Abstract
Background
Brain metastases (BM) are the most common intracranial tumors in adults outnumbering all other intracranial neoplasms. Positron emission tomography combined with computed tomography (PET/CT) is a widely used imaging modality in oncology with a unique combination of cross-sectional anatomic information provided by CT and the metabolic information provided by PET using the [18F]-2-fluoro-2-deoxy-d-glucose (FDG) as a tracer. The aim of the study is to assess the role and diagnostic performance of brain-included whole-body PET/CT in detection and evaluation of BM and when further imaging is considered necessary. The study was conducted over a period of 12 months on 420 patients suffering from extra-cranial malignancies utilizing brain-included whole-body PET/CT.
Results
Thirty patients with 71 brain lesions were detected, 18 patients (60%) had BM of unknown origin while 12 patients (40%) presented with known primary tumors. After brain-included whole-body FDG-PET/CT examination, the unknown primaries turned out to be bronchogenic carcinoma in 10 patients (33.3%), renal cell carcinoma in 2 patients (6.7%), and lymphoma in 2 patients (6.7%), yet the primary tumors remained unknown in 4 patients (13.3%). In 61 lesions (85.9%), the max SUV ranged from 0.2- < 10, while in 10 lesions (14.1%) the max SUV ranged from 10 to 20. Hypometabolic lesions were reported in 41 (57.7%) lesions, hypermetabolic in 3 lesions (4.2%), whereas 27 lesions (38.0%) showed similar FDG uptake to the corresponding contralateral brain matter. PET/CT overall sensitivity, specificity, positive and negative predictive, and accuracy values were 78.1, 92.6, 83.3, 90, and 88% respectively.
Conclusion
Brain-included whole-body FDG-PET/CT provides valuable complementary information in the evaluation of patients with suspected BM. However, the diagnostic performance of brain PET-CT carries the possibility of false-negative results with consequent false sense of security. The clinicians should learn about the possible pitfalls of PET/CT interpretation to direct patients with persistent neurological symptoms or high suspicion for BM for further dedicated CNS imaging.
Similar content being viewed by others
Background
Management protocols and treatment decisions in patients with brain tumors are based on a precise description of tumor extent. Brain metastases (BM) are the most common intracranial tumors in adults outnumbering all other intracranial tumors [1, 2]. The most common primary tumors causing brain metastases are lung, breast, melanoma, and colorectal cancers [3]. In around 10% of patients with BM, the primary tumor is unknown (cancer of unknown primary, CUP) [4, 5]. Currently, studies report that 72.2% of BM patients have solitary lesion [6], and nearly 37% have a minimum of three tumors [7]. The biological characteristics of the tumors are expected to affect the spatial distribution of their BM by a theory called “seed and soil.” This theory suggested a non-random distribution of metastases by special tumor cell properties and variances in microenvironments of different organs [8, 9]. In addition, BM distribution is dependent on an adequate supply and volume of cerebral blood; hence, BM varies in distribution with nearly 80% in the cerebral hemispheres, 15% in the cerebellum, or 5% in the brainstem [8]. Studies have shown a wide discrepancy in their estimations of the incidence proportions percentage of BM ranging from 3 to 50% [10]. In BM, headache, seizures, cognitive deficit, papilledema, and various focal neurological impairments are the main clinical manifestations [11]. BM in systemic cancers portends poor prognosis with a median survival of less than 6 months [12].
Imaging of BM can be conducted using many techniques considering that improved imaging techniques aid in early diagnosis and effective systemic treatment regimens. Of these techniques, contrast-enhanced CT is widely used owing to its accessibility, speed, and low cost. MRI with contrast is currently the procedure of choice, as MRI is more sensitive and specific than other imaging techniques in determining the presence, location, and number of metastases. MRI special sequences like arterial spin labeling (ASL) perfusion and diffusion tensor imaging (DTI) may be used for differentiating BM from primary brain tumors, e.g., gliomas. As assessment of combined ASL- and DTI-derived metrics of the peritumoral tissue may be useful in differentiating both pathologies [13]. Positron emission tomography (PET) can define metabolic activity (at the molecular level) of different subsets of metastatic brain tumor [5, 14]. [18F]-2-Fluoro-2-deoxy-d-glucose (FDG) is the most used PET tracer in nuclear medicine [15]. The combined PET/cross-sectional imaging can obtain functional and anatomic images on the same scanner without moving the patient [16]. PET/CT is more informative than PET alone in localizing increased FDG activity to specific normal or abnormal anatomic locations [17].
Currently, clinical demand for FDG-PET/CT is being increased in our clinical practice as a way to determine both body and brain metastatic disease overlooking the pitfalls of FDG-PET/CT in brain assessment. These pitfalls may challenge the modality capability to detect BM and make its use in this clinical context debatable. In this study, we aimed to assess the role and diagnostic performance of brain-included whole-body PET/CT modality in the detection and evaluation of BM and when further imaging is considered necessary. This was achieved by evaluating the scans and follow-up of patients diagnosed with extra-cranial malignancies who were referred to our institution for brain-included whole-body PET/CT for staging and re-staging. The results were compared to the published data in attempt to reach a conclusion and recommendation regarding the use of the assessed modality in clinical practice.
Methods
Study population
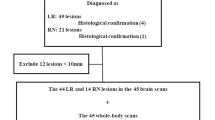
The studied group comprised 420 patients suffering from diagnosed or suspected extra-cranial malignancies referred to our hospital for brain-included whole-body PET/CT assessment and were followed up over a period of 12 months (Fig. 1). Informed consents were obtained from patients prior to conducting the current study, and the study was approved by our local research ethics committee. The clinical evaluation of all patients included full history taking, thorough clinical examination, laboratory evaluation, and other imaging modalities whenever available. Examinations were done and data were obtained using Siemens Bio-graph true point 64 PET/CT scanner. This dedicated system integrates a PET scanner with a multi-slice helical CT scanner permitting the acquisition of co-registered CT and PET images in one session. Inclusion criteria included patients diagnosed/suspected to have extra-cranial malignancy with no history of craniotomy, radiosurgery, or cerebral resection.
Imaging protocol
Patient preparation
All patients were asked to fast for 6 h prior to scan. The patients were instructed to stay in a warm quiet dark room devoid of distractions, and also asked to keep their movements, including talking, at an absolute minimum to avoid any kind of stimulation or activity prior to the examination and following injection of the radioisotope to avoid physiologic muscle uptake of FDG which can confound interpretation of the scan. Patients should be comfortable and relaxed. They were also asked to void immediately prior to scanning.
Serum glucose levels were routinely measured prior to FDG injection, and acceptable fasting levels were 70–170 mg/dl. The strategies for decreasing brown fat uptake were providing a controlled-temperature (warm) environment for patients before FDG injection and high-fat, low-carbohydrate, protein-permitted diet before the examination.
Dosage administration of FDG
About 1 L of negative oral contrast agent (5% mannitol) is ingested approximately 1 h before the exam. A dose of 0.1 mCi/kg of FDG IV injection 45–90 min before examination was administered. This period is referred to as the uptake phase and is the necessary amount of time for the FDG to be adequately bio-distributed and transported into the patient’s cells.
Scanning technique
CT scanning
Helical CT was performed following injection of about 125 ml (1-2 ml/kg) of iodinated contrast medium at a rate of 4 ml/s using a power injector. For a typical brain-included whole-body PET/CT study (head, neck, chest, abdomen, and pelvis), scanning began at the vertex of the skull and extended caudally to the level of the upper thighs.
PET scanning
PET was performed following the CT study without moving the patient. Approximately six to seven bed positions are planned in the three-dimensional acquisition mode for scanning the entire patient with 3-5-min acquisition at each bed position.
PET/CT fusion
Hundreds of trans-axial PET and CT images were first reconstructed. These are then reformatted into coronal and sagittal images to facilitate image interpretation. For each of these sets of PET and CT images, corresponding fusion images, combining the two types of data, also were generated. The whole acquisition time for an integrated PET/CT scan was approximately 25-30 min. PET image data sets were reconstructed using CT data for attenuation correction, and co-registered images were displayed using special software.
Image interpretation
For every patient, 2 independent experienced radiologists interpreted the images. Radiologists were aware of any patient’s clinical data. Discrepant interpretations between readers were resolved by consensus after simultaneous review and discussion. Assessment of radiotracer uptake by normal and pathologic tissues was evaluated visually and semi-quantitatively using maximum standardized uptake (SUV) values for each lesion and in comparison, to background activity. Abnormalities suggestive of metastatic disease were recorded which included number, location, size, and FDG uptake compared to normal brain matter. The reference standard for the current study regarding the accuracy determination of BM was made after clinical and radiological follow-up whenever available.
Statistical analysis
The data collected were tabulated and analyzed by SPSS (Statistical Package for the Social Science Software) statistical package version 22 on IBM-compatible computer qualitative data were described using number and percent. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of FDG-PET/CT were determined compared to contrast-enhanced CT (CECT) using patients’ data as reference.
Results
The study group comprised of 420 patients suffering from extra-cranial malignancies. Thirty patients had brain lesions with a median age of 58 years (range 45-77, mean ± SD 58.2 ± 9.4 years) and distributed as n = 16 males (53.3%) and n = 14 females (46.7%). Negative radiological findings for brain lesions were initially reported in 390 patients from whom follow-up data could be obtained for 70 patients (the rest of the patients were missed due to losing contact or death). All patients were followed-up over 12 months period for the development of any neurological complaints or positive brain imaging studies.
Table 1 shows the distribution of the studied cases according to the primary malignancy diagnosis and the clinical presentations. The suspected BM of unknown origin were n = 18 (60.0%), from which the unknown primaries identified following whole-body FDG-PET/CT examination were n = 14 (46.7%); while the unknown primaries that remained unidentified were n = 4 (13.3%). Twelve patients (40.0%) presented for reassessing and restaging of known primary tumors that caused BM. The number of patients suffered from bronchogenic carcinoma were (n = 15, 50%) and classified according to histopathological types into adenocarcinoma (n = 7, 23.3%), squamous cell carcinoma (n = 5, 16.7%), and small cell lung cancer (n = 3, 10.0%). Patients presented with systemic metastases along with BM were 16 patients (53.3%) and detected as bony, nodal, lung, suprarenal, hepatosplenic, and subcutaneous deposits while 14 patients (46.7%) presented with BM without systemic metastases. From those suffered from systemic metastases, 6 patients (37.5%) had bronchogenic carcinoma as the primary tumor. These results showed that bronchogenic carcinoma was the most common primary tumor both in the previously diagnosed patients and as more commonly presenting metastases of unknown origin.
Table 2 shows the 71 brain lesions identified in all 30 patients distributed according to anatomical features; number, site, and laterality, while Table 3 shows morphological features of brain lesions including size, shape, special features; calcification and hemorrhage, pattern of enhancement, presence of edema, SUV max, and compared to the corresponding contralateral normal brain matter. The results showed that multiple brain lesions were more common than solitary lesions. Supratentorial metastases were more than the infratentorial being present in 100% of patients.
Regarding the pattern of enhancement, the studied lesions showed marginal enhancement (n = 32, 45.1%), ring enhancement (n = 12, 16.9%), intralesional enhancement (n = 10, 14.1%), and non-enhancement (n = 17, 23.9%) lesions. Some of the lesions showed patchy areas of no enhancement and no radiotracer uptake due to associated elements of necrosis, calcifications, or hemorrhage. None of the studied patients had lepto-meningeal lesion or abnormal enhancement.
SUV were measured and compared to the corresponding contralateral normal brain tissue. In 61 lesions (85.9%), the max SUV ranged from 0.2- < 10, while in 10 lesions (14.1%) the max SUV ranged from 10 to 20. When compared to the corresponding contralateral brain tissue, 41 lesions (57.7%) showed less FDG uptake than the corresponding contralateral brain matter, i.e., hypometabolic (Fig. 2), 3 lesions (4.2%) showed more FDG avidity than corresponding contralateral brain matter, i.e., hypermetabolic (Figs. 3 and 4), whereas 27 lesions (38.0%) showed similar FDG uptake to the corresponding contralateral brain matter (Fig. 5). A case presented with multiple variable-sized brain space-occupying lesions with small lesion that was not appreciated in the PET image (Fig. 6).
Axial CT (right), fused (middle), and PET (left) brain images in brain-included whole-body FDG-PET/CT examination routine follow-up for a patient with thyroid carcinoma showed solitary, right sided, occipital, ovoid sizable lesion (black arrows) with diffuse intralesional enhancement and minimal vasogenic edema. Its max SUV was 4.2, less than surrounding and corresponding contralateral gray matter
Axial CT (right), fused (middle), and PET (left) brain images of brain-included whole-body FDG-PET/CT showed two solid rounded lesions, showing diffuse enhancement metastatic lesions. a Small right parietal lesion (black arrow) and b larger right temporal lesion (black arrow). The max SUV was 6.4, greater than surrounding and corresponding contra lateral gray matter. The primary tumor turned out to be right central bronchogenic carcinoma
Axial CT (right), fused (middle), and PET (left) brain images of brain-included whole-body FDG PET/CT showing bilateral brain metastatic lesions of unknown primary showing ring enhancement pattern (black arrows) with max SUV 11.4 which is greater than the FDG uptake in the surrounding and contralateral gray matter. The primary tumor turned out to be lymphoma
Axial CT (right), fused (middle), and PET (left) brain images of brain-included whole-body FDG PET/CT showing right temporal lesion (black arrow) that appears as a subtle hypodense area in CT with max SUV 4 which is nearly equal to the FDG uptake in the surrounding and contralateral gray matter. The primary tumor turned out to be right middle lobar bronchogenic carcinoma
A 65-year-old male patient presented with refractory headache. Brain-included whole-body FDG-PET/CT examination revealed a multiple variable-sized brain space-occupying lesions (black arrows). Small lesion (arrowhead) is seen in the CT image and not appreciated in the PET image. b Scans through the chest showed the primary tumor to be right lung cancer with concomitant pleural involvement
Table 4 shows the diagnostic performance of both PET/CT and contrast-enhanced CT techniques to detect BM. The true positive cases by PET/CT and contrast-enhanced CT were 25/30 and 26/30 patients, respectively, false positive: 5 and 4 patients, respectively, true negative: 63 and 64 patients respectively, and false negative: 7 and 6 patients, respectively. The sensitivity, specificity, PPV, NPV, and accuracy of FDG-PET/CT and contrast-enhanced CT in BM patient-based were as follows: the sensitivity of PET/CT examinations was 78.1%, specificity was 92.6%, PPV and NPV of PET/CT were 83.3%, and 90.0% respectively and 88% accuracy, while the sensitivity of CT alone was 81.2%, specificity was 94.1%, PPV and NPV were 86.7% and 91.4% respectively and 90% accuracy. Of the 5 false-positive patients diagnosed by FDG-PET/CT, 3 patients were proved to have old cerebral infarctions by MR, and 2 patients were interpreted as false positive due to uneven uptake of FDG tracer by the cortex cerebri on PET. Seven patients with initially negative scan complained from persistence of neurological symptoms, and MRI was done within 1-2 weeks from PET/CT scan that revealed positive MRI findings, e.g., small parenchymal lesions and leptomeningeal involvement. This MRI results reflected false-negative results of PET/CT scan.
Discussion
PET/CT is a widely used imaging modality in oncology owing to its whole-body imaging coverage allowing detection of metastases in a large part of the body. Routinely, a whole-body PET/CT covers from the skull base to upper thigh region that can be described as lips- to-hips or eyes-to-thighs excluding the brain which makes the term whole body imprecise.
FDG-PET’s role in detecting BM has been frequently questioned in literature and limited due to its low sensitivity [5, 18, 19]. However, this sensitivity increased with the introduction of IV contrast and the development of new fast CT scanners [20]. We addressed the role of including the brain in cancer patient’s whole-body scans to increase the probability of BM being detected. Hence, the term “detection” as part of our aim was more toward the clinical application of the examination making more sense of the name “Whole body scan” and to be used as a single stop shop for patient’s full assessment including the brain saving effort, time, and cost especially in low economy regions.
We examined 420 cases of extra-cranial malignancy from which 30 patients presented with 71 BM lesions with an incidence of 7.1%. Current literature reviewing incidence of BM showed high variability with an incidence proportions percentage ranging from 3 to 50% [10]. This could be explained in the context of methodological constraints related to inconsistency of studied data. The published data could be derived from population-, histology-, radiologic-, surgical-, or medical record-based data studies [4, 12, 21]. In addition, other epidemiological variables as age, sex, race, and regional area (North Africa in our case) can be responsible for the reported variations [10].
In the current study, bronchogenic carcinoma was the most common primary tumor both in the previously diagnosed patients and as more commonly presenting metastases of unknown origin [22]. These results are in accordance with most of the published data where autopsy studies have suggested that lung cancer is the most common tumor to cause BM accounting for two-thirds of patients [12, 23]. In our study, the most common histologic subtype associated with the development of BM was adenocarcinoma. This is in line with prior findings which may be related to the fact that adenocarcinoma is the most common histologic subtype of lung cancer overall [24]. In descending order, the common cancers to send BM in our study were breast carcinoma, renal cell carcinoma, melanoma, non-Hodgkin lymphoma, and thyroid carcinoma. Comparably, studies showed that breast cancer has the second most frequent incidence of BM, where autopsy studies reported an incidence rate of 18–30% [1, 25]. Melanoma is the third most common cause of BM and accounts for nearly 6–11% of lesions, with a higher incidence of metastasis in males [26]. It was reported that 50% of advanced melanoma patients developed BM and 10% of metastatic lesions presented as an intraparenchymal hemorrhage [26]. With respect to renal cell carcinoma, it was estimated that BM occurred in 2–16% of patients and that when BM emerged late in illness, renal cell carcinoma was refractory to other therapies [27]. BM is an unusual event for patients with aggressive lymphoma [28, 29]. Thyroid cancer remote metastasis to the brain occurred in about 0.3-4.6% of cases and was associated with aggressive behavior and worse prognosis [30,31,32]. Studies have shown that FDG-PET/CT detected location in nearly 25% of unknown primary disease patients [33, 34].
Neurological symptom presence may indicate BM. In this study, 16/30 patients (53.3%) with BM had neurological symptoms, whereas the remaining 14/30 patients (46.7%) had no neurological symptoms which represented nearly half of the studied patients. Patients with BM tended to be more appropriately diagnosed as positive by PET/CT in the symptomatic rather than in non-symptomatic patients. This is concordant with the published literature where Kitajima et al.’s study showed no statistical significance between these two patient groups [35]. A study proposed by Nia et al. showed that all studied patients with incidental BM were symptom free [36]. It is important to diagnose BM before patients become symptomatic to avoid dangerous complications as seizures.
Regarding the number of brain lesions, multiple lesions were more common than solitary lesions which agree with the published data [11, 25]. According to site, supratentorial metastases were present in 100% of patients with the parietal lesions representing 50.7%, while infratentorial lesions were detected in 26.7% of the studied patients. Similar results were reported by Delattre et al. [37] and Nussbaum et al. [38] where the supratentorial area was the preferential area for metastasis that can be explained in the context of the respective mass of these structures. This anatomical distribution of the BM being supratentorial in 100% of our studied patients justify the importance of including the brain in the scanned field; otherwise, they would not have been discovered with the routine base of the skull–to–thigh protocol.
In the current study, the enhancement patterns detected varied from none to marginal, ring- and intralesional enhancement. Some of the lesions showed patchy areas of no enhancement and no radiotracer uptake due to associated element of necrosis, calcifications, or hemorrhage. Schwartz et al. evaluated 221 ring-enhancing brain lesions and found that the most frequent pathologies associated with ring-enhancing lesions were gliomas (40%) followed by BM 30% [39].
The intensity of FDG uptake was variable in the current study, where the max SUV value was measured for every lesion separately, the least was 0.2 and the most was 20. In attempt to appropriately assess the FDG uptake by the metastatic deposits in the presence of hypermetabolic background of normal brain tissue, we compared the FDG uptake to the corresponding contralateral gray matter uptake to set a reference range that is reliable for every patient during their specific status of examination. It was noticed that FDG avidity varied in the studied lesions when compared to the corresponding contralateral brain tissue showing iso-, hypo-, and hyper-avidity. It is worth mentioning that bronchogenic carcinoma metastatic deposits exhibited all three FDG uptake varieties.
Analysis of FDG-PET/CT diagnostic performance in the current study showed a moderately good sensitivity (78.1%) and specificity (92.6%) with an insignificant difference in performance as compared to CECT modality alone. In accordance with our data, Hjorthaug et al. studied lung cancer patients with suspected BM using FDG PET/CT as a triage for selecting patients who need further imaging. This study showed PET/CT sensitivity, specificity, and PPV were 72, 100, and 97%, respectively [40]. Several FDG-PET studies have demonstrated a broad range of sensitivities and specificity for identifying brain tumors, whether as known primary brain tumors or recurrence after treatment, ranging from 25–100% and 22-100%, respectively [41]. Sensitivity is limited by false-negative cases that resulted from absent or reduced FDG uptake by suspected brain tumors compared to surrounding normal brain tissue. Meanwhile, specificity is limited by false-positive cases as in cases of inflammation [42, 43].
FDG has been the tracer of choice for oncologic PET imaging, based on the principle of increased glucose metabolism by most tumors [44], long half-life, easy synthesis [15, 45]. Despite its recognized limitations in brain tumor imaging due to the high uptake in the background of normal gray matter, this imaging modality tracer remains the most used nowadays [15, 45]. FDG provides a comprehensive picture of the tumor, predicting aggressiveness, helping to differentiate recurrent tumors from treatment-related changes, and differentiating pharmaco-sensitive tumors [45]. Recent technical improvement in several PET/CT protocols including the implementation of intravenous contrast resulted in improvement of the overall yield of the hybrid study in detecting BM to exceed the reported low sensitivity of a PET alone. Adding that to the whole body coverage (including head) and the accessibility to faster scanners, the CT component of the PET/CT study can work as an independent CT scan of the brain with the possibility to preclude the requirement for a dedicated diagnostic brain CT.
Limitations of the FDG-PET/CT should be recognized. Previous studies suggested limitation of PET scanning as possible false-negative results that could lead to inaccurate disease staging. In a prior study by Kruger et al., BM detected by PET-CT were evident only on the CECT portion of the examination, with FDG-PET only detecting altered metabolism in 1/8 patients [46]. In some patients, particularly those with neurological complaints, there is still a need for more imaging despite the improved diagnostic performance of PET/CT. False sense of security from negative PET/CT results should be regarded and the treating physicians must be informed about the study limits so as to avoid errors in treatment due to potentially misleading PET/CT results. Additionally, logistic issues like scanning time in an active PET service and the extra brain scanning time will reduce the overall number of patients scanned per day [19]. Radiation exposure could be considered a downside of the discussed modality; however, Osipov et al. showed that diagnostic exposure due to repeated PET-CT examinations in a group of oncological patients was not associated with changes in mortality [47]. Reduced kilovolts (kVs) with automatic exposure control were a suggested attempt to optimize the radiation exposure in head and neck scans [48].
We should recognize limitations in the current study as there was lack of a histological proof as a true reference standard for some of the detected lesions. With a reference standard based on imaging, false negatives may arise in small or slowly growing lesions in the absence of substantial morphological changes. Nevertheless, comparable with numerous studies of similar design, acquiring multiple biopsies for tissue confirmation would have been unfeasible and ethically unacceptable [20, 49]. Another recognized limitation could be the number of the studied cases which could have led to underestimating the incidence of BM. We believe that there are sources of bias as the defect in referral system, systemic brain study is not routinely performed or patients with end-stage diseases that may be considered untreatable may not have been included. Further studies aimed at improving brain PET/CT performance and a systemic diagnostic evaluation of FDG-PET/CT for the differentiation of the brain tumor are therefore essential.
Conclusion
No single modality can provide a full answer to a complex clinical question in oncology patients. Brain-included whole-body FDG-PET/CT provides valuable complementary information in the evaluation of patients with suspected BM that can be used for presumptive diagnosis to direct therapeutic decision-making and can be integrated in the routine workup protocols. However, considering the obtained results of the diagnostic performance of brain PET-CT, the possibility of false-negative results with consequent false sense of security should be considered especially in patients with suspicious neurological clinical manifestation. Those patients should have further dedicated CNS imaging for confirmation. Hence, the clinicians should learn about the possible pitfalls of PET/CT interpretation, and the prudent use of further standard brain imaging techniques needs to be promoted.
Availability of data and materials
The data used or analyzed during the study are available from the corresponding author on reasonable request.
Abbreviations
- BM:
-
Brain metastases
- CT:
-
Computed tomography
- FDG:
-
[18F]-2-Fluoro-2-deoxy-d-glucose
- PET:
-
Positron emission tomography
- SUV:
-
Maximum standardized uptake
References
Ostrom QT, Wright CH, Barnholtz-Sloan JS (2018) Brain metastases: epidemiology. Handb Clin Neurol 149:27–42. https://doi.org/10.1016/B978-0-12-811161-1.00002-5
Dirven L, Taphoorn MJB (2020) Epidemiology of central nervous system metastases. In: Ahluwalia M, Metellus P, Soffietti R (eds) Central nervous system metastases. Springer, Cham, pp 3–14
Walker AE, Robins M, Weinfeld FD (1985) Epidemiology of brain tumors: the national survey of intracranial neoplasms. Neurology 35:219–226. https://doi.org/10.1212/wnl.35.2.219
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14:48–54. https://doi.org/10.1007/s11912-011-0203-y
Galldiks N, Langen KJ, Albert NL, Chamberlain M, Soffietti R, Kim MM et al (2019) PET imaging in patients with brain metastasis-report of the RANO/PET group. Neuro Oncol 21:585–595. https://doi.org/10.1093/neuonc/noz003
Stark AM, Stohring C, Hedderich J, Held-Feindt J, Mehdorn HM (2011) Surgical treatment for brain metastases: prognostic factors and survival in 309 patients with regard to patient age. J Clin Neurosci 18:34–38. https://doi.org/10.1016/j.jocn.2010.03.046
Fabi A, Felici A, Metro G, Mirri A, Bria E, Telera S et al (2011) Brain metastases from solid tumors: disease outcome according to type of treatment and therapeutic resources of the treating center. J Exp Clin Cancer Res 30:10. https://doi.org/10.1186/1756-9966-30-10
Mustafa DA, Pedrosa R, Kros JM (2020) Pathology of brain metastasis. In: Ahluwalia M, Metellus P, Soffietti R (eds) Central nervous system metastases. Springer, Cham, pp 15–29
Graf AH, Buchberger W, Langmayr H, Schmid KW (1988) Site preference of metastatic tumours of the brain. Virchows Arch A Pathol Anat Histopathol 412:493–498. https://doi.org/10.1007/BF00750584
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22:2865–2872. https://doi.org/10.1200/JCO.2004.12.149
Saha A, Ghosh SK, Roy C, Choudhury KB, Chakrabarty B, Sarkar R (2013) Demographic and clinical profile of patients with brain metastases: a retrospective study. Asian J Neurosurg 8:157–161. https://doi.org/10.4103/1793-5482.121688
Pruitt AA (2017) Epidemiology, treatment, and complications of central nervous system metastases. Continuum 23:1580–1600. https://doi.org/10.1212/CON.0000000000000551
Abdel Razek AAK, El-Serougy L, Abdelsalam M, Gaballa G, Talaat M (2019) Differentiation of primary central nervous system lymphoma from glioblastoma: quantitative analysis using arterial spin labeling and diffusion tensor imaging. World Neurosurg 123:e303–e3e9. https://doi.org/10.1016/j.wneu.2018.11.155
Werner JM, Lohmann P, Fink GR, Langen KJ, Galldiks N (2020) Current landscape and emerging fields of PET imaging in patients with brain tumors. Molecules 25. https://doi.org/10.3390/molecules25061471
Basu S, Alavi A (2009) Molecular imaging (PET) of brain tumors. Neuroimaging Clin N Am 19:625–646. https://doi.org/10.1016/j.nic.2009.08.012
Beyer T, Townsend DW, Brun T, Kinahan PE, Charron M, Roddy R et al (2000) A combined PET/CT scanner for clinical oncology. J Nucl Med 41:1369–1379
Kapoor V, McCook BM, Torok FS (2004) An introduction to PET-CT imaging. Radiographics 24:523–543. https://doi.org/10.1148/rg.242025724
Lai G, Mahadevan A, Hackney D, Warnke PC, Nigim F, Kasper E et al (2015) Diagnostic accuracy of PET, SPECT, and arterial spin-labeling in differentiating tumor recurrence from necrosis in cerebral metastasis after stereotactic radiosurgery. AJNR Am J Neuroradiol 36:2250–2255. https://doi.org/10.3174/ajnr.A4475
Rohren EM, Provenzale JM, Barboriak DP, Coleman RE (2003) Screening for cerebral metastases with FDG PET in patients undergoing whole-body staging of non-central nervous system malignancy. Radiology 226:181–187. https://doi.org/10.1148/radiol.2261010920
Dirisamer A, Halpern BS, Flory D, Wolf F, Beheshti M, Mayerhoefer ME et al (2010) Integrated contrast-enhanced diagnostic whole-body PET/CT as a first-line restaging modality in patients with suspected metastatic recurrence of breast cancer. Eur J Radiol 73:294–299. https://doi.org/10.1016/j.ejrad.2008.10.031
Leece R, Xu J, Ostrom QT, Chen Y, Kruchko C, Barnholtz-Sloan JS (2017) Global incidence of malignant brain and other central nervous system tumors by histology, 2003-2007. Neuro Oncol 19:1553–1564. https://doi.org/10.1093/neuonc/nox091
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94:2698–2705. https://doi.org/10.1002/cncr.10541
Alexandru D, Bota DA, Linskey ME (2012) Epidemiology of central nervous system metastases. Prog Neurol Surg 25:13–29. https://doi.org/10.1159/000331167
Dagogo-Jack I, Gill CM, Cahill DP, Santagata S, Brastianos PK (2017) Treatment of brain metastases in the modern genomic era. Pharmacol Ther 170:64–72. https://doi.org/10.1016/j.pharmthera.2016.10.011
Pope WB (2018) Brain metastases: neuroimaging. Handb Clin Neurol 149:89–112. https://doi.org/10.1016/B978-0-12-811161-1.00007-4
Lu-Emerson C, Eichler AF (2012) Brain metastases. Continuum 18:295–311. https://doi.org/10.1212/01.CON.0000413659.12304.a6
Hanzly M, Abbotoy D, Creighton T, Diorio G, Mehedint D, Murekeyisoni C et al (2015) Early identification of asymptomatic brain metastases from renal cell carcinoma. Clin Exp Metastasis 32:783–788. https://doi.org/10.1007/s10585-015-9748-8
Bernstein SH, Unger JM, Leblanc M, Friedberg J, Miller TP, Fisher RI (2009) Natural history of CNS relapse in patients with aggressive non-Hodgkin’s lymphoma: a 20-year follow-up analysis of SWOG 8516 -- the Southwest Oncology Group. J Clin Oncol 27:114–119. https://doi.org/10.1200/JCO.2008.16.8021
El-Galaly TC, Villa D, Michaelsen TY, Hutchings M, Mikhaeel NG, Savage KJ et al (2017) The number of extranodal sites assessed by PET/CT scan is a powerful predictor of CNS relapse for patients with diffuse large B-cell lymphoma: an international multicenter study of 1532 patients treated with chemoimmunotherapy. Eur J Cancer 75:195–203. https://doi.org/10.1016/j.ejca.2016.12.029
Henriques de Figueiredo B, Godbert Y, Soubeyran I, Carrat X, Lagarde P, Cazeau AL et al (2014) Brain metastases from thyroid carcinoma: a retrospective study of 21 patients. Thyroid 24:270–276. https://doi.org/10.1089/thy.2013.0061
Ikekubo K, Hino M, Ito H, Hirao K, Ueshima M, Tanaka T et al (2000) Seven cases of brain metastasis from papillary thyroid carcinoma. Kaku igaku Jpn J Nucl Med 37:349–357
Gomes-Lima CJ, Wu D, Rao SN, Punukollu S, Hritani R, Zeymo A et al (2019) Brain metastases from differentiated thyroid carcinoma: prevalence, current therapies, and outcomes. J Endocr Soc 3:359–371. https://doi.org/10.1210/js.2018-00241
Verma V, Choi JI, Sawant A, Gullapalli RP, Chen W, Alavi A et al (2018) Use of PET and other functional imaging to guide target delineation in radiation oncology. Semin Radiat Oncol 28:171–177. https://doi.org/10.1016/j.semradonc.2018.02.001
Rusthoven KE, Koshy M, Paulino AC (2004) The role of fluorodeoxyglucose positron emission tomography in cervical lymph node metastases from an unknown primary tumor. Cancer 101:2641–2649. https://doi.org/10.1002/cncr.20687
Kitajima K, Nakamoto Y, Okizuka H, Onishi Y, Senda M, Suganuma N et al (2008) Accuracy of whole-body FDG-PET/CT for detecting brain metastases from non-central nervous system tumors. Ann Nucl Med 22:595–602. https://doi.org/10.1007/s12149-008-0145-0
Nia ES, Garland LL, Eshghi N, Nia BB, Avery RJ, Kuo PH (2017) Incidence of brain metastases on follow-up (18)F-FDG PET/CT scans of non-small cell lung cancer patients: should we include the brain? J Nucl Med Technol 45:193–197. https://doi.org/10.2967/jnmt.117.194571
Delattre JY, Krol G, Thaler HT, Posner JB (1988) Distribution of brain metastases. Arch Neurol 45:741–744. https://doi.org/10.1001/archneur.1988.00520310047016
Nussbaum ES, Djalilian HR, Cho KH, Hall WA (1996) Brain metastases. Histology, multiplicity, surgery, and survival. Cancer 78:1781–1788
Schwartz KM, Erickson BJ, Lucchinetti C (2006) Pattern of T2 hypointensity associated with ring-enhancing brain lesions can help to differentiate pathology. Neuroradiology 48:143–149. https://doi.org/10.1007/s00234-005-0024-5
Hjorthaug K, Hojbjerg JA, Knap MM, Tietze A, Haraldsen A, Zacho HD et al (2015) Accuracy of 18F-FDG PET-CT in triaging lung cancer patients with suspected brain metastases for MRI. Nucl Med Commun 36:1084–1090. https://doi.org/10.1097/MNM.0000000000000371
Zhao C, Zhang Y, Wang J (2014) A meta-analysis on the diagnostic performance of (18)F-FDG and (11)C-methionine PET for differentiating brain tumors. AJNR Am J Neuroradiol 35:1058–1065. https://doi.org/10.3174/ajnr.A3718
Chen W (2007) Clinical applications of PET in brain tumors. J Nucl Med 48:1468–1481. https://doi.org/10.2967/jnumed.106.037689
Shreve PD, Anzai Y, Wahl RL (1999) Pitfalls in oncologic diagnosis with FDG PET imaging: physiologic and benign variants. Radiographics 19:61–77; quiz 150-1. https://doi.org/10.1148/radiographics.19.1.g99ja0761
Weber G (1977) Enzymology of cancer cells (first of two parts). N Engl J Med 296:486–492. https://doi.org/10.1056/NEJM197703032960905
Zimmer L, Luxen A (2012) PET radiotracers for molecular imaging in the brain: past, present and future. NeuroImage 61:363–370. https://doi.org/10.1016/j.neuroimage.2011.12.037
Kruger S, Mottaghy FM, Buck AK, Maschke S, Kley H, Frechen D et al (2011) Brain metastasis in lung cancer. Comparison of cerebral MRI and 18F-FDG-PET/CT for diagnosis in the initial staging. Nuklearmedizin 50:101–106. https://doi.org/10.3413/Nukmed-0338-10-07
Osipov M, Vazhenin A, Kuznetsova A, Aksenova I, Vazhenina D, Sokolnikov M (2020) PET-CT and occupational exposure in oncological patients. SciMed J 2:63–69. https://doi.org/10.28991/SciMedJ-2020-0202-3
Gómez AML, Santana PC, Mourão AP (2020) Dosimetry study in head and neck of anthropomorphic phantoms in computed tomography scans. SciMed J 2:38–43. https://doi.org/10.28991/SciMedJ-2020-0201-6
Murakami R, Kumita S, Yoshida T, Ishihara K, Kiriyama T, Hakozaki K et al (2012) FDG-PET/CT in the diagnosis of recurrent breast cancer. Acta Radiol 53:12–16. https://doi.org/10.1258/ar.2011.110245
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YZ, KN, and MZ conceived of the study, participated in its design, and supervised the selection of cases and controls. MZ and RH conducted the clinical part of the imaging, reviewed cases and carried the statistical analysis, and drafted and finalized the manuscript. All authors read and approved the final manuscript and accepted the publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was obtained from the participants prior to the study. The study has been carried out following the approval of the Ethics Committee of the Faculty of Medicine Alexandria University in accordance with Helsinki Declaration (reference number: 0104276).
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zidan, M.A., Hassan, R.S., El-Noueam, K.I. et al. Brain metastases assessment by FDG-PET/CT: can it eliminate the necessity for dedicated brain imaging?. Egypt J Radiol Nucl Med 51, 223 (2020). https://doi.org/10.1186/s43055-020-00342-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00342-8