Abstract
Background
Neonatal intestinal obstruction is a complex condition that poses challenge in management. Prompt recognition and appropriate management are crucial to prevent complications. We present a case of a term neonate with intermittent bilious vomiting.
Case presentation
The baby underwent routinely performed investigations, including abdominal radiography and ultrasound, which provided inconclusive results. However, contrast-enhanced computed tomography revealed a web at duodenojejunal flexure. Exploratory laparotomy confirmed the diagnosis, and surgical intervention was performed. The baby’s postoperative course was prolonged with a gradual transition from parenteral nutrition to enteral feeds.
Conclusion
This case highlights a rare cause of intestinal obstruction, the unusual location of duodenal web, the importance of maintaining a high index of suspicion for intestinal obstruction, even in the absence of classical signs, and the value of utilizing contrast-enhanced computed tomography when initial investigations are inconclusive.
Similar content being viewed by others
Background
Intestinal obstruction is a common cause of admission to neonatal intensive care unit. The varied aetiology and clinical presentation in these cases often poses a diagnostic and therapeutic challenge. These infants may also experience a prolonged postoperative period due to various complications. Prompt diagnosis and timely surgical intervention are essential to prevent further complications. The estimated reported incidence of neonatal intestinal obstruction is 1 in 2000 live birth [1]. Though clinical presentations in neonatal intestinal obstruction are diverse, presence of maternal polyhydramnios, bilious emesis, failure to pass meconium and abdominal distension are some of the cardinal clinical signs of neonatal intestinal obstruction [2]. Clinical history and examination coupled with imaging is often helpful in arriving at a diagnosis. An abdominal radiograph remains the first investigation in these cases. The abdominal gas pattern is distinctive and can aid in localising the site of obstruction in several cases. However, the typical gas pattern may not be observed, and the radiograph remains inconclusive. Thus, a high index of suspicion for obstruction and the use of other imaging modalities might help in an earlier diagnosis. Delay in the diagnosis and surgical intervention may result in loss of a significant portion of bowel and associated complications [1]. The present case shows a rare cause and location of intestinal obstruction in a term neonate who presented with intermittent bilious emesis without other cardinal signs of intestinal obstruction.
Case presentation
A singleton girl baby was delivered at a gestational age of 39 completed weeks through lower segment caesarean section due to non-progression of labor. The baby weighed 2780 g and did not require any resuscitation after birth. Mother was 35 years, primigravida and had regular antenatal visits. Prenatal ultrasonography done at 20 weeks and 34 weeks were reported normal. There was no obvious external congenital anomalies. The baby was nursed by the mother and breast feeding initiated.
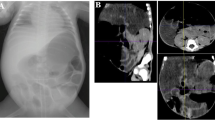
At 6 h of life, the baby presented with multiple bilious vomiting and was admitted to intensive care. On examination, there was no obvious external congenital malformation with patent anal opening and no abdominal distension. Differentials of upper gastrointestinal obstruction and sepsis were kept. Intravenous fluids started after admission, orogastric tube was inserted and kept on continuous drainage. Empirical antibiotics started after sending blood culture. Abdominal radiograph performed at 16 h of life suggested paucity of colonic and rectal gas but there was no specific pattern (Fig. 1). Abdominal ultrasound revealed dilation of stomach and duodenum with normal orientation of superior mesenteric vessels. Complete blood counts were normal, C-reactive protein was 0.9 mg/dl. There was no significant drainage through orogastric tube for 24 h. The baby also passed meconium within 24 h of life and thereafter. The case was discussed with paediatric surgeon and a decision to initiate feeds through orogastric tube was taken. While advancing feeds, there was recurrence of bilious vomiting on day 6. A repeat abdominal radiograph findings was non-specific and inconclusive. After discussing with radiologist, a contrast enhanced computed tomography (CECT) of abdomen was performed on day 8, which revealed a web at the duodenojejunal flexure (Fig. 2). Exploratory laparotomy was performed on day 10. Abdomen was approached via a right supraumbilical transverse incision. Intraoperative findings revealed a transition zone at the duodenojejunal junction with a dilated proximal bowel loop (Fig. 3). Resection of the web and duodenojejunal anastomosis (classical diamond anastomosis) was performed, trans-anstomotic naso-jejunal tube was placed. The baby was started on total parenteral nutrition in postoperative period. She continued to have bilious aspirate through orogastric drainage, gradually reducing by 7th postoperative day. Enteral feeds were commenced through the naso-jejunal trans-anastomotic tube. As the baby tolerated feeds, volume of feeds were escalated over the next four days and parenteral nutrition discontinued. Later, by day 14th postoperative day, baby was accepting direct breast feeds. She was discharged on day 24 of life and weighing 2630 g at time of discharge.
Discussion
The present case shows congenital duodenal web as a cause of intestinal obstruction in a term neonate. The neonate presented with intermittent bilious emesis and there was no significant abdominal distension at time of admission. Baby also passed meconium regularly. The bilious emesis was negligible while the baby was nil per oral and was more pronounced while baby was on feeds.
Gastrointestinal webs are not a very common cause of intestinal obstruction in neonates. Although it can occur anywhere along the gastrointestinal tract, the small intestine and stomach are the most common site of occurrence. Some authors consider intestinal webs, including duodenal, jejunal, and ileal webs, to be a type of intestinal atresia [3, 4]. The second portion of the duodenum is the most frequent site of intestinal webs (85–90% cases) followed by third and fourth part of duodenum [3, 5, 6]. Congenital duodenal web refers to complete or partial luminal blockage in the duodenum and arises from a membranous web or intraluminal diverticulum. Structurally, the web consists of mucosa and submucosa and lacks muscular layer [7]. Typically, a small opening is present at the centre of the duodenal web, which differentiates it from duodenal atresia. Although there is limited epidemiological information available regarding duodenal webs, they are believed to be less common, with an estimated incidence ranging from 1 in 10,000 to 1 in 40,000 [8].
A study spanning 32 years and examining 138 neonatal cases of duodenal obstruction revealed that vomiting was the most common symptom which was present in 90% of cases, and bilious vomiting in 66% of cases. Abdominal distension (25%), dehydration (24%), and weight loss (17%) were the other reported signs and symptoms [9]. More than half (56%) of the neonates developed symptoms within 24 h of birth. Plain abdominal roentgenograms were diagnostic in 58% of cases [9]. In our case although the baby exhibited repeated instances of bilious vomiting, abdominal radiographs reports were unremarkable. Sarin YK et al. have reported 18 cases of duodenal web and found that the average age of the presentation was around 8 days, with bilious vomiting being the most frequent symptom [7]. But, the classical radiographic signs of small intestinal atresia was not evident in all cases, similar to the index case. In another case series, the authors have discussed 12 cases of congenital duodenal web and noted that the first and second parts of the duodenum were the most frequently affected sites. However, our case presented a rare occurrence of duodenal web at the duodenojejunal flexure [10]. It is clear from the above discussion that congenital duodenal web, though less common, remains a differentials in suspected cases of small intestinal obstruction in neonate. Intermittent bilious vomiting may provide an additional clue and CT abdomen may be of help in such cases.
Gupta et al. have reported congenital duodenal web that were found near duodeno-jejunal flexure with good outcome in 2 out of 3 cases [6]. Webs at duodeno-jejunal flexure are always surgically challenging and at the same time poses a huge challenge to the treating neonatologist due to heightened risk of sepsis during post operative period.
The case we have presented is mostly one of the very few cases who have atypical presentation with the site of obstruction being at the duodenojejunal flexure, which itself is a rare site, There has been no recurrence any symptoms till now. The neonate is healthy during follow-up visit and has been growing well.
Conclusion
The case highlights congenital duodenal web as a rare cause of small intestinal obstruction in neonates. Intermittent bilious emesis is an important clinical manifestation and should help in suspecting an underlying problem and CT abdomen may be of significant help in cases where initial investigations are inconclusive.
Availability of data and materials
Available on request.
References
Juang D, Snyder CL (2012) Neonatal bowel obstruction. Surg Clin North Am 92(3):685–x. https://doi.org/10.1016/j.suc.2012.03.008
Verma A, Rattan KN, Yadav R (2016) Neonatal intestinal obstruction: a 15 year experience in a tertiary care hospital. J Clin Diagn Res 10(2):SC10-1SC13. https://doi.org/10.7860/JCDR/2016/17204.7268
Poddar U, Jain V, Yachha SK, Srivastava A (2016) Congenital duodenal web: successful management with endoscopic dilatation. Endosc Int Open 4(3):E238–E241. https://doi.org/10.1055/s-0041-110955
Lin HH, Lee HC, Yeung CY et al (2012) Congenital webs of the gastrointestinal tract: 20 years of experience from a pediatric care teaching hospital in taiwan. Pediatr Neonatol 53(1):12–17. https://doi.org/10.1016/j.pedneo.2011.11.004
Beeks A, Gosche J, Giles H, Nowicki M (2009) Endoscopic dilation and partial resection of a duodenal web in an infant. J Pediatr Gastroenterol Nutr 48(3):378–381. https://doi.org/10.1097/mpg.0b013e31818c600f
Gupta R, Mathur P, Gubbi S, Gupta PK, Shukla R, Bhandari A (2016) More distally located duodenal webs: a case series. J Neonatal Surg 5(4):56. https://doi.org/10.21699/jns.v5i4.435
Sarin YK, Sharma A, Sinha S, Deshpande VP (2012) Duodenal webs: an experience with 18 patients. J Neonatal Surg. 1(2):20 Published 2012 Apr 1.
Jex RK, Hughes RW Jr (1986) Endoscopic management of duodenal diaphragm in the adult. Gastrointest Endosc 32(6):416–419. https://doi.org/10.1016/s0016-5107(86)71927-5
Bailey PV, Tracy TF Jr, Connors RH, Mooney DP, Lewis JE, Weber TR (1993) Congenital duodenal obstruction: a 32-year review. J Pediatr Surg 28(1):92–95. https://doi.org/10.1016/s0022-3468(05)80364-1
Siva Kumar SS, Dasaratha Rao L, Rao KVJ (2014) Congenital intrinsic duodenal obstruction [webs] - 13 case series and review of literature. Surgery Journal. 1(1):85–88. https://doi.org/10.9790/0853-14818588
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
AM collected the data and involved in case management. DN drafted the initial manuscript and was involved in case management. AP was the chief surgeon for the case and contributed in proofreading the manuscript. VK contributed in compiling and critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Case report approval is waived from institutional ethics committee.
Consent for publication
Written informed consent from parents have been obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mudugere, A., Pradhan, A., Kumar, V. et al. A case of intermittent bilious emesis in a term neonate: a case report and brief review of literature. Egypt Pediatric Association Gaz 72, 33 (2024). https://doi.org/10.1186/s43054-024-00274-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00274-2