Abstract
Background
Aphasia complicating stroke occurs due to language deficits that decrease communication abilities and functional independence. Our study aims to assess fractional anisotropy (FA) and mean diffusivity (MD) parameters of diffusion tensor imaging (DTI) of the dorsal stream language areas in patients with post-stroke aphasia. It was conducted on 27 patients with post-stroke aphasia and 27 age- and sex-matched controls who underwent DTI of the brain. FA and MD values of Broca's area (BA), Wernick's area (WA), superior longitudinal fasciculus (SLF), and arcuate fasciculus (AF), and number of tract fibers (TF) of AF and SLF were calculated. Results were correlated with National Institutes of Health Stroke Scale (NIHSS), Arabic version of Comprehensive Aphasia Test (Arabic CAT), and Mansoura Arabic Screening Aphasia Test (MASAT).
Results
FA of AF and SLF in patients was significantly lower (P = 0.001) than controls. MD of AF and SLF in patients was significantly higher (P = 0.001) than controls. The mean volume TF of AF and SLF in patients was significantly (P = 0.001) lower than the mean volume in controls for AF and SLF. FA cutoff for AF was 0.34 and for SLF, it was 0.35 with sensitivity, specificity, and accuracy (85.2%, 62.1%, 73.2%) for AF, (74.1%, 69%, 71.4%) for SLF, respectively. MD cutoff value for AF was 0.87, and 0.84 for SLF with sensitivity, specificity, and accuracy (63%, 72.4%, 67.8%) for AF, (81.5%, 79.3%, 80.4%) for SLF, respectively. Cutoff TF of AF was 1728 and for SLF it was 601 with sensitivity, specificity, and accuracy (88.9%, 72.4%, 80.4%) for AF and (85.2%, 85.2%, 78.6%) for SLF, respectively.
Conclusions
DTI is a non-invasive promising method that can be used to assess language areas in patients with post-stroke aphasia.
Similar content being viewed by others
Background
Aphasia is a very common complication in stroke patients; it is reported in up to 30% of acute stroke survivors and long-lasting in the chronic post-stroke stage in 16–31% of these patients; however, spontaneous recovery may occur during the first three months after onset. Aphasia occurs due to language deficits that impair communication abilities and decrease functional independence. Patients with aphasia have many difficulties in spontaneous speech, comprehension, repetition, reading, writing, and calculation, which have adverse effects on their daily life. Therefore, a quantitative and precise assessment of microstructural damage in language areas would enhance understanding of disease pathology and prognosis of aphasia [1,2,3]. Several cerebral areas such as BA and WA are responsible for language processing; WA (posterosuperior temporal) is considered receptive language area and BA (inferolateral frontal) is considered expressive language area or motor center of speech. Neural tracts for language are classified into two categories: the dorsal stream for phonation and the ventral stream for comprehension. The dorsal stream originates in the peri-Sylvian area within the superior temporal gyrus. Its major fiber tracts include SLF and AF, connecting WA with BA. AF in the dominant hemisphere (usually the left) supports comprehension, speech production, repetition, and reading. AF also plays an essential role in the presence, recovery, and prognosis prediction of aphasia [2,3,4,5,6].
National Institutes of Health Stroke Scale (NIHSS) quantifies the impairment caused by a stroke. The NIHSS is composed of 11 items, each of which scores a specific ability between 0 and 4. For each item, a score of 0 typically indicates a normal function in that specific ability, while a higher score is indicative of some level of impairment [7]. Mansoura Arabic Screening Aphasia Test (MASAT) is a valid and a reliable screening tool that can be completed within a brief single therapy session, bedside evaluation, or the first clinic appointment that detects the type and severity of Arabic-speaking aphasic patients [8]. Arabic version of the Comprehensive Aphasia Test (Arabic CAT) the modified CAT provides an overview of the linguistic abilities and impairments of an aphasic person through a quick comprehensive and standardized profile of language performance [9].
Diffusion tensor imaging (DTI) is an emerging MR imaging technique that reflects micromovement of water molecules and can distinguish between different tissue compartments at the cellular level with different metrics. The most common metrics of diffusion tensor imaging used are fractional anisotropy (FA) and mean diffusivity (MD) [10,11,12,13,14,15]. DTI facilitates the reconstruction and investigation of the language areas and allows anatomical assessment of damage-dysfunction relationships [16,17,18]. FA reflects brain integrity using the movement of water molecules and is used to investigate changes in brain structures associated with language function according to duration after stroke [1,2,3,4, 19]. DTI provides useful information on the evaluation of AF injury and its severity in stroke patients with aphasia [4, 5, 20, 21]. In this study measurement of the FA and MD changes in WA and BA was correlated with the clinical scoring for stroke (NIHSS) and aphasia scores including Arabic CAT Screening test and Mansoura Arabic Screening Aphasia Test.
This work aimed to test the significance of FA and MD of DTI in assessing the dorsal stream language areas in patients with aphasia after stroke in correlation with clinical scoring systems.
Methods
Patients
Institutional review board approval was obtained, and informed consent was taken from each patient. This study was a prospective study that was performed on 29 consecutive patients, and inclusion criteria included patients presented with aphasia, according to clinical scoring systems [8, 9], after having an ischemic stroke. Exclusion criteria included the presence of cognitive and neurological deficits or psychiatric illness or other major medical disorder in healthy participants. Two patients with motion artifacts were also excluded. The final patients included in this study were 27 patients (15 males and 12 females, age range from 33 to 82 years, mean age 57.9 ± 8.3 years). All patients presented clinically with aphasia and right-sided hemiparesis and underwent non-contrast MRI of the brain with DTI on the diseased side (in all patients it was the Lt side), disease duration ranged between 2 and 6 weeks, and 27 controls of matched age and sex who had no neurological deficits underwent brain MRI with DTI with assessment of the same parameters.
Clinical tests
Patients were subjected to specific clinical tests which were done, while the patient in the acute stage (within 2–6 weeks), NIHSS was done followed by MASAT and Arabic CAT for true assessment of established language defect. For stroke assessment using NIHSS, the individual scores from each item are summed in order to calculate a patient's total NIHSS score. Score 0 indicates no stroke symptoms, score 1–4 indicates minor symptoms, score 5–15 indicates moderate stroke, score 16–20 indicates moderate to severe [7]. MASAT is categorized into (A) Educated patients: Total normal test examination = 60, mild dysphasia = 46–59, moderate dysphasia = 31–45, and severe dysphasia ≤ 30. (B) Illiterate patients: Total normal test examination: = 48, mild dysphasia = 25–47, moderate dysphasia = 13–24, severe dysphasia = 0–12 [8]. Arabic CAT Screening test: Almost all the test items are scored on a 0–2 scale [9]. Arabic CAT is the profile of T-scores across the different subtests that can be used to identify strengths and weaknesses relative to the aphasic population. The overall severity of aphasic impairment is estimated by taking the mean T-score across the eight language modalities of the CAT (totals of spoken language, written language, repetition, naming, spoken picture description, reading, writing, and written picture description). If scores are unavailable, the mean score on at least 4–6 of the eight modalities may yield a reliable estimate of the overall severity. The T-score is represented on T-score profile on which the cutoff scores are represented. Scores below the cutoff points indicate aphasic performance [8, 9].
MR imaging
All patients were examined on a 1.5-T scanner (Ingenia, Philips, Philips Medical Systems, Best, Nederland). A self-shielding gradient set with a 16-channel neurovascular coil was used. Sequences used: T1-weighted images TR/TE = 800/15 ms), T2-weighted fast spin-echo images (TR/TE = 6000/80 ms), and fluid-attenuated inversion recovery FLAIR images. The scanning parameters were section thickness = 5 mm, an inter-slice gap = 1.5 mm, a field of view (FOV) = 25–30 cm2 and an acquisition matrix = 256 × 224. DTI acquired using a single-shot echo-planar imaging sequence (TR/TE = 3200/ 90 ms) with parallel imaging. Automatic multi-angle-projection shim and chemical shift selective fat suppression (CHESS) technique applied to reduce the artifacts at diffusion-weighted MR images. Diffusion gradients were applied along 32 axes, using a b-value of 0 and 1000 s/mm2. The scanning parameters were: FOV = 250 × 170 mm2, data matrix = 92 × 88 and voxel dimensions = 2.43 × 2.54 × 2.5 mm3. Forty-eight slices were obtained, with a thickness of 2.5 mm, with no gap and the total scan duration was 7–8 min.
Image analysis
Using secondary work station (Phillips Advantage windows workstation with functional tool software) image analysis was performed by ten and fifteen years experienced neuro-radiologists who were blinded to the clinical tests. Conventional MRI images were evaluated by one radiologist (AA), for the detection of infarction region. Fiber tracking and reconstruction of the AF and SLF was done by the other radiologist (AE). For reconstructing the AF, two ROIs approach by Catani et al. [22, 23] was used; a ROI was manually placed on the posterior parietal area of the superior longitudinal fascicle, and another target ROI was placed in the posterior temporal lobe. In control group fiber tracking was initiated with a fractional anisotropy (FA) > 0.18 and apparent diffusion coefficient (ADC) > 0.01 at the center of a seed voxel. For SLF ROI on the axial plane placed on the angular gyrus and the precentral gyrus and caudal middle frontal gyrus based on brain atlas. Fibers running to the temporal lobe were excluded as they belong to the arcuate fasciculus.
Tracts were captured over 3D brain volumes T2-BRAVO images.
A ROI was placed on the obtained tracts on the diseased side with infarction; the FA and MD were automatically calculated as well as the number of TF. A ROI was placed on BA (inferolateral frontal) and WA (posterosuperior temporal) on the side with infarction with measurement of the FA and MD values. Tracts were visually evaluated for changes in size and changes in the number of tract fibers, and the involved white matter tracts were compared with the corresponding tracts of the normal hemisphere in the control group.
Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS Corp. Released in 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Quantitative data (FA, MD, volume, NHISS) were described using median (minimum and maximum), mean, and standard deviation. The significance of the obtained results was judged at the (0.05) level. After testing normality using the Kolmogorov–Smirnov test, Student's t test was used to compare between patients and control groups. The Spearman's rank-order correlation is used to determine the strength and direction of a linear relationship between two non-normally distributed continuous variables (between FA, MD, number of TF, and clinical assessment scores). The diagnostic performance of a test or the accuracy of a test to discriminate diseased cases from non-diseased cases is evaluated using receiver operating characteristic (ROC) curve analysis. Sensitivity and specificity were detected from the curve, and PPV, NPV, and accuracy were calculated through cross-tabulation.
Results
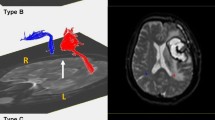
All patients had left-sided ischemic stroke lesions, one patient with conduction aphasia showed partial injury of the left AF, patients with Broca's aphasia showed disruptions of the left AF over the stroke lesions, and one patient with global aphasia had a severe injury and Wallerian degeneration of the left AF with difficult reconstruction and marked thinning of tract fibers Fig. 1.
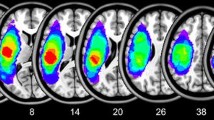
Table 1 shows the mean, standard deviation of FA and MD (×10−3mm2/s), and number of TF between patients and control. Table 2 shows the ROC curve results with the calculation of AUC, cutoff, accuracy, sensitivity, and specificity of FA and MD (10−3 mm2/s) of the language areas used to differentiate patients and control. Figure 2 shows DTI of mild aphasia, and Fig. 3 shows DTI of severe aphasia.
DTI of patient with mild aphasia: 46-year-old male, a axial T2-WI, b axial FLAIR image showing Lt. temporal infarction, c coronal DTI image with reconstructed AF, d axial DTI image with reconstructed SLF showing mild reduction of the Lt. AF and Lt. SLF size with decreased number of fibers. On the Rt. side values showed more preserved function and integrity
DTI of patient with sever aphasia 68-year-old male, a axial T2-WI, b axial FLAIR image showing Lt.-sided infarction, with senile brain atrophic changes, c axial T2 DTI with reconstructed SLF, d coronal T2 DTI image with reconstructed AF showing marked reduction of both AF and SLF size more evident on the Lt. side, with decreased number of fibers, the patient had history of Rt.-sided infarction 2 years ago
DTI findings
The mean FA of affected SLF (0.31 ± 0.05) was significantly lower than controls (0.37 ± 0.02). The mean FA of the affected AF was 0.30 ± 0.04 which was significantly lower than controls (0.35 ± 0.02). There was no statistically significant difference between the FA of the affected BA and WA. The FA cutoff value for AF was 0.34, and for SLF it was 0.35 below which was considered a diseased area, and values above were considered normal areas, with sensitivity, specificity, and accuracy (85.2%, 62.1%, 73.2%) for AF, (74.1%, 69%, 71.4%) for SLF, respectively (Fig. 4a).
The mean MD value of the affected SLF was 0.91 ± 0.1 × 10−3 mm2/s which was significantly higher than the mean MD of control (0.81 ± 0.04 × 10−3 mm2/s) (P = 0.001). The mean MD value of the affected AF was 0.89 ± 0.09 × 10−3 mm2/s which was significantly higher than controls (0.84 ± 0.05 × 10−3 mm2/s). There was no statistically significant difference between the mean MD value of the affected BA which was 0.87 ± 0.1 × 10−3 mm2/s and controls (0.82 ± 0.1 × 10−3 mm2/s). Also, the mean MD value of the affected WA was 0.82 ± 0.1 × 10−3 mm2/s which was not higher than controls (0.83 ± 0.1 × 10−3 mm2/s). The MD cutoff value for AF was 0.87 and for SLF it was 0.84, values above were considered diseased area, and values below were considered normal areas, with sensitivity, specificity, and accuracy (63%, 72.4%, 67.8%) for AF and (81.5%, 79.3%, 80.4%) for SLF, respectively (Fig. 4b).
The volume of TF of SLF in patients was 285.6 ± 264 which was significantly (P value = 0.001) lower than that of TF in controls (1039.6 ± 698). The volume of TF of AF in patients was 731 ± 743 which was significantly lower than that of controls (2649.5 ± 1728), (P value = 0.001). The cutoff values of volume of AF and SLF between patients and controls was 1728 and 601 with sensitivity, specificity and accuracy (88.9%, 72.4%, 80.4%) for AF and (85.2%, 85.2%, 78.6%) for SLF, respectively (Fig. 4c).
Clinical tests and correlations
According to NIHSS, one patient had minor stroke symptoms, twenty-five had moderate stroke symptoms, and one had severe stroke symptoms. Patients were clinically classified according to the type of aphasia; five patients had Wernick's aphasia, two patients with transcortical motor aphasia, four patients with global aphasia, two with conduction aphasia, thirteen patients with Broca's aphasia, and one patient with anomic aphasia. According to the Arabic CAT, all patients were aphasic. According to MASAT, patients were classified into mild (n = 2), moderate (n = 12), and severe (n = 13). The mean of NIHSS was 9.1; there was a significant difference between mild and advanced cases. The NIHSS was negatively correlated with FA of the SLF (r = − 0.55, p = 0.011). The mean value of Mansoura score was 20.3; it was positively correlated with FA of SLF (r = 0.532, p = 0.02) and with number of TF of AF (r = 0.62, p = 0.005). The mean value of Arabic CAT was 44.5 it was positively correlated with the number of TF of AF (r = 0.54, p = 0.02), and disease duration (r = 0.727, p = 0.001). Also, a number of TF of the SLF was positively correlated with MASAT (r = 0.554, p = 0.017) and with Arabic CAT (r = 0.470, p = 0.049).
Discussion
DTI metrics have been used to monitor structural changes in aphasia after stroke due to marked sensitivity in detecting structural tissue abnormalities. DTI parameters can also be used as prognostic markers of disease evolution [1, 2, 17,18,19]. In this study, mean FA and MD of the AF and SLF and number of TF were found to be accurate parameters for detecting differences and changes between patients (with affected language areas and tracts) and controls.
FA is a common measurement used in DTI studies that indicates diffusion orientation and is high along well-defined pathways such as the corpus callosum, pyramidal tracts, and optic radiations. FA value is a potential marker of axonal structural integrity; higher FA values indicate increased parallel movement of water molecules to fiber tracts, denoting increased structural connectivity [1,2,3, 18, 19]. Decreased FA value is related to the disintegration of the neural tract. In our study, we found that the mean FA of AF and SLF in patients with aphasia was significantly lower than controls with a positive correlation between FA of SLF and MASAT. There was also a negative correlation between the FA of the SLF and NIHSS, indicating that decrease in FA value was associated with a higher NIHSS score. This was in agreement with previous DTI studies [4, 5, 20, 21] that showed negative correlations between comprehension abilities and FA decline.
MD value indicates the magnitude of water diffusion, which can increase with vasogenic edema or accumulation of cellular debris due to axonal damage. The mean MD value of AF and SLF in patients with aphasia in our results was significantly higher than the mean MD value in controls. This study's findings demonstrated that injuries of the AF and SLF could cause conduction aphasia in stroke patients. This was coping with other studies [5] which showed that lower FA and higher MD values of the AF and SLF of the affected hemisphere were found to show a correlation with a decreased ability of repetition and comprehension deficits after stroke, and also showed an association with lower FA value of the affected AF [1, 2, 17, 18].
In our study changes of the AF and SLF in patients were in the form of decreased FA value, increased MD value, and decreased number of TF on DTI which can be used as follow-up DTI parameter in stroke patients. This was in agreement with other studies which revealed that AF has a critical role in determining aphasia severity with decreased FA value and a smaller number of TF of the affected AF, compared with the control AF [5, 20, 21].
In our study during processing of cases, we have noticed that atrophic brain changes led to marking thinning of the affected tract fibers with evident degeneration and atrophy, and patients with mild NIHSS showed more preserved shape and number of TF of the AF and SLF, while aged patients with brain atrophic changes showed a decreased number of TF of the AF and SLF as a part of the aging process. A previous study reported that higher FA values and a higher number of tract fibers in corpus callosum suggest intact fibers, and also reported that density and volume of corpus callosum can be affected by brain size [24] which was in agreement with our results (Fig. 5).
DTI of patient with sever aphasia: 61-year-old patient with a axial T2 reconstructed Lt SLF with marked thinning and atrophy of its fibers, b coronal T2 reconstructed AF shows the Lt AF also with sever atrophy, c axial T2WI for both SLF with marked thinning. d Coronal reconstructed AF and e axial reconstructed SLF in another patient with similar findings
In our study, the FA values of the affected posterior segments of the AF, and the anterior segments of the AF in patients with Wernick's-like conduction aphasia and in patients with Broca's-like conduction aphasia, respectively, were smaller than those of controls. However, there was no significant difference detected in the mean FA value in BA and WA between patients and control which may be attributed to the presence of Lt-sided infarction in all patients interfered with accurate ROI placement at the anatomical site of the BA and WA.
The integration of both DTI and conventional MRI measures together with connectivity-based regional assessment and the development of novel image analysis and visualization techniques could provide better means to understand the nature and the location of WM abnormalities. The relationship between WM disruption, WM connectivity, and clinical measures will potentially allow clinicians to correlate fiber tract disruption and cognitive impairment better. Furthermore, it would ultimately lead to improved monitoring of patients, better prediction of the course of the disease, and more rapid assessment of new treatments or therapies [1,2,3,4, 19].
In this study, there is a correlation between NIHSS and DTI parameters. NIHSS quantifies the impairment caused by a stroke [7]. MASAT is a valid and reliable brief assessment tool that can be completed on the first clinic appointment that detects the type and severity of Arabic-speaking aphasic patients; the tool is designed to be used by either phoniatricians who are physicians in Egypt or speech-language pathologists [8]. Provided clinical data by these tests could be correlated with imaging findings and parameters detected by DTI; minor or moderate stroke symptoms with subsequent mild to moderate aphasia are expected to have less damage to and more preserved functions of the affected language areas as well as maintained number of TF, in contrary to cases with moderate to severe and cases with severe stroke symptoms and aphasia.
There are a few limitations of this study. First, this study includes a small number of patients. Further studies done upon a large number of patients are recommended and also patients recruited at different stages of post-stroke recovery and were grouped together over a time period ranging from two to six weeks after stroke, which might have affected the results. Second, this study used DTI at a 1.5-Tesla machine. Further studies that used multi-parametric MR imaging include arterial spin labeling, perfusion MR imaging, and MR spectroscopy will improve the results [25,26,27,28,29,30,31,32,33,34]. Third, there is no follow-up of these patients. Further studies with longitudinal assessment of these patients after therapy are recommended.
Conclusions
We concluded that FA and MD of AF and SLF, as well as the number of TF, can detect changes in language areas in patients with aphasia after stroke, which could be correlated with the patient's clinical data.
Availability of data and materials
Not applicable.
Abbreviations
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- MD:
-
Mean diffusivity
- SLF:
-
Superior longitudinal fasciculus
- AF:
-
Arcuate fasciculus
References
Kyeong S, Kang H, Kyeong S, Kim DH (2019) Differences in brain areas affecting language function after stroke. Stroke 50:2956–2959
Yu Q, Wang H, Li S, Dai Y (2019) Predictive role of subcomponents of the left arcuate fasciculus in prognosis of aphasia after stroke: A retrospective observational study. Medicine 98:e15775
Hillis AE, Beh YY, Sebastian R, Breining B, Tippett DC, Wright A et al (2018) Predicting recovery in acute poststroke aphasia. Ann Neurol 83:612–622
Meier EL, Johnson JP, Pan Y, Kiran S (2019) The utility of lesion classification in predicting language and treatment outcomes in chronic stroke-induced aphasia. Brain Imaging Behav 13:1510–1525
Jang SH, Cho IT, Lim JW (2017) Recovery of aphasia and change of injured arcuate fasciculus in the dominant hemisphere in stroke patients. NeuroRehabilitation 41:759–764
Watila MM, Balarabe SA (2015) Factors predicting post-stroke aphasia recovery. J Neurol Sci 352:12–18
Kwah LK, Diong J (2019) National institutes of health stroke scale (NIHSS). J Physiother 60:61
Abou-Elsaad T, Baz H, Belal T, Elsherbeny S (2018) Developing an arabic screening test for adult-onset chronic aphasia. Folia Phoniatr Logop 70:74–81
Abou El-Ella MY, Alloush TK, Elshobary AM, El-Dien Hafez NG, Abd EL-Halim AI, El-Rouby IM (2013) Modification and standardisation of Arabic version of the Comprehensive Aphasia Test. Aphasiology 27:599–614
Abdel Razek AAK, El-Serougy L, Ezzat A, Eldawoody H, El-Morsy A (2020) Interobserver agreement of white matter tract involvement in gliomas with diffusion tensor tractography. J Neurol Surg A Cent Eur Neurosurg 81:233–237
Abdel Razek AAK, Talaat M, El-Serougy L, Abdelsalam M, Gaballa G (2019) Differentiating glioblastomas from solitary brain metastases using arterial spin labeling perfusion- and diffusion tensor imaging-derived metrics. World Neurosurg 127:e593–e598
Abdel Razek AAK, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M (2019) Differentiation of primary central nervous system lymphoma from glioblastoma: quantitative analysis using arterial spin labeling and diffusion tensor imaging. World Neurosurg 123:e303–e309
Razek AAKA, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M (2018) Differentiation of residual/ recurrent gliomas from postradiation necrosis with arterial spin labeling and diffusion tensor magnetic resonance imaging-derived metrics. Neuroradiology 60:169–177
El-Serougy L, Abdel Razek AA, Ezzat A, Eldawoody H, El-Morsy A (2019) Assessment of diffusion tensor imaging metrics in differentiating low-grade from high-grade gliomas. Neuroradiol J 29:400–407
Razek AAKA, Batouty N, Fathy W, Bassiouny R (2018) Diffusion tensor imaging of the optic disc in idiopathic intracranial hypertension. Neuroradiology 60:1159–1166
Hill VB, Cankurtaran CZ, Liu BP, Hijaz TA, Naidich M, Nemeth AJ et al (2019) A practical review of functional MRI anatomy of the language and motor systems. version 2. AJNR Am J Neuroradiol 40:1084–1090
Ivanova MV, Isaev DY, Dragoy OV, Akinina YS, Petrushevskiy AG, Fedina ON et al (2016) Diffusion-tensor imaging of major white matter tracts and their role in language processing in aphasia. Cortex 85:165–181
Smits M, Jiskoot LC, Papma JM (2014) White matter tracts of speech and language. Semin Ultrasound CT MR 35:504–516
Ryu H, Park CH (2020) Structural characteristic of the arcuate fasciculus in patients with fluent aphasia following intracranial hemorrhage: a diffusion tensor tractography study. Brain Sci 10:E280
Lim JS, Kang DW (2015) Stroke connectome and its implications for cognitive and behavioral sequela of stroke. J Stroke 17:256–267
Jang SH (2013) Diffusion tensor imaging studies on arcuate fasciculus in stroke patients: a review. Front Hum Neurosci 7:749
Catani M, Jones DK, ffytche DH, (2005) Perisylvian language networks of the human brain. Anna Neurol 57:8–16
Qiwei Yu MM, Hong Wang MM, Shuqing Li MM, Yanhong Dai MM (2019) Predictive role of subcomponents of the left arcuate fasciculus in prognosis of aphasia after stroke A retrospective observational study. Medicine 98:23
Timocin G, Toprak A, Aralasmak A (2020) Relationships of language lateralization with diffusion tensor imaging metrics of corpus callosum, tumor grade, and Tumors distance to language-eloquent areas in glial neoplasms. J Comput Assist Tomogr 44:956–968
Abdel Razek AAK, Talaat M, El-Serougy L, Gaballa G, Abdelsalam M (2019) Clinical applications of arterial spin labeling in brain tumors. J Comput Assist Tomogr 43:525–532
El-mewafy Z, Abdel Razek AAAK, El-Eshmawy M, Abo El-Eneen N, El-Biaomy A (2018) MR spectroscopy of the frontal region in patients with metabolic syndrome: Correlation. Polish J Radiol 83:e215-9
Razek AAKA, Batouty NM, Azab AG (2020) Role of susceptibility-weighted imaging in patients with idiopathic intracranial hypertension. Jpn J Radiol 38:740–745
Abdel Razek AA, Elkhamary S, Al-Mesfer S, Alkatan HM (2012) Correlation of apparent diffusion coefficient at 3T with prognostic parameters of retinoblastoma. AJNR Am J Neuroradiol 33:944–948
Abdel Razek AA, Kamal E (2013) Nasopharyngeal carcinoma: correlation of apparent diffusion coefficient value with prognostic parameters. Radiol Med 118:534–539
Razek AAKA (2018) Diffusion tensor imaging in differentiation of residual head and neck squamous cell carcinoma from post-radiation changes. Magn Reson Imaging 54:84–89
Abdel Razek AA (2018) Characterization of salivary gland tumours with diffusion tensor imaging. Dentomaxillofac Radiol 47:20170343
Razek AA, Shabana AA, El Saied TO, Alrefey N (2017) Diffusion tensor imaging of mild-moderate carpal tunnel syndrome: correlation with nerve conduction study and clinical tests. Clin Rheumatol 36:2319–2324
Abdel Razek AAK (2020) Editorial for “preliminary assessment of intravoxel incoherent motion diffusion-weighted MRI (IVIM-DWI) metrics in Alzheimer’s disease.” J Magn Reson Imaging 52:1827–1828
Razek AAKA (2020) Editorial for “Preoperative MRI-based radiomic machine-learning nomogram may accurately distinguish between benign and malignant soft tissue lesions: a two-center study.” J Magn Reson Imaging 52:883–884
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
AE gave the idea and revised the manuscript. AAR revised the manuscript. TA-E and NI collected the data. TB analyzed the data. EA analyzed the data and wrote the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration. The study was approved by Mansoura Faculty of Medicine Institutional Research Board (MFM-IRB), and reference number is not available. Verbal consents were provided by patient guardians (all patients were aphasic), so the ethics committee approved this procedure.
Consent for publications
Obtained.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmongui, A., AbdelRazek, A., Abou-Elsaad, T. et al. Diffusion tensor imaging of dorsal stream language areas in patients with post-stroke aphasia. Egypt J Radiol Nucl Med 53, 11 (2022). https://doi.org/10.1186/s43055-021-00690-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00690-z