Abstract
Background
Pediatric ureteral injuries can arise from trauma or surgical procedures, and urinary-enteral fistulas, although rare, are both challenging to manage and repair. More information is needed regarding ureteral-enteral fistulas in the general population, and successful treatment options are limited. This case report introduces an innovative approach, treatment, and successful follow-up featuring a novel repair technique designed for pediatric patients.
Case presentation
As a result of complicated appendicitis, a 2-year-old male developed a uretero-enteral fistula. A right ureteral-enteral fistula was detected, and because of the persistent metabolic acidosis and deteriorating malnourishment, a percutaneous nephrostomy tube was inserted with the closure of the fistula through a colonoscopy clip. Three months later, with a better patient’s condition, corrective ureteral surgery was performed with total resection of the fistulized ileocolonic segment (an anastomosis previously made because of the ileocecal valve resection secondary to appendiceal process) and total reconstruction of the urinary tract using a Boari vesical flap. The postoperative course was satisfactory.
Conclusion
Managing the ureteral-enteral fistulas is a surgical challenge due to their diverse etiology and presentation. An effective surgical management plan requires a comprehensive understanding of ureteral injuries and associated conditions and an examination of the patient's urological anatomy and function to tailor the best treatment for each case.
Similar content being viewed by others
Background
Pediatric ureteral injuries most commonly can occur because of penetrating or blunt trauma but also can be due to surgical interventions. Ureteral injuries can be classified by location, the injury's onset, and the extent of damage (Table 1). The overall incidence of iatrogenic ureteral trauma shifts depending on the type of surgery approach [1,2,3]. Urinary enteral fistulas are uncommon anomalies and can be associated with ureteral trauma; they are difficult to approach due to their diverse etiology.
The symptoms and clinical findings are often non-specific and variable, making establishing a clear suspicion of the condition challenging [5, 6]. The diagnosis can be successfully achieved by contrast-based imaging or endoscopy [7]. The management of the condition is guided by the patient’s clinical status, comorbidities, and nutritional state, with options ranging from observation to surgical reparation [8].
Currently, there are limited descriptions in the general population about ureteral enteral fistulas and ureteral injury together. The treatment success rates are relatively scarce. This prompts us to present the following case, which includes its innovative approach, treatment, and successful follow-up, utilizing a novel repair technique specifically designed for pediatric patients.
Case presentation
Because of complicated appendicitis, a 2-year-old male with a right ureteral-enteral fistula and ureteral injury received treatment at our tertiary care center. The patient underwent laparoscopic appendectomy, followed by three subsequent laparotomies due to recurrent intestinal perforations and drainage of collections. These interventions comprised: 1) primary closure of the colon with cavity irrigation, 2) closure of perforations at 10 and 45 cm from the ileocecal valve, along with the establishment of an ileostomy, and 3) resection of the cecum and terminal ileum with ileocolonic anastomosis, followed by a redo of Double-barreled ileostomy.
The patient continued to experience chronic diarrhea and, despite active management, developed malnutrition and persistent metabolic acidosis with a pH of 7.25, HCO3 of 13.2, and a base excess of -14.2. To address this, we initiated the administration of sodium bicarbonate through infusion at a rate of 3 mEq/kg/day to improve the acid–base balance. A right ureteral-enteral fistula was detected with urinary output through the distal stoma, probably resulting from an unadvertised injury of the right ureter during one of the last surgeries that explains chronic diarrhea, metabolic acidosis, and the urinary output through the stoma. Therefore, the patient was ultimately referred to our hospital for advanced treatment. The diagnosis was confirmed through excretory urography (Fig. 1). During cystoscopy and ascending pyelography as part of the diagnostic approach, it was impossible to pass a hydrophilic guidewire and contrast into the ipsilateral ureter through the right meatus, revealing an amputated ureter at the junction of the distal and middle portions.
A percutaneous nephrostomy tube was inserted to reduce the flow through the fistula. However, due to persistent metabolic acidosis and worsening malnutrition, we decided to perform a diagnostic colonoscopy. During the procedure, methylene blue was infused through the nephrostomy tube to identify the fistula site, which was found to be 45 cm from the anal margin. We successfully placed an endoscopic clip at this location (Fig. 2). As a result, there was a significant reduction in fistula output, leading to a decreased need for sodium bicarbonate supplementation.
Ureteral-enteral fistula and its closure. (A) The ureteral-enteral fistula was observed through descending pyelography via nephrostomy (arrow). (B) Uretero-enteral fistula located via endoscopy with methylene blue instillation through nephrostomy (arrow). (C) Fluoroscopic confirmation of the endoscopic clip placement at the site of the fistula (arrow)
We implemented ambulatory care and provided coordinated nutritional support to enhance the patient's nutritional status, preparing for corrective surgery under improved conditions.
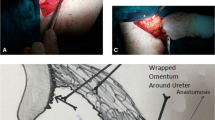
Three months later, treatment surgery was performed, including ileostomy closure by end-to-end anastomosis, total resection of the fistulized ileocolonic segment with end-to-end ileocolonic anastomosis, and total reconstruction of the urinary tract using a Boari vesical flap with proximal anastomosis to the renal pelvis. The proximal ureteral stump was excluded from the procedure, as it necessitated resection during dissection due to intimate adherence to the fistula site. Additionally, a trans anastomotic double-J stent was carefully positioned (Fig. 3).
Urinary reconstruction with a 'Boari' vesical flap technique. Through a Gibson-type approach and after the total resection of the fistula to the ileocolonic anastomosis site, A Length measurement from the bladder to the ureteral stump (or renal pelvis, in this case (*)), and the same distance is measured on the bladder dome (arrow). B The incision in the bladder dome to take the pre-measured flap. C Completed ureteral reconstruction
During the postoperative period, we proceeded satisfactorily. For the following five days, the patient was managed with fasting and an open nephrostomy, after which the patient was discharged for outpatient care with the nephrostomy closed. We removed the double-J catheter four weeks later and conducted an antegrade pyelography during the same session to confirm proper contrast flow to the bladder. Consequently, we decided to remove the nephrostomy tube. After three months, we excluded the obstruction and confirmed satisfactory flow through MAG 3 scintigraphy, indicating a split function of 35.4% for the right kidney. Due to the bladder surgery, we performed a voiding cystourethrogram, revealing adequate bladder capacity with ureteral reflux (grade III) and clearance of the renal pelvis at the time of voiding (Figs. 4 and 5).
Discussion
The incidence of ureteral injuries is generally low, with only a few cases reported in the literature [4, 8, 9]. Uretero-digestive fistulas are uncommon and typically associated with urinary surgery or endourologic procedures [10, 11] or resulting from trauma. During laparoscopic surgery, ureteral injuries often go unnoticed, resulting in insidious symptoms and delayed treatment [12]. They are also related to recurrent infection, chronic inflammation, and, in some cases, malignancies [13,14,15].
Ureteral involvement can lead to a range of comorbidities, including stenosis, fistulas, hydronephrosis, chronic pain, recurrent infections, and loss of renal function [16]. Clinical presentations often emphasize the potential for cross-contamination of colonic and urinary tract contents, which can lead to electrolyte abnormalities, diarrhea, recurrent urinary tract infections, pneumaturia, and, in some cases, fecaluria. Digestive symptoms and flank pain are reported less frequently, ultimately contributing to malnourishment. Metabolic acidosis resulting from electrolyte imbalance can be life-threatening in pediatric patients, requiring an urgent repair of the urinary connection to the digestive tract [17].
Postoperative fistulas result in increased morbidity and a more extended hospital stay. Treatment options for these conditions may include nephrostomy tube placement, ureteral stenting, intestinal resection, and urinary tract reconstruction [18]. While surgery is the most common treatment, the endoscopic approach is an increasingly utilized alternative, predominantly in adult patients and often involving stent placement instead of clipping [19].
The approach to urinary tract reconstruction depends on the location and length of the injury. Minor defects can be effectively addressed through endoscopic procedures, such as temporarily placing a ureteral stent for a few weeks. Additionally, a technique involving endoscopic realignment, combining antegrade and retrograde ureteroscopy, is applicable in cases of wholly transected ureters [20]. However, for injuries resulting in longer strictures, these minimally invasive approaches exhibit limited long-term success rates [21].
In open approaches for tuberculous stricture, urogenital malignancy, and strictures post-pelvic surgery, radiation, or trauma, various attempts have been made to utilize different bowel segments, such as ileal, colonic, or appendiceal segments, for open ureteral reconstructions [22, 23]. These segments are opened anti-mesenterically and reconfigured after rotation, resembling the Yang-Monti procedure [24]. However, severe postoperative complications, including metabolic acidosis secondary to renal failure, stenosis, and fistulas, have been reported after bowel interposition [25].
Full-length ureteral defects can also be reconstructed using only the urinary bladder. One method involves creating a spiral bladder muscle flap while preserving branches of the superior vesical artery. This flap demarcated slightly longer than the ureteral defect, is spirally wrapped around a stent and anastomosed to the proximal end of the ureter. Other successful operative techniques include ureteroureterostomy, ureter cystostomy with psoas hitch, and Boari flap [25,26,27].
Another proven technique involves injecting indocyanine green into the stricture ureter via nephrostomy and ureteral catheter. Visualization of indocyanine green with near-infrared fluorescence allows for the clear identification of the ureter, stricture length, and localization [28]. The most successful outcomes are observed when these techniques are combined and tailored to individual cases, and all the methods are now used in laparoscopic and robot-assisted approaches [11, 29].
Distal injuries are often successfully managed with vesicoureteral reimplantation only or psoas hitch procedure. In cases of long ureteral loss, procedures like Boari vesical flap reconstruction can achieve success rates exceeding 80% [30] (Fig. 5).
This case highlights the patient's improved condition, achieved through the successful closure of the ureterocolonic fistula using an endoscopic clip with a nephrostomy. This approach allowed for the planning of subsequent fistula resection and ureteral reconstruction with a vesical flap. The follow-up confirmed patency from the bladder to the renal pelvis during a retrograde cystogram.
Conclusion
Ureteral-enteral fistulas pose a surgical challenge due to their diverse etiology and presentation. An effective surgical management plan necessitates a comprehensive understanding of ureteral injuries and their associated conditions and a thorough examination of the patient's urological anatomy and function to tailor the best treatment for each case.
Availability of data and materials
The data and materials used in this study are available upon request. Due to restrictions on sharing the data publicly, a direct link to the dataset cannot be provided. However, all relevant data and materials necessary to replicate the study's findings will be made available to the corresponding author upon reasonable request.
References
Bryk DJ, Zhao LC (2016) Guideline of guidelines: a review of urological trauma guidelines. BJU Int 117(2):226–234
Singer G, Arneitz C, Tschauner S, Castellani C, Till H (2021) Trauma in pediatric urology. Semin Pediatr Surg 30(4):151085
Gearhart JP, Rink RC, Mouriquand PDE. Pediatric Urology (2nd ed). Saunders/Elsevier. 2010.
Engelsgjerd JS, LaGrange CA. Ureteral injury. In. StatPearls. 2022. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK507817/
Flood HD, Jones B, Grainger R (1992) Ureterocolic fistula: a unique complication of extracorporeal shock wave lithotripsy. J Urol 147(1):122–124
Mozo M, Gonzálo R, Gutiérrez JM, Gutiérrez LE, Cotruta L, Roca A, García R (2018) Colorenal fistula after renal tumor cryotherapy. Int J Surg Case Rep 53:441–443
Heney NM, Crooks KK (1984) Ureterocolic fistula. Br J Urol 56:225–226
Hillman E, Fu H, Anele U (2023) Colo-renal fistula in a patient with refractory anemia and recurrent urinary tract infections: a case report and review of the literature. Cureus 15(9):e44741. https://doi.org/10.7759/cureus.44741
Dalecki J, Patel R, Sundararajan L (2010) Ureteral damage during appendicectomy. J Pediatr Surg 45(11):e11–e13
Selzman AA, Spirnak JP (1996) Iatrogenic ureteral injuries: a 20-year experience in treating 165 injuries. J Urol 155(3):878–881
Stühler V, Bedke J, Stenzl A (2019) Rekonstruktionsmöglichkeiten des Harnleiters. Urologe 58(6):651–657
Ding G, Li X, Fang D, Hao H, Li X, Zhou L (2021) Etiology and ureteral reconstruction strategy for iatrogenic ureteral injuries: a retrospective single-center experience. Urol Int 105(5–6):470–476
Zeller FL, García Garzón JM, Peralta J (2013) Asymptomatic renocolic fistula as a complication of staghorn calculus: case report. Arch Esp Urol 66:817–819
Bensouda A, El Hader K, Sbihi L, Benkabbou A, Karmouni T, Tazi K et al (2010) Entero-urinary fistula. Tunisian Med J 88(11):814–819
Murakami K, Tomita M, Kawamura N, Hasegawa M, Nabeshima K, Hiki Y et al (2007) Severe metabolic acidosis and hypokalemia in a patient with enterovesical fistula. Clin Exp Nephrol 11(3):225–229
Parpala-Spårman T, Paananen I, Santala M, Ohtonen P, Hellström P (2008) Increasing numbers of ureteric injuries after the introduction of laparoscopic surgery. Scand J Urol Nephrol 42(5):422–427
Gill HS (2016) Diagnosis and surgical management of uroenteric fistula. Surg Clin North Am 96(3):583–592
Burks FN, Santucci RA (2014) Management of iatrogenic ureteral injury. Ther Adv Urol 6(3):115–124
Díaz Ruiz R, Castillo Pradillo M, Nogales Rincón Ó, González Asanza C (2017) Enteral stent for the treatment of a urinary fistula associated with a biological mesh following a Bricker-type procedure. Rev Esp Enferm Dig 109(4):286–287
Siegel J, Simhan J, Tausch TJ, Morey AF (2014) Ureteral strictures and reconstruction in the cancer survivor. Curr Opin Urol 24(4):421–426
Liu C, Zhang X, Xue D et al (2014) Endoscopic realignment in the management of complete transected ureter. Int Urol Nephrol 46(2):335–340
Takeuchi M, Masumori N, Tsukamoto T (2014) Ureteral reconstruction with bowel segments: experience with eight patients in a single institute. Korean J Urol 55(11):742–749
Chen CL, Tang SH, Cha TL et al (2014) Combined Y-shaped common channel transureteroureterostomy with Boari flap to treat bilateral long-segment ureteral strictures. BMC Res Notes 7:550
Li Y, Li C, Yang S et al (2014) Reconstructing full-length ureteral defects using a spiral bladder muscle flap with vascular pedicles. Urology 83(5):1199–1204
Ordorica R, Wiegand LR, Webster JC, Lockhart JL (2014) Ureteral replacement and onlay repair with reconfigured intestinal segments. J Urol 191(5):1301–1306
Do M, Kallidonis P, Qazi H et al (2014) Robot-assisted technique for Boari flap ureteral reimplantation: Is robot assistance beneficial? J Endourol 28(6):679–685
Engel O, Rink M, Fisch M (2015) Management of iatrogenic ureteral injury and techniques for ureteral reconstruction. Curr Opin Urol 25(4):331–335
Lee Z, Moore B, Giusto L, Eun DD (2014) Use of indocyanine green during robot-assisted ureteral reconstructions. Eur Urol 67(2):291–298
Zhong W, Du Y, Yang K, Meng S, Lin R, Li X et al (2017) Ileal ureter replacement combined with Boari flap-psoas hitch to treat full-length ureteral defects: technique and initial experience. Urology 108:201–206
Wenske S, Olsson CA, Benson MC (2013) Outcomes of distal ureteral reconstruction through reimplantation with psoas hitch, boari flap, or ureteroneocystostomy for benign or malignant ureteral obstruction or injury. Urology 82(1):231–236
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JGC was responsible for data collection, management, sequence alignment, and initial manuscript drafting. PJU contributed to the clinical aspects of the study and provided patient treatment. EMC participated in patient treatment, sequence alignment, and manuscript drafting. SB contributed to the study design, performed statistical analysis, and provided critical input. JGC and SB contributed to the study design, coordination, and manuscript drafting. All authors have read and approved the final manuscript. JGC illustrator of Fig. 5.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article presents a case report involving a pediatric patient with a ureteocolonic fistula and its management. The study complied with the ethical principles outlined in the Declaration of Helsinki. Written informed consent was obtained from the patient's parents or legal guardians to publish their cases and accompanying images. The need for ethics approval was waived by the Hospital Inner Committee, as per their guidelines. The confidentiality of patient information was strictly maintained, and all data were de-identified before analysis. This study adheres to the ethical standards of our institution and ensures the privacy and rights of the patients involved."
Consent for publication
Written informed consent was obtained from the patient's parents or legal guardians to publish their cases and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chavez, J.L.G., Urueta, P.S.J., Camacho, E.M. et al. Management of uretero-colonic fistulas and ureteral injuries: a comprehensive surgical and endoscopic approach. Egypt Pediatric Association Gaz 72, 40 (2024). https://doi.org/10.1186/s43054-024-00280-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00280-4