, and then they were further evaluated by 3D Cube FLAIR MR Sequence. They were 142 females and 36 males with ages ranging between 17 and 50 years with a mean age of 33.4 years.
Most of the patients (92.5%) have relapsing remittent MS (RRMS) except 8 cases with secondary progressive MS (SPMS) and only four cases with clinically isolated syndrome (CIS) with EDSS ranging from 1 to 6.5 with a mean score of 3.4 and a standard deviation of 1.4. The duration of the disease ranges from 1 month to 18 years with a mean duration of 5 years. (Table 3)
The patients showed a wide variety of neurological symptoms including motor, sensory, visual, cerebellar and brain stem symptoms as demonstrated in (Table 4).
The degree of disability was found to be correlated with the numbers of T1 (black hole) lesions and infra-tentorial T2 lesions. Higher EDSS scores were associated with higher numbers of either or both lesions.
The detected lesions were mostly in the supra-tentorial regions (juxta-cortical, periventricular and DWM) 2120 of total 2200 in 2D and 3176 of total 3408 in 3D, and in all three locations, 3D FLAIR sequence showed significantly more lesions than 2D FLAIR.
The 3D FLAIR detected more lesions (1128) in the juxta-cortical region versus 560 lesions seen by the 2D FLAIR, the 3D showed a statistically significant difference compared to 2D FLAIR (p = < 0.001) with a percentage increase of 101.4%.
The 3D FLAIR detected 896 periventricular lesions, while the 2D FLAIR detected 696 lesions. The 3D FLAIR showed a statistically significant difference compared to 2D FLAIR (p = < 0.001) with a percentage increase of 28.7%.
As for the DWM region, the 3D FLAIR detected 1152 lesions, while the 2D FLAIR detected 864 lesions. The 3D FLAIR showed a statistically significant difference compared to 2D FLAIR (p = < 0.001) with a percentage increase of 33.3%.
While the infra-tentorial lesions were detected in 48 patients in the 2D FLAIR sequence and 104 patients in the 3D FLAIR sequence. The 3D FLAIR showed higher detection rate of lesions with a percentage increase of 190% (80 lesions in 2D & 232 lesions in 3D).
At 2 mm reformatting, there is no difference in the detection of MS lesion between sagittal 3D FLAIR and axial MIP reconstruction, so MIP algorithm can be used to simplify lesion detection by reducing the number of images with the same degree of reliability. Summary of the study and the most important results are displayed in Table 5.
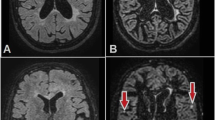
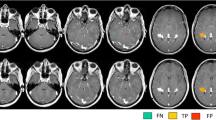
An example of one of the patients studied is displayed in (Figs. 1, 2, 3 and 4), which was a case of a 30 years old female patient, with RRMS for 6 years and an EDSS score of 5.5.
Infra-tentorial sections: the 3D FLAIR and axial MIP (green arrows at B and C) show a well delineated left cerebellar MS lesion that is not seen in 2D FLAIR (red arrow at A). A poorly seen lesion (encircled in red at A) is clearly demonstrated in axial MIP (encircled in green at C). Also, the sharp demarcation of the layers of the cerebellum is noted
Another example is A 19 years old female patient with RRMS for 18 months and an EDSS of 1.5 (Figs. 5 and 6).
Discussion
Multiple sclerosis is a chronic inflammatory, degenerative, demyelinating disorder of the CNS that is most prevalent in young adults. This disease is characterized by relapses of attacks affecting different areas of the brain, optic nerves, and spinal cord over time. It is the most common cause of disability in young adults after trauma [10].
In our present study, 3D Cube FLAIR sequence at 1.5 T was used alongside the conventional MRI sequences in the assessment of patients with MS to measure its value in the detection of supra-tentorial and infra-tentorial lesions and comparing the results of the 3D sequence and its axial MIP reconstruction with those of 2D FLAIR that is routinely used.
3D sequences have numerous advantages over 2D sequences. Images obtained by 3D sequences have isotropic voxel dimensions without inter-slice gap so it can be easily reformatted without affecting the image quality. In 3D images, the thinner slice thickness leads to an increased number of detected lesions. Furthermore, Cube FLAIR was shown to produce almost no CSF flow artifacts when applied in brain imaging which improves visualization of lesions in the infra-tentorial region. Detecting these lesions is very vital because they have major impact on clinical disability of MS patients [11].
Earlier, 3D sequences took long acquisition time as they were multi-slab mode, but that drawback was attuned by using single-slab mode [12]. In our study, although 3D-FLAIR sequence has a longer time (5:21 min) compared to (2:10 min) in 2D FLAIR sequence, it is not considered a disadvantage as the 3D sequence also allows axial, coronal, and sagittal reformatting.
2D and 3D FLAIR scans were compared, and lesions on each sequence were counted. Only hyper intense areas larger than 2 mm were calculated.
In current study, the detected lesions were mostly in the supra-tentorial regions (juxta-cortical, periventricular and DWM). 3D FLAIR sequence showed significantly more lesions than 2D FLAIR, that in keeping with Gramsch et al., [13] that state that adding 3D FLAIR sequence in standard MS protocols can considerably increase MS lesion detection and provide the possibility of an adequate replacement of both axial 2D FLAIR and mid-sagittal T2W sequences. This results also matched with Tawfik et al., [14] and Patzig et al., [12] who used 3 Tesla MRI machine.
Among the 160 patients, infra-tentorial lesions were detected in 48 patients in the 2D sequence and 104 patients in the 3D sequence. The 3D FLAIR showed higher detection rate of lesions with a percentage increase of 190% as the 2D-FLAIR was generally reported as less sensitive mostly due to CSF and blood inflow artifacts. The use of 3D FLAIR overcomes these issues because it can achieve homogeneous CSF suppression. Tawfik et al., [14] and Patzig et al., [12] also noted a 3D detection percentage increase of 80% and 140% respectively. A significant positive association between infratentorial lesions and higher EDSS score or clinical disability was noted as Almutairi et al., also observed [15].
The overall results in this study were compatible with the results reported by the other studies regarding the comparison between 2D FLAIR and 3D FLAIR sequences in the detection of MS lesions. However, there were some differences between the present study and other ones, including:
This study included 160 patients using 1.5 T GE MRI machine, While Tawfik et al, [14] studied 20 patients using Philips 1.5 T MRI scanner and Patzig et al, [12] studied 12 patients at 3 Tesla.
At 2 mm reformatting, there is no difference in the detection of MS lesion between sagittal 3D FLAIR and axial MIP reconstruction, so MIP algorithm can be used to simplify lesion detection by reducing the number of images with the same degree of reliability which is in agreement with what Bravo et al., [7] observed.
MIP 3D FLAIR sequence overcame the problem of small size cortical lesions and the partial volume effects with cerebrospinal fluid in the sulci. The significant higher numbers of detectable lesions in regions classified as juxtacortical using 3D FLAIR sequences compared to 2D sequences also argued for an integration of 3D FLAIR sequences into standard MRI protocols. The higher detection rate of hemispheric and infratentorial lesions and similar detection rate in the corpus callosum suggested that 3D FLAIR sequences could substitute both dual-echo sequences and sagittal T2W sequences. However, a replacement of the conventional MRI sequences by the newer one will certainly require critical reconsidering of MS diagnostics. 3D FLAIR sequence can detect smaller MS lesions started at sizes of one mm; this could have a non-negligible impact on the evaluation of a patient’s examination in terms of the revised McDonald criteria. The more sensitive MR sequences used, the earlier these criteria were met and the more significantly diagnosis differs between imaging centers because many sites use only conventional sequences.
Our study has some limitations: First, the results of the study are somewhat limited by the relatively small number of patients. Also, the results may be exclusive to the scanner and coil hardware used as no other systems were used or tested. Second, a low 1.5 Tesla field strength MRI machine was used. A 3 T or higher MRI would have enabled the detection of more lesions. Finally, because we did not correlate results to pathology specimens, we cannot be certain that all lesions detected were MS lesions. This would have implied post-mortem exams, which were not obtainable.
Conclusion
3D FLAIR sequences should be added to conventional 2D FLAIR sequences in the MRI protocol when MS is suspected as it provides better detection of MS lesions in all three planes in one acquisition. MIP reformatting algorithm can simplify MS lesions detection with the same degree of precision within a shorter interpretation time.
Availability of data and materials
All data generated or analyzed during our study are included in this published article.
Abbreviations
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional,
- BBB:
-
Blood brain barrier
- CIS:
-
Clinically isolated syndrome
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- DIS:
-
Dissemination in space
- DIT:
-
Dissemination in time
- DWM:
-
Deep white matter
- EDSS:
-
Expanded Disability Status Scale
- FA:
-
Fractional Anisotropy
- FLAIR:
-
Fluid-attenuated inversion recovery
- GE:
-
Gradient-echo
- GE:
-
General Electric
- GM:
-
Grey matter
- MIP:
-
Maximum intensity projection
- MRI:
-
Magnetic resonance imaging
- MS:
-
Multiple sclerosis
- RIS:
-
Radiologically isolated syndrome
- RRMS:
-
Relapsing–remitting MS
References
Rijnsburger M, Djuric N, Mulder IA et al (2021) Adipokines as immune cell modulators in multiple sclerosis. Int J Mol Sci 22(19):10845
Brownlee WJ, Hardy TA, Fazekas F et al (2017) Diagnosis of multiple sclerosis: progress and challenges. Lancet 389(10076):1336–1346
Chen JJ, Carletti F, Young V et al (2016) MRI differential diagnosis of suspected multiple sclerosis. Clin Radiol 71(9):815–827
Hemond CC, Bakshi R (2018) Magnetic resonance imaging in multiple sclerosis. Cold Spring Harb Perspect Med 8(5):1–21
Peltonen JI, Mäkelä T, Salli E (2018) MRI quality assurance based on 3D FLAIR brain images. MAGMA 6:689–699
Lecler A, Bouzad C, Deschamps R et al (2019) Optimizing 3D FLAIR to detect MS lesions: pushing past factory settings for precise results. J Neurol 266(11):2786–2795
Bravo P, Sánchez JJ, Ibáñez L et al (2014) A comparative MRI study for white matter hyperintensities detection: 2D-FLAIR, FSE PD 2D, 3D-FLAIR and FLAIR MIP. Br J Radiol 87(1035):1–5
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Şen S (2018) Neurostatus and EDSS Calculation with Cases. Noro Psikiyatr Ars 55(Suppl 1):S80–S83
Kara F, Göl MF, Boz C (2021) Determinants of disability development in patients with multiple sclerosis. Arq Neuropsiquiatr 79(6):489–496
Vos SB, Micallef C, Barkhof F et al (2018) Evaluation of prospective motion correction of high-resolution 3D-T2-FLAIR acquisitions in epilepsy patients. J Neuroradiol [Internet] 45(6):368–373
Patzig M, Burke M, Brückmann H, Fesl G (2014) Comparison of 3D Cube FLAIR with 2D FLAIR for multiple sclerosis imaging at 3 Tesla. Rofo 186(5):484–488
Gramsch C, Nensa F, Kastrup O et al (2015) Diagnostic value of 3D fluid attenuated inversion recovery sequence in multiple sclerosis. Acta radiol 56(5):622–627
Tawfik AI, Kamr WH (2020) Diagnostic value of 3D-FLAIR magnetic resonance sequence in detection of white matter brain lesions in multiple sclerosis. Egypt J Radiol Nucl Med 51(1):1–5
Almutairi AD, Hassan HA, Suppiah S et al (2020) Lesion load assessment among multiple sclerosis patient using DIR, FLAIR, and T2WI sequences. Egypt J Radiol Nucl Med 51(1):0–8
Acknowledgements
Staff member of Tanta University hospital especially radiology.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
RA correlated the study concept and design and had the major role in analysis, SZ collected data in all stage of manuscript, performed data for analysis and MKh supervised the study with significant contribution to design the methodology, manuscript revision and preparation. AZ correlated the finding with clinical finding and managed the cases. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consents taken from the patients, the study approved from ethical committee of faculty of medicine Tanta University number 136–2019.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zamzam, A.E.A., Aboukhadrah, R.S., Khali, M.M. et al. Diagnostic value of three-dimensional cube fluid attenuated inversion recovery imaging and its axial MIP reconstruction in multiple sclerosis. Egypt J Radiol Nucl Med 53, 119 (2022). https://doi.org/10.1186/s43055-022-00795-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00795-z