Abstract
Background
Bone metastasis can be noted in the course of many primary malignant neoplastic lesions; breast and prostate cancers are the most frequent, but lung, kidney, and thyroid malignancies frequently metastasize to bones. Secondary osseous lymphomatous infiltrations is relatively uncommon and mainly noted in patients with non-Hodgkin lymphoma (NHL). By adding the metabolic changes to the conventional CT morphologic changes, combined positron emission tomography (PET) and computed tomography (CT) may offer clinically useful addition in assessment of treatment response of these lesions and offer helpful judgment for the different oncologic therapeutic regimens.
Results
The study included 45 patients, 24 females (53.33%) and 21 males (46.66%). Showing bone dominant or isolated bony secondary malignant infiltrations. The study included 24 patients with history of breast cancer (53.33%), 12 patients with history of lymphoma (26.66%), and 9 patients (20%) with history of lung cancer. All the bony lesions included in the study were multiple lesions in each patient, classified into mixed lytic and sclerotic bony lesions in 21 patients (46.66%), sclerotic lesions in 12 patients (26.66%), and radiologically occult lesions or osteopenic areas in 12 patients (26.66%). The most accurate SUV max cut-off value among studied cases was 4, taking the lesion with highest SUV max value as the reference standard, with measurements taken before and after the medical regimen with six months interval. Confirmation of PET/CT results was done by serial post management follow up at 6 months interval and 1 year interval.
Conclusion
PET/CT study is an effective tool for assessment of treatment response for ossoues secondary malignant lesions.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Secondary malignant bony lesions can occur in patients with advanced cancer and can cause signifiacnt morbidity and disability. Pain, mechanical disability, spinal cord compression, and pathological fractures could occur as a sequel to bone secondary malignancies [1]. Secondary bony lesions could be classified into lytic, sclerotic or radiologically occult, or mixed according to its morphology [2].
Evaluation of treatment response as early as possibe is mandatory to make the correct treatment decisions; accurate techniques are needed for monitoring the treatment response [3].
Although bone scintigraphy was the imaging modality of choice for decades for evaluation of bony secondary neoplastic lesions, yet it has limitations in its sensitivty and specificity and limitation in assessment of treatment response with poor anatomical details [4, 5]. Computed tomography (CT) assessment misses the early bone marrow lesions with negative CT morphological changes; CT also is limited in differntiating the active metastatic sclerotic bony lesions from the healed sclerotic ossoeus lesions with the same morphological pattern [6].
By adding the functional metabolic data to the morphological data obtained in the fused PET/CT images, advance in secondary osseous malignant lesions knowledge can be achieved including its detection, characterization, and assessment of teatment response [7].
Methods
This is a retrospective analysis of 45 patients with primary malignancies developed secondary osseous lesions.
The visual assessment method and semi-quantitative analysis were used with measuring the standard uptake value (SUV) max and the normal would be the normal blood pool liver SUV max.
Inclusion criteria
-
Patients with primary malignant lesions with bone dominant or isolated bony metastatic disease
-
Patients with history of non Hodgkin lymphoma developed secondary osseous infiltrations
Exclusion criteria
-
Primary malignant ossoeus lesions
-
Bone deposits due to primary prostate malignant lesion
-
Pediatric population
Technique
A hybrid PET/CT scanner (Siemens Biograph 64 PET/CT scanner) was used in this study. Before the examination by 6 h, the patients were instructed to fast, except for water. Avoidance of (extreme) exercise for at least 6 h before the study was asked to minimize 18FDG uptake in muscles and to reduce the false positive results. The allowable blood glucose level for the study was of < 150 mg/dL. Voiding of urine was done before injection, and then approximately 5 MBq/kg body weight of 18 FDG was injected. Further, 60–90 min later, the data were acquired [8]. The patients then were kept lying comfortably and were asked not to talk to avoid false positive uptake. A noncontrast-enhanced CT from mid-thigh to the skull was obtained 60 min after the tracer injection. Nuclear medicine consultant and radiology consultant interpreted the data at Siemens work station.
The lesion with the highest SUVmax was taken and studied befroe and after the treatment algorithm
Ethics approval and consent to participate
All the patients included in this study gave written informed consent to publish the data contained within this study. Approval for this study was obtained from the Research Ethics Committee of our medical institute. All study procedures were carried out in accordance with the Declaration of Helsinki regarding research involving human subjects.
Results
The study included 45 patients, 24 females (53.33%) and 21 males (46.66%). Showing bone dominant secondary malignant infiltrations (Table 1).
The study included 24 patients with history of breast cancer (53.33%), 12 patients with history of lymphoma (26.66%), and 9 patients (20%) with history of lung cancer lung (Table 1); all with osseous dominant metastatic disease.
All the bony lesions included in the study were multiple lesions in each patient.
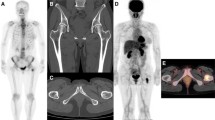
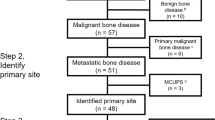
The lesions are classified according to the CT morphology into mixed lytic and sclerotic bony lesions in 21 patients (46.66%) (Fig. 1), radiologically occult lesions in 12 patients (26.66%) (Fig. 2), and sclerotic lesions in 12 patients (26.66%) (Fig. 3).
Follow up post chemotherapy regimen for patient with cancer breast and isolated bony metastatic disease a axial CT bone window and b, c corresponding PET/CT fused image showing multiple iliac and sacral lesions, the lesion with highest SUV max value was the lytic lesion targeting the posterior asepct of the right iliac bone SUV max: 6.8 (arrow in b). d Axial CT pelvis and e corresponding PET/CT fused image 6 months following the chemotherapy; the lesion shows relative increase density in the CT image and signifnact decrease in FDG uptake (arrow); the SUV max value reaching 2 treatment responder
A 56-year-old male patient with history of NHL. a Conventional CT study showing no gross lytic or sclerotic lesions noted within the sternum and DV5 body. b, c Corresponding PET/CT fused image shows focal FDG uptake in the sternum and DV5 vertebral body matching with radiologically occult bone marrow infiltration, SUV Max of the vertebral lesion: 4.05 d 7 months post treatment PET/CT fused image showing complete metabolic response with disappearance of the metabolically active bone marrow lesions by the visual assessment method
Assessment of treatment response of patient with history of cancer breast and isolated bony metastatic disease with sclerotic metastatic lesions. a Axial CT bone window setting with sclertoic lesion noted in the rigth ischium (arrow). b Corresponding PET image showing avid uptake in the right ischium anatomical site. c Axial CT pelvis 6 months post treatment PET/CT study with sclerotic morhpolgy of the right ischium could represent sclerotic metastatic lesion or healed lesion. d Corresponding PET image shows no uptake within the lesion impressive of complete metabolic response
The most accurate SUV max cut-off value among studied cases was 4, taking the lesion with highest SUV max value as the reference standard, with measurements taken before and after the medical regimen with six months interval.
The lesions were classified according to the PET/CT results in to two groups: responder in 36 patients with appreciable decrease in the SUV max after treatment (80%) and non responders in 9 patients (20%) with notification of denovo osseous lesions (Table 1).
Confirmation of PET/CT results was done by serial post management follow up at 6 months interval (Fig. 4).
Follow up post chemotherapy regimen for patient with history of breast cancer. a Axial CT bone window showing isolated lytic ossoeus lesion targeting CV7 right pedicle.b Correponding PET axial image. c Corresponding PET/CT fused image showing avid uptake within the lesion by visual assessment method, SUV max: 7. d Axial CT bone window 6 months post chemotherapy regimen. e Corresponding PET axial image and f fused PET/CT image showing no appreciable interval changes. Non responder
Discussion
A weakness point of conventional imaging techniques is its inability to early measure the effect of treatment upon the isolated or dominant bony secondary malignant lesions, an area where functional imaging may be of benefit for response assessment [9].
Our study suggested that 18 FDG uptake by the ossoeus lesions reflect the metabolic neoplastic activity of the lesions regardless of its CT morphological pattern either lytic or sclerotic or radiologically occult.
Generally, there is no universally accepted technique for assessment of treatmane response of bone deposits. A combination of imaging, laboratory, and clinical symptoms assessment (pain relief, movement limitations improvement) for response assessment are used. Bone scan was the imaging modality of choice for assessment of bone deposits for decades yet limited by the poor spatial resolution, as well as false positive results. Flare phenomenon occurs within 2 weeks to 3 months post treatment that describes the avid uptake of the tracer during the healing process of the metastatic lesion which could be falsely intepreted as progressive disease [9,10,11].
Whole-body diffusion magnetic resonance imaging (WB-DWI) is a well-established technique with multiple advantages: no exposure to ionizing radiatation, no injection of radioactive agents with its pre-injection and post injection precautions, even with no contrast material injection. In his study, Padhani et al. [12] concluded that it can make signifiacnt impact on therapy assessment. The disadvantages of the technique is relative limitations in assessment of mineralized lesions and sclerotic deposits [12].
In this study, 18FDG was used in the PET/CT study; it is widely used radioactive agent yet with limitation in uptake in certain malignancies like cancer prostate. Cook G et al. [13] supported the use of other PET/CT agents for cancer prostate bone deposits assessment; Choline, labeled either with 11C-carbon or 18F-fluorine, has become a standard clinical tracer for staging high-risk prostate cancer and patients with biochemical recurrence [13].
The SUV max cut-off value among studied cases was 4 , we used in this study the SUV max unit , Wahl et al. [14] used the SUL peak unit based on the lean body mass (total body weight minus the body fat weight ), Cronin et al. [15] in the other hand depended mainy in his study upon the visual assessment with taking hepatic FDG uptake as the reference standard.
Considerations about cost-effectiveness have not been part of this study but will be necessary, as they will play an increasing role in the near future as the clinical utility of PET/CT will lead to a change in the diagnostic and management strategy of cancer patients [16,17,18].
Conclusion
PET/CT is essential for assessment of treatment response of lytic and sclerotic bony lesions and can directly improve or refine the oncologic management plan.Further studies designed for comparison between PET/CT and whole body diffusion MRI is advised.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PET:
-
Positron emission tomography
- CT:
-
Computerized tomography
- SUV:
-
Standardized uptake value
- SUL:
-
Standardized uptake value corrected to lean body mas
- WB-DWI:
-
Whole body diffusion-weighted magnetic resonance imaging
References
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12:6243s–6249.
Tateishi U, Gamez C, Dawood S, Yeung HW, Cristofanilli M, Macapinlac HA (2008) Bone metastases in patients with metastatic breast cancer: morphologic and metabolic monitoring of response to systemic therapy with integrated PET/CT. Radiology 247:189–196
Von Schulthess GK, Steinert HC Hany TF(2006) Integrated PET/CT: Current applications and future directions. Radiology 238:405–422
Hoefeler H, Duran I, Hechmati G et al (2014) Health resource utilization associated with skeletal-related events in patients with bone metastases: results from a multinational retrospective—prospective observational study—a cohort from 4 European countries. J Bone Oncol 3:40–48
Abe K, Sasaki M, Kuwabara Y, Koga H, Baba S, Hayashi K et al (2005) Comparison of 18FDG-PET with 99mTc-HMDP scintigraphy for the detection of bone metastases in patients with breast cancer. Ann Nucl Med. 19:573–579
Yang HL, Liu T, Wang XM, Xu Y, Deng SM (2011) Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol 21:2604–2617
Du Y, Cullum I, Illidge TM, Ell PJ (2007) Fusion of metabolic function and morphology: sequential [18F]fluorodeoxyglucose positron-emission tomography/computed tomography studies yield new insights into the natural history of bone metastases in breast cancer. J Clin Oncol 25:3440–3447
Zidan D, Hasan M, Tantawy M (2013) Postoperative restaging: PET/CT impact on diagnosis and management. Egypt J Radiol Nuclear Med 44(2):321–329
Metser U, Goor O, Lerman H, Naparstek E, Even-Sapir E (2004) PET-CT of extranodal lymphoma. AJR 182:1579–1586
Blake GM, Park-Holohan SJ, Cook GJ, Fogelman I (2001) Quantitative studies of bone with the use of 18F-fluoride and 99mTc-methylene diphosphonate. Semin Nucl Med 31:28–49
Messiou C, Cook G, Reid AH et al (2011) The CT flare response of metastatic bone disease in prostate cancer. Acta Radiol 52(557–5):61
Padhani A, Gogbashian A (2011) Bony metastases: assessing response to therapy with whole-body diffusion MRI. Cancer Imaging. 11(1A):S129–S154
Cook G, Goh V (2018) Functional and Hybrid Imaging of Bone Metastases. J Bone Mineral Res 33(6):961–972
Wahl RL, Jacene H, Kasamon Y, Lodge MA(2009) From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 50:122S–150.
Cronin, C., Swords, R., Truong, M., Viswanathan, C., Rohren, E., Giles, F., O'Dwyer, M. and Bruzzi, J (2010) Clinical Utility of PET/CT in Lymphoma. Am J Roentgenol 194(1):W91-103.
Siegel RL, Miller KD, Jemal A (2017) Cancer Statistics. CA Cancer J Clin 67:7–30
Han A, Xue J, Zhu D, Zheng J, Yue J, Yu J (2011) Clinical value of (18)F-FDG PET/CT in postoperative monitoring for patients with colorectal carcinoma. Cancer Epidemiol 35:497–500
Cheson B (2018) PET/CT in lymphoma: current overview and future directions. Sem Nuclear Med 48(1):76–81
Acknowledgements
None.
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
MA reported the cases. WO reported the cases and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A written informed consent was obtained from all patients included in this study to publish this study data. Approval for this study was obtained from the Research Ethics Committee of our medical institute (IRB: 00012098) (FWA: 00018699). All study procedures were carried out in accordance with the Declaration of Helsinki regarding research involving human subjects.
Consent for publication
All the patients included in this study gave written informed consent to publish the data contained within this study.
Competing interests
There are no conflicts of interests. The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelmohsen, M.A., Omar, W.M. The added value of positron emission tomography/computed tomography (PET/CT) in assessment of treatment response of secondary malignant osseous lesions: our experience. Egypt J Radiol Nucl Med 51, 174 (2020). https://doi.org/10.1186/s43055-020-00292-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00292-1