Abstract
Background
Conventional brain MRI cannot always distinguish between different white matter lesions. Susceptibility weighted imaging (SWI) can detect a sign called central vein sign which is suggested to discriminate between multiple sclerosis and other white matter lesions thus increasing the accuracy of MRI in MS diagnosis. This study aimed to evaluate the role of MR susceptibility weighted imaging in differentiating MS from CSVD lesions.
Results
The central vein sign (CVS) was found to have a premium diagnostic performance in diagnosis of MS with sensitivity 83.3%, specificity 70%, positive predictive value 80.6%, and negative predictive value 73.7%. When CVS positive lesions load was ≥ 44.24%, the specificity of CVS in diagnosing MS raised to 100%.
Conclusion
Detection of the CVS on SWI can reliably discriminate between MS and CSVD.
Similar content being viewed by others
Background
Multiple sclerosis (MS) is defined as an inflammatory autoimmune neurodegenerative disease of the central nervous system, characterized by inflammation, demyelination, gliosis, and neuro-axonal loss in lesions [1].
MRI is a common investigation which can support a clinical diagnosis of MS by detecting lesions in the brain and spinal cord [2]. It can also be used for monitoring the disease activity which helps to guide treatment decision and to decrease relapse occurrence and disease progression [3, 4].
With advancing neuro-imaging, more atypical cases were experienced and because white matter lesions are depicted in many CNS diseases, specific diagnostic tools are needed [5].
Multiple MRI protocols were evolved to detect MS plaques and differentiating them from other similar lesions. Regarding the pathogenesis of MS lesions, they were found to be typically perivenular, so special MR sequences were used to detect the veins within the MS plaques [6], this feature is called the “central vein sign,” that would increase the accuracy of MRI in MS diagnosis [7].
Susceptibility-weighted imaging is one of the new MR sequences which can draw a venous map of the brain and can show the central vein in MS lesions [5].
Several recent studies using SWI in imaging of MS patients have revealed that SWI is more sensitive than conventional MR sequences (such as T2-weighted and FLAIR images) in detection of MS plaques and can demonstrate many signal patterns not previously seen within the MS plaques [8].
This study aimed to evaluate the role of MR susceptibility-weighted imaging in differentiating MS from CSVD lesions.
Methods
Informed written consents were obtained from the patients’ guardians according to the National Ethics Committee.
Patients
This prospective study included 50 patients who were classified into two groups: 30 patients (22 females and 8 males) were included in the first group, they were diagnosed clinically as MS, their ages ranged from 17 to 54 years. Patients with severe kidney disease or allergy to contrast medium, cardiovascular, cerebrovascular disease, or history of malignant disease were excluded. The second group included 20 patients (6 females and 14 males) with white matter lesions, possibly due to CSVD, their ages ranged from 36 to 70 years. Patients with prior brain stroke or history of malignant disease were excluded.
MRI imaging
All patients were examined by MRI 1.5 T system (GE SIGNA Explorer) with 16-channel head coil in supine position using a uniform protocol which includes axial T2-weighted and FLAIR sequences and SWI for detection of the CVS (Table 1).
If the referring physician suspects disease activity in MS patients, or if new lesion was detected, contrast enhanced T1-weighted sequence was done using gadolinium contrast medium with the dose (0.3 mmol/kg).
Image analysis
Two conjoint experienced neuroradiologists analyzed the data; they were totally blinded to patients’ clinical history. They analyzed FLAIR and T2W images for detection and localization of hyperintense white matter lesions then they classify the lesions according to their location into periventricular or non-periventricular and the non-periventricular lesions were then sub-classified into juxta-cortical, deep white matter, and infratentorial. Only the lesions which were 3 mm or more in size were included and confluent lesions were excluded.
In patients with CSVD, only patients who had lesions classified as Fazekas 0–2 (according to Fazekas scale [9, 10]) were included. Fazekas 0 lesion was defined as single punctate lesion, Fazekas 1 lesions represented multiple punctate lesions. Fazekas 2 lesions included some lesions that were beginning confluence. In this group of patients, confluent lesions were also excluded.
SWI images were analyzed for depiction of a central vein in the white matter lesions. The MinIP SWI images were utilized to better identify the signal void of a vein.
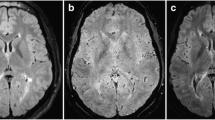
The central vein sign was defined according to the standard radiological definition established in the North American Imaging in Multiple Sclerosis (NAIMS) guidelines [11, 12] which recommend that: (Fig. 1)
- 1)
Lesions adopted a ‘coffee bean’ appearance with the vein appears as a thin hypointense central line (when the MRI slice was parallel to the vein long axis) or a ‘doughnut’ appearance with the vein appears as a small hypointense central dot (when the MRI slice was perpendicular to the vein).
- 2)
The vein runs partially or entirely through the lesion, but must be central in location regardless of the lesion’s shape.
- 3)
The vein is small in diameter (< 2 mm).
Magnified SWI images showing the morphology of the central vein sign according to vein direction. a Lesion with “coffee bean” appearance in which a thin hypointense line (representing the CVS) is seen running through the lesion and intersecting it. b Lesion with “doughnut” appearance, in which a hypointense central circular dot is noted and representing the CVS
When both evaluators were in agreement in detection of CVS, we defined the lesion as a CV positive lesion.
Exclusion criteria were also designed according to the standard radiological definition and included: lesion < 3 mm in diameter; confluent lesion; lesion with multiple distinct veins and lesion that is poorly visible (due to motion or other MRI artifacts).
Statistical analysis
Descriptive statistics were calculated for the two groups of patients, including mean/median, percentage, and range (minimum-maximum values). Then, the ratios between number of CVS positive lesions and total number of lesions for each patient were calculated, in both groups. The same ratios were also calculated for lesions according to their distribution (periventricular, non-periventricular). Mann-Whitney U test was used to compare variables between both groups which include total number of lesions, periventricular, non-periventricular. SPSS software package version 22.0 was used to analyze the data. A value of p < 0.05 was considered statistically significant.
Results
In this study, 50 patients were scanned: 30 of them were diagnosed clinically as MS, they included 22 females and 8 males with mean age 30.97 ± 9.79 years (range 17–54 years). The other 20 patients (including 6 females and 14 males with mean age 61.40 ± 10.34 years (range 36–70 years)) were known to have ischemic white matter lesions related to cerebral small-vessel disease. The difference in age and sex between the two groups of patients was significantly different (p < 0.001).
Regarding disease duration in MS group, 83.3% of MS patients suffered from the disease for < 5 years and 16.7% of patients for ≥ 5 years.
Based on the duration of MS disorder, the numbers of detected plaques for each patient were calculated in T2, FLAIR, and SWI sequences. It was found that the median numbers of detected plaques in patients with disease duration more than 5 years were 24 (18–31) in T2W sequences, 25 (18–33) in FLAIR sequences, and 25 (14–31) in SWI sequences. However, the median numbers of plaques in patients with disease duration less than 5 years were 12 (3–40), 13 (3–37), and 12 (3–38) in T2W, FLAIR, and SWI sequences, respectively. All MRI sequences used in this study showed significantly higher numbers of plaques in patients with disease duration more than 5 years than patients with disease duration less than 5 years (p = 0.01).
In MS patients, 453 lesions were detected, while 144 lesions were detected in patients with CSVD. Regarding lesion distribution, in MS patients, 181 (39.95%) lesions were detected in the periventricular region, (Figs. 2 and 5) while 272 (60%) lesions were detected in non-periventricular location and then classified as (93 (34.1%) juxta-cortical, 159 (58.5%) deep white matter, and 20 (7.4%) infratentorial). In CSVD patients, 43 (29.9%) lesions were detected in the periventricular region while 101 (70.1%) lesions were detected in non-periventricular location and then classified as (30 (29.7%) juxta-cortical, 64 (63.4%) deep white matter, and 7 (6.9%) cerebellar) (Table 2).
Axial (a, c e) T2WI images show hyperintense MS periventricular (black arrows), deep white matter (arrowhead), and juxta-cortical lesions (white arrow). On corresponding (b, d f) SWI images, a thin hypointense line representing the CVS is seen within the periventricular (black arrows), deep white matter (arrowhead), and juxta-cortical lesions (white arrow) while a central hypointense dot in the right periventricular lesion (red arrow)
By analyzing the proportion of CVS-positive lesions in each patient, we found that the number of MS patients presented with CVS-positive lesions (29 patients with the proportion of CVS positive lesions in each patient ranging from 0 to 100%, median 48%) was significantly higher than CSVD patients (14 patients with the proportion of CVS positive lesions in each patient ranging from 0 to 44%, median 25%) (Fig. 3). This was statistically significant (p = 0.007).
A total of 223 out of 453 MS lesions (49.22%) have demonstrated the CVS, most of them (124/223, 55.6%) seen in the periventricular region, while only 37 out of 144 CSVD lesions (25.69%) were CVS-positive with (15/37, 40.5%) lesions had a periventricular distribution. This was statistically significant with (p value < 0.001) (Table 3).
As regards the location of the CVS positive lesions, there was a statistically significant difference between the MS and CSVD patients in both periventricular and non-periventricular location (with the p value = 0.004 and 0.007, respectively) as shown in Fig. 4. In MS patients, 68.5% (124/181) of periventricular lesions and 36.39% (99/272) of non-periventricular lesions were positive for CVS (Figs. 2 and 5), while in CSVD group, only 34.88% (15/43) of periventricular lesions and 21.78% (22/101) of non-periventricular were positive for CVS (Figs. 6 and 7).
Axial (a) T2WI image shows hyperintense MS periventricular and juxta-cortical lesions (arrow and arrowhead). On the corresponding SWI (b) and amplified SWI images (c and d), a thin hypointense line and a central hypointense dot (representing the CVS) are seen in the juxta-cortical (arrow head) and periventricular lesions (arrow), respectively
A 60-year-old male patient with cerebral small vessel disease. Axial (a and c) T2WI images show multiple hyperintense periventricular (black arrows), deep white matter (arrow head), and juxta-cortical lesions (white arrow). On corresponding (b and d) SWI images, a thin hypointense line representing the CVS is seen in the periventricular (black arrows), deep white matter (arrow head), and juxta-cortical lesions (white arrow)
A 63-year-old female patient with cerebral small vessel disease. Axial (a) T2WI image show multiple hyperintense periventricular (black arrows) and juxta-cortical lesions (white arrow). On corresponding (b) SWI image, a thin hypointense line representing the CVS is seen in the periventricular (black arrows) and juxta-cortical lesions (white arrow)
The CVS was found to have a premium diagnostic performance in diagnosis of MS with the sensitivity 83.3%, specificity 70%, positive predictive value 80.6%, and negative predictive value 73.7% (Table 4). When CVS positive lesions load was 44.24% and above, the specificity of CVS in diagnosing MS raised to 100% (Fig. 8).
Discussion
White matter lesions are usually depicted on brain MRI done for various indications. The majority of them caused by microangiopathy, but multiple sclerosis, is also considered an important cause. Conventional MRI cannot accurately differentiate between these pathologies. SWI can detect the central vein sign which has been suggested to discriminate between MS and other white matter lesions as microangiopathic brain lesions [13].
This study revealed that central vein sign positive lesions were much more in MS (49.22%) than in CSVD (25.69%) with statistically significant difference (p < 0.001). This is in agreement with a study done by Sparacia et al. [14], in which 40.9% of MS lesions versus 29.3% of CSVD lesions have demonstrated the central vein sign. This difference explains the different pathogenesis of both diseases.
It was also found that the proportion of CVS-positive lesions in patients with MS (median 48%, range 0–100%) was consistently much higher than in subjects with CSVD (mean 25%, range 0–44%). This copes with Tallantyre et al. study [15] which revealed higher proportion of perivenous lesions in patients with MS (mean 80%, range 53–100%) than in patients without MS (mean 16%, range 0–34%).
In this study, periventricular location of the central vein sign was more obvious in MS lesions (55.6%) than in CSVD lesions (40.5%). This matches with previous studies done by Sparacia et al. [14], Lane et al. [16], Kau et al. [17], and Al-Zandi et al. [5]. This observation reflects the fact that MS inflammation begins around small cerebral veins, as discovered by pathology [11, 18].
This study also revealed that the CVS is a significant discriminator (p < 0.001) between MS-WMLs and CSVD-WMLs with a sensitivity 83.3%, specificity 70%, positive predictive value 80.6%, and negative predictive value 73.7%. The CVS was also found to have a premium diagnostic efficacy in MS diagnosis with a specificity reaching 100% when the load of CVS positive lesions is ≥ 44.24%. This finding is in agreement with the results of Al-Zandi et al. study [5] in which the specificity for predicting the diagnosis of MS reached 100% when the load of CVS positive lesions was ≥ 47.5%. Also the sensitivity, specificity, positive, and negative predictive values of the CVS in MS diagnosis were 86.84%, 86.6%, 88.7%, and 75.72%, respectively. Yet, with regard to the specificity of the CVS, our results did not cope with a study done by Lummel et al. [19] which revealed that the central vein sign is a non-specific finding for MS. A probable explication for this result is that they used a different technique (susceptibility-weighted imaging angiography), that differs from SWI applied in our study.
The limitations of this study can be summarized in three main factors: first, the relatively low field strength (1.5 T) compared to other studies done using field strength 3 T and 7 T. Second, although we carried out a lesion based analysis in a reasonable number of WMLs, both MS and CSVD groups were small. Eventually, the significant difference in age between the two groups of patients that reflects the different age of affection in MS and CSVD.
Conclusion
Finally, it was concluded that SWI sequence improves the diagnostic accuracy of MS through detection of the CVS which considered as a fairly reliable discriminator between MS-WMLs and CSVD-WMLs especially when CVS positive lesion load is ≥ 44.24% of the total lesions.
Availability of data and materials
Available on request with the corresponding author.
Abbreviations
- CSVD:
-
Cerebral small vessel disease
- CVS:
-
Central vein sign
- MRI:
-
Magnetic resonance imaging
- MS:
-
Multiple sclerosis
- SWI:
-
Susceptibility weighted imaging
- WMLs:
-
White matter lesions
References
Sheng H, Zhao B, Ge Y (2019) Blood perfusion and cellular microstructural changes associated with iron deposition in multiple sclerosis lesions. Frontiers in neurology, 10, 747. https://doi.org/10.3389/fneur.2019.00747.
Filippi M, Rocca MA, Ciccarelli O, De Stefano N, Evangelou N, Kappos L et al (2016) MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurology 15(3):292–303 https://doi.org/10.1016/S1474-4422(15)00393-2
Miller DH (2004) Biomarkers and surrogate outcomes in neurodegenerative disease: lessons from multiple sclerosis. NeuroRx 1(2):284–294 https://doi.org/10.1602/neurorx.1.2.284
Giovannoni G, Butzkueven H, Dhib-Jalbut S, Hobart J, Kobelt G, Pepper G et al (2016) Brain health: time matters in multiple sclerosis. Multiple sclerosis and related disorders 9:S5–S48 https://doi.org/10.1016/j.msard.2016.07.003
Al-Zandi SH, Fayadh NA, Al-Waely NK (2018) Central vein sign detected by SWI at 3 T MRI as a discriminator between multiple sclerosis and leukoaraiosis. The Egyptian Journal of Radiology and Nuclear Medicine 49(1):158–164 https://doi.org/10.1016/j.ejrnm.2017.09.003
Absinta M, Sati P, Gaitán MI, Maggi P, Cortese IC, Filippi M et al (2013) Seven-tesla phase imaging of acute multiple sclerosis lesions: A new window into the inflammatory process. Annals of neurology 74(5):669–678 https://doi.org/10.1002/ana.23959
Sati P, Thomasson DM, Li N, Pham DL, Biassou NM, Reich DS et al (2014) Rapid, high-resolution, whole-brain, susceptibility-based MRI of multiple sclerosis. Multiple Sclerosis Journal 20(11):1464–1470 https://doi.org/10.1177/1352458514525868
Miller C, Goldberg MF (2012) Susceptibility-weighted imaging and computed tomography perfusion abnormalities in diagnosis of classic migraine. Emergency radiology 19(6):565–569. https://doi.org/10.1007/s10140-012-1051-2 Epub 2012 Jun 9
Fazekas G, Fazekas F, Schmidt R, Kapeller P, Offenbacher H, Krejs GJ (1995) Brain MRI findings and cognitive impairment in patients undergoing chronic hemodialysis treatment. Journal of the neurological sciences 134(1):83–88 https://doi.org/10.1016/0022-510X(95)00226-7
Forbes K (2017) MRI brain white matter change: spectrum of change–how can we grade? JOURNAL OF THE ROYAL COLLEGE OF PHYSICIANS OF EDINBURGH 47(3):271. https://doi.org/10.4997/JRCPE.2017.313
Sati P, Oh J, Constable RT, Evangelou N, Guttmann CR, Henry RG et al (2016) The central vein sign and its clinical evaluation for the diagnosis of multiple sclerosis: a consensus statement from the North American Imaging in Multiple Sclerosis Cooperative. Nature Reviews Neurology 12(12):714. https://doi.org/10.1038/nrneurol.2016.166 Epub 2016 Nov 11
Mistry N, Abdel-Fahim R, Samaraweera A, Mougin O, Tallantyre E, Tench C et al (2016) Imaging central veins in brain lesions with 3-T T2*-weighted magnetic resonance imaging differentiates multiple sclerosis from microangiopathic brain lesions. Multiple Sclerosis Journal 22(10):1289–1296 https://doi.org/10.1177/1352458515616700
Geraldes R, Ciccarelli O, Barkhof F, De Stefano N, Enzinger C, Filippi M et al (2018) The current role of MRI in differentiating multiple sclerosis from its imaging mimics. Nature Reviews Neurology 14(4):199 https://doi.org/10.1038/nrneurol.2018.14
Sparacia G, Agnello F, Gambino A, Sciortino M, Midiri M (2018) Multiple sclerosis: High prevalence of the ‘central vein’sign in white matter lesions on susceptibility-weighted images. The neuroradiology journal 31(4):356–361 https://doi.org/10.1177/1971400918763577
Tallantyre EC, Dixon JE, Donaldson I, Owens T, Morgan PS, Morris PG et al (2011) Ultra-high-field imaging distinguishes MS lesions from asymptomatic white matter lesions. Neurology, 76(6), 534-539. https://doi.org/10.1212/WNL.0b013e31820b7630.
Lane JI, Bolster B, Campeau NG, Welker KM, Gilbertson JR (2015) Characterization of multiple sclerosis plaques using susceptibility-weighted imaging at 1.5 T: can perivenular localization improve specificity of imaging criteria? Journal of computer assisted tomography 39(3):317–320. https://doi.org/10.1097/RCT.0000000000000233
Kau T, Taschwer M, Deutschmann H, Schönfelder M, Weber JR, Hausegger KA (2013) The “central vein sign”: is there a place for susceptibility weighted imaging in possible multiple sclerosis? European radiology 23(7):1956–1962. https://doi.org/10.1007/s00330-013-2791-4 Epub 2013 Feb 22
Adams CWM, Poston RN, Buk SJ (1989) Pathology, histochemistry and immunocytochemistry of lesions in acute multiple sclerosis. Journal of the neurological sciences 92(2-3):291–306 https://doi.org/10.1016/0022-510X(89)90144-5
Lummel N, Boeckh-Behrens T, Schoepf V, Burke M, Brückmann H, Linn J (2011) Presence of a central vein within white matter lesions on susceptibility weighted imaging: a specific finding for multiple sclerosis? Neuroradiology 53(5):311–317 https://doi.org/10.1007/s00234-010-0736-z
Acknowledgements
Not applicable.
Funding
Not applicable (no funding received for this study).
Author information
Authors and Affiliations
Contributions
SE and RA designed the research. RA performed the research; and wrote the manuscript. SE and ME analyzed the collected data. SE, TB, and ME revised data and manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of the Radiology Department of the Faculty of Medicine, Mansoura University, on 8/7/2017, reference number of approval: MD/17.06.94.
All patients included in this study gave a written informed consent to participate in the research.
Consent for publication
All patients included in this study gave a written informed consent to publish the data contained in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anan, R.A., El-Adalany, M.A., Belal, T.M.I. et al. Detection of central veins using susceptibility weighted imaging (SWI) for discrimination between lesions in multiple sclerosis (MS) and cerebral small vessel disease (CSVD). Egypt J Radiol Nucl Med 51, 63 (2020). https://doi.org/10.1186/s43055-020-00185-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00185-3