Abstract
Background
Cholecysto-enteric fistula is a rare complication of cholelithiasis and cholecystitis. Another even rarer complication is proximal impaction of gallstone(s) in gastric pylorus leading to gastric outlet obstruction, known as the Bouveret Syndrome. Only a few cases have been reported in the available literature. It can be confused with a malignant thickening at the pylorus, knowledge of this syndrome helps in arriving at the right diagnosis.
Case report
A 52-year-old female patient, who was admitted to our hospital for evaluation of recurrent vomiting and abdominal pain. She was investigated with various imaging modalities including upper gastrointestinal (GI) endoscopy, abdominal ultrasonography as well as Contrast Enhanced Computerized Tomography (CECT) scan of the abdomen. On the outside scan, it was given as a malignant thickening at the pylorus. However, current radiologists felt that imaging findings were not of a typical malignant mass, and suspicion of Bouveret syndrome was given. Intraoperative findings confirmed the diagnosis of Bouveret syndrome. The patient has not experienced any postoperative complications till now.
Conclusion
Bouveret syndrome is associated with significant morbidity and mortality. Being familiar with the imaging appearance of this condition, and differentiating it with malignant thickening can help radiologists avoid unnecessary invasive procedures in such patients. Being a benign etiology, it also helps in a better prognosis.
Similar content being viewed by others
Background
Bouveret syndrome is caused by the impaction of migrated gallstone(s) in the pylorus or proximal duodenum which causes gastric outlet obstruction [1]. Only 316 cases have been reported in available literature till now [2]. It most commonly affects elderly female patients [3]. Since it is a rare and atypical complication of gallstone disease, the diagnosis of Bouveret syndrome is often delayed or overlooked. This is associated with considerable morbidity and mortality. The aim of reporting this case is to increase the awareness of this overlooked condition as timely diagnosis and management will lead to improved prognosis in these patients [4].
Case presentation
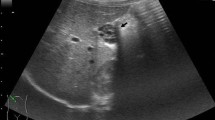
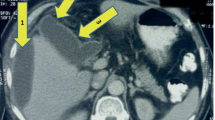
A 52-year-old female patient who was a known case of diabetes mellitus and hypertension presented to the gastro-surgery outpatient’s Department (OPD) with complaints of recurrent attacks of vomiting and abdominal pain. On physical examination there was no obvious lump in the abdomen, however, there was tenderness in the epigastrium. No similar illness was present in family members. Patients had a good socio-economic status. The patient had no significant past medical or surgical history. The patient was advised routine blood workup, upper GI endoscopy, and abdominal ultrasound. Endoscopy showed a mass lesion in the gastric pylorus obstructing which scope could not be negotiated. Biopsy was taken which showed an inflammatory picture without evidence of malignancy. Ultrasonography showed cholelithiasis. A contrast-enhanced CT scan of the abdomen was done to characterize the lesion causing obstruction. CT showed mild pneumobilia associated with a well-defined spherical non-enhancing hypodense lesion of size 2 cm in the submucosa of the gastric pylorus as shown in Fig. 1, consistent with an impacted gallstone causing Bouveret syndrome. The patient underwent surgery, intraoperative findings (Fig. 2) confirmed the diagnosis of Bouveret syndrome. Our patient underwent exploratory laparotomy, cholecystectomy, primary repair of fistula opening. Frozen section biopsy from pyloric mucosa and GB wall were sent for histopathological correlation. The patient has not experienced any postoperative complications till now. It was a life-changing surgery for the patient since he was previous diagnosed with a malignant mass. The patient was happy with the current diagnosis and surgery for being a benign etiology instant of malignant as diagnosed previously.
A–C Contrast-enhanced computed tomography images in coronal (A), axial (B) and sagittal (C) sections showing submucosal impaction of gallstone (hypodense) with surrounding mucosal thickening (red arrow) at pylorus causing gastric outlet obstruction. D Axial CT images in lung window to show pneumobilia (blue arrow)
Discussion
Bouveret's syndrome refers to gastric outlet obstruction caused by the formation of a chole-cysto-pyloric fistula and subsequent migration and impaction of a large gallstone into the pylorus [5]. Risk factors for Bouveret's syndrome include gallstones > 2.5 cm in size, the female sex, and age > 70 years. Gastric outlet obstruction causes multiple symptoms including abdominal pain, recurrent nausea/vomiting, and dyspepsia. Abdominal imaging in this syndrome typically reveals Rigler's triad of ectopic gallstone, pneumobilia, and small bowel obstruction. However, only ~ 33% of gallstone ileus cases exhibit these changes on conventional radiographs [6].
In this study a 52 years old female, who is relatively younger as compared to patients presenting with Bouveret syndrome. It provides a unique opportunity to examine the treatment options.
After extensive research of current literature, it was found out that a CECT scan of the abdomen is the most effective imaging technique to diagnose Bouveret syndrome. In this patient, the CECT scan successfully revealed both gallstones at the pylorus and its associated cholecysto-pyloric fistula causing gastric outlet obstruction.
Multiple treatment options are available for these patients from the least invasive treatment options like the endoscopy approach (with the low successful outcome) to surgical exploration (with the highly successful post-operative result). Existing literature suggests enterolithotomy as one of the treatment options for this syndrome as the advanced age makes them poor surgical candidates. A younger patient such as in our case can safely undergo surgery [4]. This case also emphasizes that younger patients can safely undergo surgical procedures, a course of action that can reduce the risk of gallstone recurrence. In absence of repair young patients would be at a greater risk of developing problems associated with a persisting fistula [7]. In our particular case, fistula repair was carried out, with positive results evidenced by the healthy condition of the patient after the operation [5]. The present case, alongside the existing literature regarding treatment in younger patients, shows that younger patients indeed can accept the greater surgical pressures associated with these approaches.
The present study offers the rare opportunity to study the successful treatment and outcome of a Bouveret syndrome patient whose age is far below that of the average patient afflicted by this condition.
Conclusions
Being a rare complication, Bouveret syndrome presents as a diagnostic dilemma and the US abdomen shows low specificity for diagnosis. A timely diagnosis is possible with an available imaging modality. Being a benign etiology it has a better prognosis. Abdominal radiograph, US, CT can be used for diagnosis, with CT being one of the most sensitive modalities for diagnosis. Being familiar with the imaging appearance of this condition, a radiologist can help in significantly reducing morbidity and mortality from this syndrome.
Availability of data and materials
Not applicable.
Abbreviations
- CECT:
-
Contrast-enhanced computed tomography
- GB:
-
Gall Bladder
- US:
-
Ultrasonography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- GI endoscopy:
-
Gastrointestinal endoscopy
- OPD:
-
Out Patient’s Department
References
Brennan GB, Rosenberg RD, Arora S (2004) Bouveret syndrome. Radiographics 24(4):1171–1175. https://doi.org/10.1148/rg.244035222
Wang F, Du ZQ, Chen YL, Chen TM, Wang Y, Zhou XR (2019) Bouveret syndrome: a case report. World J Clin Cases 7(23):4144–4149. https://doi.org/10.2998/wjcc.v7.i23.4144
Zafar A, Ingham G, Jameel JK (2013) “Bouveret’s syndrome” presenting with acute pancreatitis a very rare and challenging variant of gallstone ileus. Int J Surg Case Rep 4(5):528–530. https://doi.org/10.1016/j.ijscr.2013.01.017
Caldwell KM, Lee SJ, Leggett PL, Bajwa KS, Mehta SS, Shah SK (2018) Bouveret syndrome: current management strategies. Clin Exp Gastroenterol 11:69–75. https://doi.org/10.2147/CEG.S132069
Yu YB, Song Y, Xu JB, Qi FZ (2019) Bouveret’s syndrome: a rare presentation of gastric outlet obstruction. Exp Ther Med 17(3):1813–1816. https://doi.org/10.3892/etm.2019.7150
Trubek S, Bhama JK, Lamki N (2001) Radiological findings in bouveret’s syndrome. Emerg Radiol 8(6):335–337
Yang KJ, Chang CK (2020) Bouveret syndrome: a rare case of instance and treatment in a younger patient. Case Rep Gastrointest Med 2020:1837387. https://doi.org/10.1155/2020/1837387
Acknowledgements
No acknowledgements.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
LM made contribution in the form of design and draft of the work. BS has made contributions in the form of description of CECT images. RS contributed to data acquisition. UC has made contributions in diagnosis of the case, conception and design of the work, and also supervised the whole manuscript. AM has made contributions to operative details and provided intraoperative images. All authors approved the submitted version of the case report. All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee of our institute.
Consent for publication
The written and informed consent to publish the personal and clinical details of the participant was obtained from the patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
CARE Checklist of information to include when writing a case report.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meena, L., Sharma, B., Singh, R.S. et al. Cholecysto-pyloric fistula with submucosal impaction of gall stone causing gastric outlet obstruction masquerading as a gastric mass, Bouveret Syndrome: case report. Egypt J Radiol Nucl Med 52, 237 (2021). https://doi.org/10.1186/s43055-021-00619-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00619-6