Abstract
Introduction
Trigeminal neuralgia is a neuropathic pain that occurs in the sensory supply region of the trigeminal nerve (V cranial nerve). The common etiology of trigeminal neuralgia is said to be vascular compression on the trigeminal nerve root. In our day-to-day practice, we see many asymptomatic patients having vascular loops around the trigeminal nerve root. We undertook this study to see the significance of nerve root compression by the vascular loop as a cause for trigeminal neuralgia.
Materials and methods
A total of 67 classical trigeminal neuralgia patients with NVC involving the trigeminal nerve as diagnosed on MRI brain sequences including FIESTA sequence were included in the study. NVC in all the patients were studied for the side, site of neurovascular contact of cisternal segment of the trigeminal nerve from the brainstem, deviation of nerve at NVC, atrophy of nerve, nature and origin of vascular loop causing NVC and correlated with TGN symptoms.
Results
Out of 67 patients studied, all of them (100%) had NVC on ipsilateral side and 26 patients (34%) had NVC at contralateral trigeminal nerve. Incidence of trigeminal neuralgia was most commonly seen between the 41 and 60 years age (64%) followed by 61–80 years with mean age of 55.6 years. Incidence in females (64%) was found to be more common than in males (35%). NVC was observed at the root entry zone (< 7 mm from brain stem) in 63 trigeminal nerves on symptomatic side and 5 trigeminal nerves on the asymptomatic side. NVC occurring at REZ on symptomatic side was found to be statistically significant with P < 0.001. Mean distance of NVC from brain stem at symptomatic side was 3.4 mm and was 8.4 mm in asymptomatic side NVCs. Atrophy was seen in 8 trigeminal nerves, all on symptomatic side and NVC occurring at root entry zone. No displacement of nerve root at the point of neurovascular contact was observed in our study. Most common vessel causing was found to be ipsilateral superior cerebellar artery followed by the ipsilateral anterior inferior cerebellar artery.
Conclusions
Neurovascular contact of trigeminal nerve occurring at the nerve root entry zone has a strong association with ipsilateral trigeminal neuralgia symptoms. In addition, the presence of the trigeminal nerve thinning is also associated with ipsilateral trigeminal neuralgia. With the increase in age, there are higher chances of association of NVC with ipsilateral trigeminal neuralgia symptoms.
Similar content being viewed by others
Introduction
Trigeminal neuralgia is a neuropathic pain that occurs in the sensory supply region of the trigeminal nerve (V cranial nerve). It is characterized by stereotyped attacks of paroxysmal, intense, sharp, and lancinating pain that may last from a split second up to 2 min. The prevalence of classical trigeminal neuralgia is 1–2 per 10,000 individuals [1]. The exact underlying etiology is unknown with multiple hypotheses being laid. Neurovascular conflict at the cisternal segment of trigeminal is the most widely accepted cause of trigeminal neuralgia [2].
The exact pathophysiology of the vascular contact causing the facial pain in cases of trigeminal neuralgia remains controversial, however, it is agreed that the vascular contact causing focal demyelination of the trigeminal nerve, more commonly observed at the root entry zone (REZ), leading to cross-talk between the one nerve fiber and another nerve fiber resulting in altered pain mechanisms, thus causing neuropathic pain [3]. The widely accepted definition of REZ is the length of the proximal cisternal segment of the trigeminal nerve which is centrally myelinated before transitioning into peripherally myelinated distal nerve segment [4]. The myelin of central and peripheral segments was derived from Schwann cells and oligodendroglia respectively. This results in more susceptibility to external compression resulting in hemifacial pain in the distribution of the trigeminal nerve. This susceptibility is not seen in the rest of the distal part of the trigeminal nerve. As per previous studies, the medial part of the trigeminal nerve root shows shorter central myelination as compared to the lateral part of the trigeminal nerve [5, 6]. There is marginal variation in the length of the REZ (3–7 mm) and the cisternal segment length [6].
MRI brain study is the first investigation of choice in patients with trigeminal neuralgia. The MRI sequences we used include MR axial T2, T1, DWI, GRE, Fast Imaging Employing Steady-state Acquisition (FIESTA), and MR angiography TOF sequence. This is a unique study wherein the correlation between classical trigeminal neuralgia and NVC of trigeminal nerve is evaluated.
Materials and methods
The study included patients referred from department of neurology, PESIMSR, Kuppam with clinical diagnosis of unilateral classical trigeminal neuralgia for the duration of 25 months from August 2019 to September 2021.
The exclusion criteria of our study were patients with cerebellopontine angle lesions, past history of microvascular decompression surgery, multiple sclerosis, trigeminal nerve sheath tumors, secondaries, meningiomas, skull-based lesion and patients with herpetic infection of trigeminal nerve (trigeminal herpes zoster).
In the department of neurology, the neurologist clinically examined and arrived at the clinical diagnosis of trigeminal neuralgia, which was made based on the diagnostic criteria of trigeminal neuralgia according to the beta-version of 3rd edition of the International Classification of Head ache Disorders (ICHD-3). These include:
-
A.
At least 3 attacks of unilateral facial pain fulfilling criteria B and C,
-
B.
Occurring in one or more divisions of trigeminal nerve, with no radiation beyond the trigeminal distribution,
-
C.
Pain has at least three of the following four characteristics: (1) Recurring in paroxysmal attacks lasting from a fraction of a second to 2 min; (2) Severe intensity; (3) Electric shock like shooting pain; (4) Precipitated by innocuous stimuli to effected side of face,
-
D.
No clinically evident neurological deficit, and
-
E.
Not better accounted for any other ICHD-3 diagnosis [7].
Such patients were referred to department of Radiodiagnosis, PESIMSR for MRI brain imaging. Our department has 1.5 Tesla GE Signa explore machine. MRI brain study was performed in these patients with routine sequences including MR axial T2, T1, DWI, GRE along with FIESTA and MR angiography TOF sequence. Imaging analysis was done in all three planes (coronal, axial, and sagittal) by a single radiologist with more than 5 years of experience in reporting MRI brain studies. Radiologist was not blinded to the clinical diagnosis. Radiologist evaluated both the trigeminal nerves in each case for the presence of NVC, side of occurrence of NVC, site of occurrence, the anatomical origin of the vascular loop causing NVC, displacement and atrophy of involved trigeminal nerves. Further age, sex characteristics of patients and side of patient’s symptoms were recorded. Ipsilateral NVC is defined as NVC occurring at the same side as that of patient’s clinical symptoms. Contralateral NVC is defined as NVC of trigeminal nerve observed on the contralateral side to that of patient’s clinical symptoms.
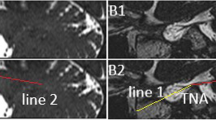
Neurovascular contact is defined as a vascular loop coming in contact with the trigeminal nerve. Whenever a vascular loop coming in close contact with the trigeminal nerve as observed in more than 1 plane, the diagnosis of NVC was made. No CSF signal must be observed between the nerve root and vascular loop interfaces for diagnosing a neurovascular contact (NVC).
Root entry zone (REZ) is the length of the proximal cisternal segment of the trigeminal nerve which is centrally myelinated before transitioning into peripherally myelinated distal nerve segment [4]. There is marginal variation in the length of the REZ (3–7 mm) and the cisternal segment length [6]. In our study, we took 7 mm of the proximal part of cisternal segment of trigeminal starting from its origin at pons as root entry zone. Any NVC occurring at this segment was considered as NVC occurring at root entry zone.
When there is no NVC on bilateral trigeminal nerves, these patients were considered idiopathic trigeminal neuralgia patients.
The displacement of nerve root is defined as buckling of trigeminal nerve at the site of occurrence of NVC. Atrophy of nerve root was a subjective diagnosis based on focal thinning (or reduced volume) of trigeminal nerve at the point of occurrence of NVC.
We used MS Excel 2007 version for data entry and SSPS 20 for statistical analysis. Chi-square test and Fischer's exact test were used to compare the changes in trigeminal nerves at the site of NVC between the ipsilateral and contralateral sides. P value < 0.05 was considered a statistically significant difference.
Results
A total of 76 patients with classical trigeminal neuralgia symptoms referred to our department for MRI brain imaging during this study period. 9 patients (12%) did not have neurovascular contact of trigeminal nerve (on both sides). So, a total of 67 (88%) patients who had neurovascular contact of trigeminal nerve were studied. Both ipsilateral and contralateral sides (134 trigeminal nerves) were evaluated for the presence of neurovascular contact. 67 patients (100%) had ipsilateral neurovascular contact of trigeminal nerve and 26 patients (34%) also had neurovascular contact of trigeminal nerve on the contralateral asymptomatic side. Neurovascular contact was found in 93 trigeminal nerves in our study.
None of the 76 patients had any MRI brain imaging findings of multiple sclerosis, nerve sheath tumors, dural-based tumors of Meckel’s cave, cerebellopontine angle lesions or cavernous sinus lesions.
Incidence of trigeminal neuralgia was most commonly seen between the 41 and 60 years age group with 43 cases (64%) in this group, 20 cases were between 61 and 80 years (30%) and 4 cases (6%) between 20 and 40 years (Fig. 1). Mean age of TGN patients was 55.6 years. No patients were of age below 20 years and above 80 years in our study.
Out of 67 cases with NVC, 43 were female patients (64%) and 24 were male patients (35%) (Fig. 2). Among 67 patients, 40 (60%) had NVC on the left side and 27 (40%) on the right side.
NVC was observed at the root entry zone (< 7 mm from brain stem) in 63 trigeminal nerves on symptomatic side and 5 trigeminal nerves on the asymptomatic side. NVC outside the REZ (> 7 mm from brain stem) in ipsilateral trigeminal nerve was observed in 4 patients. NVC outside the REZ (> 7 mm from brain stem) in contralateral trigeminal nerve was observed in 21 patients (Fig. 3). NVCs at asymptomatic side were considered as controls in our study. With this, NVC occurring at REZ on symptomatic side was found to be statistically significant with P < 0.001. Mean distance of NVC at symptomatic side was 3.4 mm and 8.4 mm in asymptomatic NVCs.
Focal atrophy of trigeminal nerve at the site of NVC was seen in 8 trigeminal nerves, all on symptomatic side and with NVC occurring at root entry zone (Fig. 4).
No displacement of nerve root at the point of neurovascular contact was observed in our study.
Out of 93 trigeminal nerves with NVC, 72 nerves (77%) had vascular compression by the ipsilateral superior cerebellar artery and 21 nerves (23%) by the ipsilateral anterior inferior cerebellar artery (Fig. 5). No NVC due to venous loop was found in our study.
Mean length of cisternal segment was found to be 10.3 cm.
After the MRI brain imaging, the patients were issued MRI reports and referred back to department of neurology for further clinical management. We followed them regarding their management for trigeminal neuralgia symptoms. All the 67 patients were found to be on medical management. None of the patients underwent microvascular decompression surgery. This is a major limitation in our study. Due the absence of microvascular decompression surgery for these classical TGN patients with imaging diagnosis of NVC of trigeminal nerve, we were unable to intraoperatively confirm the neurovascular conflict, which in case would have been more reliable and strengthened our study results.
Discussion
Neurovascular contact is defined as a vascular loop coming in contact with cranial nerve roots that sometimes results in neurological symptoms and focal neurological deficit.
Incidence of trigeminal neuralgia was more commonly seen in 41–60 years age group followed by 61–80 years in our study with mean age of 55.6 years. This is comparable to study done by Maarbjerg et al [8]. They observed the mean age of occurrence of symptoms onset to be 53 years and mean age at the time of diagnosis to be 60.1 years. None of the patients were of less than 30 years in our study. This likely association between the older age group and TGN symptoms suggests that as the age increases the symptoms due to neurovascular conflict are more likely to manifest. However, our study sample size is small, further studies with larger sample size are necessary to establish this association between the older age and TGN symptoms.
NVC was more commonly seen in females (63%) than in males (37%) in our study. This correlates with Maarbjerg et al [8] with 61% of female patients. In another study done by Katusic et al [9] on trigeminal neuralgia had more incidence in female patients compared to our study with 73% females and 27% males in their study.
In our study, NVC occurring at the root entry zone (< 7 mm from brainstem) (Fig. 6) was associated with ipsilateral trigeminal neuralgia. This is in correlation with the study done by Maarbjerg et al [10]. They found out that severe neurovascular contact (NVC at REZ) was highly prevalent on the symptomatic compared to the asymptomatic side, i.e., 53% versus 13% with P < 0.001.
Out of 93 trigeminal nerves with NVC, 63 ipsilateral and 5 contralateral had NVC at root entry zone. NVC distal to REZ (Fig. 7) was observed in a total 25 trigeminal nerves, out of which 4 were on ipsilateral side and 21 on contralateral trigeminal nerves. These 21 cases of NVC outside the REZ on contralateral side had NVC within the root entry zone on ipsilateral side. NVCs occurring at REZ were more on symptomatic side. This observation is correlating with the study done by Miller et al. [10] where they observed the NVC to be occurring at more proximal nerve segment in symptomatic nerves compared to asymptomatic nerves.
The presence of NVC as such can be regarded as an anatomical variant. This becomes significant in certain conditions like the site of occurrence of NVC, i.e., distance from the brainstem and patient’s age. Our study shows NVC occurring in the root entry zone is the most important criterion correlating with ipsilateral TGN.
Superior cerebellar artery (SCA) or its branches have been described as the most common vessel causing NVC of the trigeminal nerve in the cisternal segment in literature [11] followed by AICA and its branches. In some cases, both SCA and AICA can be found in contact with the affected trigeminal nerve. In a study done by Yoshino et al. [12], SCA was found to cause NVC in 46%, AICA in 9%, basilar artery in 4%, posterior cerebellar artery in 2%, and vein in 6%. In our study, SCA was seen in 77% of cases causing NVC and AICA was found to be the cause of NVC in 23%. No venous loop was observed in our study.
In a study done by Maurya et al. [13], nerve atrophy was found in 52.9% of cases, arterial imprint/grooving on the trigeminal nerve in 50.9% of cases, and distortion of the course of the trigeminal nerve in 23.5% of cases. In our study, nerve atrophy (Fig. 8) was uncommonly observed in 8 cases (12%) only. The NVC was observed at root entry zone in all the cases with nerve root atrophy in our study. No nerve atrophy seen in the trigeminal nerves with NVC occurring distal to REZ.
We did not observe any nerve root deviation/obvious displacement from the normal course of the cisternal segment of the trigeminal nerve.
MRI brain imaging with FIESTA sequence is very reliable in diagnosing NVC. MRI TOF angiogram sequence is helpful in identifying the origin and nature of vascular loop involved in the NVC. The imaging diagnosis of NVC at root entry zone, when observed in patients with trigeminal neuralgia symptoms is definitely significant. However, the gold standard method to prove that NVC is underlying cause of TGN is by intraoperative confirmation and marked clinical improvement of symptoms post microvascular decompression surgery. This is the major limitation in our study. However, from previous studies done by Mistry et al. [14] who had done intra operative confirmation, we can assure that NVC at REZ is most likely cause for trigeminal neuralgia in patients with ipsilateral symptoms.
Conclusions
Neurovascular conflict of trigeminal nerve occurring at the nerve root entry zone has a strong association with ipsilateral trigeminal neuralgia symptoms. In addition, the presence of the trigeminal nerve thinning is also associated with ipsilateral trigeminal neuralgia. Neurovascular conflict occurring distal to the root entry zone is less likely associated with trigeminal neuralgia. With the increase in age, there are higher chances of association of NVC with ipsilateral trigeminal neuralgia symptoms.
Availability of data and materials
Will not be shared due to patient’s confidentiality and privacy concerns.
Abbreviations
- AICA:
-
Anterior inferior cerebellar artery
- FIESTA:
-
Fast Imaging Employing Steady-state Acquisition
- ICHD-3:
-
International Classification of Head ache Disorders 3rd edition
- NVC:
-
Neurovascular contact
- REZ:
-
Root entry zone
- SCA:
-
Superior cerebellar artery
- TGN:
-
Trigeminal neuralgia
- mm:
-
Millimeter
References
Manzoni GC, Torelli P (2005) Epidemiology of typical and atypical craniofacial neuralgias. Neurol Sci 26(2):s65–s67
Devor M, Amir R, Rappaport ZH (2002) Pathophysiology of trigeminal neuralgia: the ignition hypothesis. Clin J Pain 18:4–13
Love S, Coakham HB (2001) Trigeminal neuralgia: pathology and pathogenesis. Brain 124(Pt 12):2347–2360
Lang E, Naraghi R, Tanrikulu L, Hastreiter P et al (2005) Neurovascular relationship at the trigeminal root entry zone in persistent idiopathic facial pain: findings from MRI 3D visualization. J Neurol Neurosurg Psychiatry 76:1506–1509
McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90:1–8
Peker S, Kurtkaya O, Uzun I, Pamir MN (2006) Microanatomy of the central myelin-peripheral myelin transition zone of the trigeminal nerve. Neurosurgery 59:354–359
Headache Classification committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808.
Maarbjerg S, Wolfram F, Gozalov A, Olesen J, Bendtsen L (2015) Significance of neurovascular contact in classical trigeminal neuralgia. Brain 138:311–319
Katusic S, Beard CM, Bergstralh E, Kurland LT (1990) Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945–1984. Ann Neurol 27(1):89–95
Miller JP, Acar F, Hamilton BE, Burchiel KJ (2009) Radiographic evaluation of trigeminal neurovascular compression in patients with and without trigeminal neuralgia. J Neurosurg 110(4):627–632
Elainia S, Magnanb J, Devezeb A, Girardc N (2013) Magnetic resonance imaging criteria in vascular compression syndrome. Egypt J Otolaryngol 29:10–15
Yoshino N, Akimoto H, Yamada I et al (2003) Trigeminal neuralgia: evaluation of neuralgic manifestation and site of neurovascular compression with 3D CISS MR imaging and MR angiography. Radiology 228:539–545
Maurya V, Sreedhar CM, Khera A, Bhatia M, Sharma V (2019) Trigeminal neuralgia: When does neurovascular contact turn into a conflict? Med J Armed Forces India 75(2):134–139
Mistry AM, Niesner KJ, Lake WB, Forbes JA, Shannon CN, Kasl RA, Konrad PE, Neimat JS (2016) Neurovascular compression at the root entry zone correlates with trigeminal neuralgia and early microvascular decompression outcome. World Neurosurg 95:208–213
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HAA: study design, data collection, statistical analysis, data interpretation, manuscript preparation, literature search. MRK: study design, data collection, statistical analysis, data interpretation, manuscript preparation, literature search. SS: study design, data collection, statistical analysis, data interpretation, manuscript preparation, literature search. RRK: manuscript preparation. VV: manuscript preparation. GS: literature search. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approved by Institutional human ethics committee, PES Institute of medical sciences and research. Approval No: PESIMSR/IHE/139-21.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anwar, H., Ramya Krishna, M., Sadiq, S. et al. A study to evaluate neurovascular conflict of trigeminal nerve in trigeminal neuralgia patients with the help of 1.5 T MR imaging. Egypt J Radiol Nucl Med 53, 66 (2022). https://doi.org/10.1186/s43055-022-00746-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00746-8