Abstract
Background
The incidence of thyroid cancer has been increasing among the population less than 20 years of age, especially during the second decade of life. Differentiated papillary thyroid cancer is the most common pathology in children. It usually presents with thyroid nodules with or without cervical lymphadenopathy. Thyroid nodules carry a considerable risk of malignancy in children.
Case presentation
We herein report a 5-year-old girl with poorly differentiated papillary thyroid cancer which is an extremely rare finding at this age. The patient underwent right thyroid lobectomy followed by left hemi thyroidectomy and right central and lateral neck dissection. Pathologic examination revealed a poorly differentiated papillary thyroid carcinoma with nodal deposits.
Conclusion
It is essential to raise awareness of proper evaluation and management of thyroid nodules at such an age.
Similar content being viewed by others
Background
Thyroid cancer is a rare diagnosis in the pediatric population. It represents only 1.8% of thyroid cancer occurrence in all age groups [1]. Most pediatric thyroid cancer cases occur in the population of 10–19 years of age with rare occurrences below 10 years of age. Recently, the incidence has been increasing in the USA [2]. The ratio is higher in females than males being five times more common in females during adolescence [3]. Irradiation exposure is the most important risk factor for developing papillary thyroid carcinoma (PTC) in children [4].
The World Health Organization (WHO) classifies Differentiated Thyroid cancer (DTC) into many subtypes with Papillary thyroid cancer (PTC) representing 90% of the cases, in second place comes Follicular thyroid carcinoma (FTC) however uncommon. Medullary thyroid carcinoma, poorly differentiated carcinoma, and anaplastic carcinomas are rare in young patients [5]. Thyroid mass is the most common presentation in children. However, PTC may commonly present with cervical lymph node enlargement with or without a thyroid mass [6].
Poorly differentiated thyroid carcinoma (PDTC) was introduced into the WHO classification in 2004, it has been considered an intermediate between well-differentiated thyroid carcinoma and undifferentiated thyroid carcinoma both morphologically and behaviorally [7]. Diagnosis can be made based on Turin Criteria which include the presence of the following: (1) solid/trabecular/insular growth pattern; (2) the absence of nuclear features of papillary thyroid carcinoma; and (3) one or more of the following three features: convoluted nuclei, mitotic index of 3 or more per 10 HPF, and tumor necrosis [8].
The diagnosis of PDTC is an important prognostic factor as it carries a much worse prognosis than well-differentiated thyroid cancer with a 10-year survival rate of 50% [9].
Case presentation
A 5-year-old girl presented to our hospital with a painless neck swelling dating from 6 months ago. Initial evaluation showed no changes in her appetite, weight, bowel habits, or sleep pattern. There were also no associated symptoms. The patient’s parents denied any changes in her voice or breathing pattern recently, and no history of radiation exposure. There was no past history of medical diseases. Family history was unremarkable in both parents’ families.
On physical examination, height and weight were within normal ranges for age. General examination of the patient showed normal appearance, body built, and complexion. Vital signs showed a pulse count of 86, Blood pressure of 100/60 mmHg, Temperature of 37.2 ℃, and a respiratory rate of 23. Thus, there were no remarkable changes that could raise suspicion of hypo or hyperthyroidism. She had an olive-sized palpable non-tender right thyroid nodule that moved with deglutition, and a few lymph nodes were palpated at the right side of the neck at levels II and III (upper and middle deep cervical lymph nodes).
The thyroid function test results were all within normal ranges. Neck ultrasonography (Fig. 1) showed an enlarged right thyroid lobe with a large solid, wider than taller nodule of mixed echogenicity with microcalcifications (A), its size was about 19 × 14 mm, and radiologically classified as TIRADS IV, this was accompanied by an enlarged upper right upper cervical (B), lower cervical (C), and paratracheal (D) LNs showing cortical thickening, and the lower cervical LNs showed similar echogenicity to the thyroid nodule.
Neck ultrasonography showing A right thyroid lobe with a single nodule (19 × 14 mm) with cystic and solid parts, ill-defined outline, and foci of micro-calcifications. B Right upper cervical lymph nodes and C right lower cervical lymph nodes, both being distorted with abnormal shape and absent hila. D Paratracheal lymph nodes
The clinical and radiologic findings raised the suspicion of a malignant thyroid nodule, thus requiring a biopsy. Fine needle aspiration cytology was performed showing bloody material and no detected atypical cells, Bethesda I. Based on the earlier findings, the possibility of carcinoma could not be excluded and a diagnostic right lobectomy with an intraoperative frozen section was planned after MDT discussion and counseling with the patient’s family. Since the FNAC results were not conclusive for PTC and there were no symptoms or signs suggestive of distant metastases, preoperative metastasis workup was not recommended for the patient.
A preoperative laryngeal examination was carried out by an otolaryngologist and confirmed the presence of bilateral freely mobile vocal cords.
The right lobectomy was performed through a Kocher collar incision, and the specimen was sent for intraoperative frozen section examination. The result was conclusive for poorly differentiated papillary thyroid cancer. This was followed by a completion left hemithyroidectomy and right central (levels VI and VII) and lateral lymph node dissection (levels II, III, and IV) (Fig. 2) which was carried out after extending the incision into a hockey stick neck incision in the right side. The recurrent laryngeal nerves were identified on both sides and marked to be safe and uninjured, the tumor was on the anterior surface of the right thyroid away from the right recurrent laryngeal nerve. This with the fact that no changes happened to the voice or the breathing of the child after the surgery disputed the need to perform a post-operative laryngeal examination.
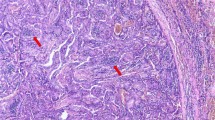
Examination of prepared slides from the right lobe revealed infiltration by tumor tissue (2.5 × 1.5 × 1 cm) in size, formed of atypical epithelial cells, mostly arranged in trabecular and insular patterns. These exhibit a moderate degree of nuclear atypia with mitotic activity of about 3/10 HPFs. There is difficulty identifying nuclear grooving and pseudo inclusions. However, minute foci showed an attempt for papillary configuration (< 5% of tumor tissue). No significant tumor necrosis. The surrounding thyroid tissue showed unremarkable changes. Tumor tissue was seen reaching the capsule, with extrathyroidal extension and multiple satellites. No perineural tumor invasion was detected in the examined material (Fig. 3). The left lobe revealed variable-sized thyroid follicles lined by low cuboidal to flat cells and containing eosinophilic colloid. It was free from tumor tissue. Free thymic tissue was also noted. Sections prepared from the right central nodes revealed infiltration of ten out of eleven nodes dissected, while five out of thirty-four lateral cervical nodes were infiltrated.
The patient was then referred to a nuclear medicine physician. Adjuvant radioactive iodine 131 (RAI131) therapy was decided since the patient was categorized as high risk according to the ATA classification system. The activity of RAI therapy was decided to be 30 mci. The benefits and risks of RAI131 for the patient and her family were discussed with the parents. A whole-body scan with SPECT-CT was performed 4 days after RAI 131 intake showing increased uptake of the tracer at the thyroid bed, clear lung fields, no bony metastasis, and no uptake by the cervical LNs.
Then the patient started Levothyroxine suppressive therapy (75 µg daily). Six months after receiving RAI 131, an assessment of response was performed with a whole-body iodine scan (2 mci), which revealed a complete resolution of the previous uptake seen in the post-treatment scan. Serum-stimulated thyroglobulin level was within normal range and neck ultrasound was free. The patient was scheduled for regular follow-up visits every 6 months, to be monitored by neck imaging and laboratory tests. After more than 1 year of follow-up, she was free from local, nodal, or distant recurrence.
Discussion
Thyroid cancer is not commonly observed in pediatrics less than 10 years of age. According to the Surveillance, Epidemiology and End Result Program (SEER), In the USA in the period from 2016 to 2020, the incidence rate of thyroid malignancies below the age of 10 years is 0.1 per 100,000. However, the incidence rate from 10 to 19 years old ranges from 1.0 to 3.4 per 100,000 [10]. A recent study by Tawde et al. studied the incidence of thyroid cancer in 1175 pediatric patients occurring between 2000 and 2016 and found that most diagnosed cases lay between 15 and 19 years of age [11]. Another study by Hogan et al. reviewed 1753 cases of pediatric thyroid carcinoma in ages ranging from 0 to 19 years old occurring in the period from 1973 to 2004. Only 5.4% of the cases were younger than 10 years of age [3]. In our case, the patient was 5 years old which is considered a rare age to diagnose such a disease.
Many risk factors are attributed to the development of thyroid cancer in children. Most importantly, radiation exposure; It was proven that subjection to 10 Gy of radioactivity during childhood increases the risk of DTC development fifteen times, compared to individuals who have never been subjected [12]. In all ages, exposure of the neck to radiation increases the risk ten times [13,14,15]. Other risk factors include thyroid diseases (e.g., autoimmune thyroiditis) and genetic predisposition (e.g., familial adenomatous polyposis). Our patient was not exposed to any of the known risk factors. Also, she did not have any family history that could suggest the presence of a familial genetic mutation.
In all the previously mentioned studies, well-differentiated PTC was the most prevalent histological subtype of pediatric thyroid cancer [3, 10, 11]. However, in our case, the pathology report revealed a poorly differentiated papillary thyroid cancer which is an atypical finding at this age. There are a few criteria that may suggest malignancy, radiation exposure, and family history of thyroid cancer during history taking. The increase in nodule size and the presence of any compression manifestations such as hoarseness of voice and dyspnea—also, the presence of cervical lymphadenopathy may also suggest malignancy [16]. Only the presence of enlarged cervical lymph nodes was elicited in the patient, this raised the possibility of a malignant thyroid nodule.
The current recommendations show that the best diagnostic modality after the physical examination is done using neck US and FNA cytology if needed [17]. FNA cytology is interpreted using the Bethesda scoring system; in our case, it got Bethesda score 1, undetermined cytology; in these cases, the likelihood of malignancy is as low as 20% of reported cases [17]. This percentage, however, could not dispel the doubt of malignancy and that is why the operation was performed and revealed poorly differentiated PTC.
Our patient underwent right thyroid lobectomy with an intraoperative frozen section which confirmed the malignancy, then went on for a completion left hemithyroidectomy with right central and lateral neck dissection. The current recommended approach to neck dissection in the pediatric age group shows that it is recommended to do central neck dissection in case of any preoperative clinical or radiological sign of malignancy. And to do lateral neck dissection in cases of proven infiltration of them [18]. Adequate central neck dissection has the potential to improve the effectiveness of 131I treatment for distant metastases and is linked to a lower risk of persistent/recurrent loco-regional illness [19].
Pathological examination of the specimen confirmed the diagnosis of PDTC according to Turin criteria [7] since the specimen included wide areas of insular pattern, near absence of papillary structures, and mitotic activity of 3/10 HPF.
According to the American Thyroid Association (ATA) stratification system, the patient’s case was classified as an ATA pediatric high risk for recurrence and distant metastases due to extensive regional disease (n1b) [18]. This favored the decision to start RAI therapy. Determination of the activity may be done empirically (e.g., child’s weight in kilograms/70 kg) based on the typical adult activity used to treat similar disease extent [20]. An adult with the same risk criteria may receive an empiric dose (80–120 mci). The patient weighed 23 kg at the time of examination. So, the recommended activity should be between 26 and 37 mci. Another method is based on body weight alone (1.0–1.5 mci/kg). So, the recommended activity based on the second method should be between 23 and 35 mci [21]. An average of both methods was calculated and started for the patient.
Conclusion
Despite being rare, thyroid cancer should always be put into consideration in pediatric patients with neck swellings. Once clinically suspected, neck ultrasonography and fine needle aspiration can help reach an accurate diagnosis and design an adequate treatment plan for such a disease with an exceptionally good prognosis if properly managed.
Availability of data and materials
All the clinical, radiological, and pathological data used in this manuscript are available on the Mansoura University medical system (Ibn Sina Hospital management system). http://srv137.mans.edu.eg/mus/newSystem/.
Abbreviations
- CT:
-
Computerized tomography
- DTC:
-
Differentiated thyroid cancer
- FNA:
-
Fine needle aspiration
- FTC:
-
Follicular thyroid cancer
- LNs:
-
Lymph nodes
- MRI:
-
Magnetic resonance imaging
- PTC:
-
Papillary thyroid cancer
- SEER:
-
Surveillance, Epidemiology, and End Results
- US:
-
Ultrasound
- ATA:
-
American Thyroid Association
References
Assessment UENC for E. (2009) SEER cancer statistics review, 1975–2012
Vergamini LB, Frazier AL, Abrantes FL, Ribeiro KB, Rodriguez-Galindo C (2014) Increase in the incidence of differentiated thyroid carcinoma in children, adolescents, and young adults: a population-based study. J Pediatr 164(6):1481–1485
Hogan AR, Zhuge Y, Perez EA, Koniaris LG, Lew JI, Sola JE (2009) Pediatric thyroid carcinoma: incidence and outcomes in 1753 patients. J Surg Res 156(1):167–172
Sinnott B, Ron E, Schneider AB (2010 )Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev 31(5):756–73.[cited 2022 Aug 16] Available from: https://academic.oup.com/edrv/article/31/5/756/2354856
Travis WD, Brambilla E, Müller-hermelink HK, Harris CC (2004). World Health Organization Classification of Tumours WHO Classification. Pathology & Genetics Tumours of the Lung, Pleura, Thymus and Heart. IARC/Press 9–122. [cited 2022 Aug 16]. Available from: https://books.google.com/books/about/Pathology_and_Genetics_of_Tumours_of_End.html?Id=id-AL7mFv8IC
Karapanou O, Tzanela M, Vlassopoulou B, Kanaka-Gantenbein C (2017) Differentiated thyroid cancer in childhood: a literature update. Hormones. 16(4):381–7. [cited 2023 May 25]. Available from: https://link.springer.com/article/https://doi.org/10.14310/horm.2002.1758
Pathology and Genetics of Tumours of Endocrine Organs - Google Books. [cited 2023 Nov 22]. Available from: https://books.google.com.eg/books?Hl=en&lr=&id=id-AL7mFv8IC&oi=fnd&pg=PA18&dq=Delellis+RA,+Lloyd+RV,+Heitz+PU,+Eng+C.+WHO+classification+of+tumours+of+endocrine+organs.+Lyon:+International+Agency+for+Research+on+Cancer+(IARC)%3B+2004.&ots=32pqrsaidj&sig=rjx9nukvrjeolcbtyxdvvzfea9e&redir_esc=y#v=onepage&q=Delellis%20RA%2C%20Lloyd%20RV%2C%20Heitz%20PU%2C%20Eng%20C.%20WHO%20classification%20of%20tumours%20of%20endocrine%20organs.%20Lyon%3A%20International%20Agency%20for%20Research%20on%20Cancer%20(IARC)%3B%202004.&f=false
Volante M, Collini P, Nikiforov YE, Sakamoto A, Kakudo K, Katoh R et al (2007) Poorly differentiated thyroid carcinoma: the Turin proposal for the use of uniform diagnostic criteria and an algorithmic diagnostic approach. Am J Surg Pathol 31(8):1256–1264
Volante M, Landolfi S, Chiusa L, Palestini N, Motta M, Codegone A, et al (2004) Poorly differentiated carcinomas of the thyroid with trabecular, insular, and solid patterns: a clinicopathologic study of 183 patients. Cancer. 100(5):950–7 [cited 2023 Nov 22]. Available from: https://pubmed.ncbi.nlm.nih.gov/14983490/
SEER*Explorer Application. [cited 2023 Jun 10]. Available from: https://seer.cancer.gov/statistics-network/explorer/application.html?Site=80&data_type=1&graph_type=3&compareby=sex&chk_sex_1=1&rate_type=2&race=1&advopt_precision=1&advopt_show_ci=on&advopt_show_count=on&hdn_view=1&advopt_show_apc=on&advopt_display=2#resultsregion1
Tawde A, Jeyakumar A (2022) Surveillance, Epidemiology, and End Results Database update for pediatric thyroid carcinomas incidence and survival trends 2000–2016. Int J Pediatr Otorhinolaryngol 1(153):111038
Prasad PK, Mahajan P, Hawkins DS, Mostoufi-Moab S, Venkatramani R (2020) Management of pediatric differentiated thyroid cancer: an overview for the pediatric oncologist. Pediatr Blood Cancer. 67(6):e28141 [cited 2023 May 17]. Available from: https://doi.org/10.1002/pbc.28141
Bhatti P, Veiga LHS, Ronckers CM, Sigurdson AJ, Stovall M, Smith SA, et al 2010 Risk of second primary thyroid cancer after radiotherapy for childhood cancer in a large cohort study: an update from the childhood cancer survivor study. Radiat Res. 174(6):741–52. [cited 2023 May 17]. Available from: https://pubmed.ncbi.nlm.nih.gov/21128798/
Veiga LHS, Lubin JH, Anderson H, De Vathaire F, Tucker M, Bhatti P, et al (2012) A pooled analysis of thyroid cancer incidence following radiotherapy for childhood cancer. Radiat Res. 178(4):365–76 [cited 2023 May 17]. Available from: https://pubmed.ncbi.nlm.nih.gov/22857014/
Michaelson EM, Chen YH, Silver B, Tishler RB, Marcus KJ, Stevenson MA, et al (2014) Thyroid malignancies in survivors of Hodgkin lymphoma. Int J Radiat Oncol Biol Phys. 88(3):636–41 [cited 2023 May 17]. Available from: https://pubmed.ncbi.nlm.nih.gov/24521679/
Dinauer C, Francis GL (2007) Thyroid cancer in children. Endocrinol Metab Clin North Am. 36(3):779–806 [cited 2023 May 25]. Available from: https://pubmed.ncbi.nlm.nih.gov/17673128/
Monaco SE, Pantanowitz L, Khalbuss WE, Benkovich VA, Ozolek J, Nikiforova MN, et al (2012) Cytomorphological and molecular genetic findings in pediatric thyroid fine-needle aspiration. Cancer Cytopathol. 120(5):342–50 [cited 2023 May 25]. Available from: https://pubmed.ncbi.nlm.nih.gov/22605559/
Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM, et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid. 25(7):716–59 [cited 2022 Aug 16]. Available from: https://pubmed.ncbi.nlm.nih.gov/25900731/
Handkiewicz-Junak D, Wloch J, Roskosz J, Krajewska J, Kropinska A, Pomorski L, et al (2007) Total thyroidectomy and adjuvant radioiodine treatment independently decrease locoregional recurrence risk in childhood and adolescent differentiated thyroid cancer. Journal of Nuclear Medicine. 48(6):879–88 [cited 2022 Aug 16]. Available from: https://jnm.snmjournals.org/content/48/6/879
Hung W, Sarlis NJ (2002). Current controversies in the management of pediatric patients with well-differentiated nonmedullary thyroid cancer: a review. Thyroid. 12(8):683–702 [cited Jul 22]. Available from: https://pubmed.ncbi.nlm.nih.gov/12225637/
Jarza̧b B, Handkiewicz-Junak D, Włoch J (2005). Juvenile differentiated thyroid carcinoma and the role of radioiodine in its treatment: a qualitative review. Endocr Relat Cancer. 12(4):773–803. [cited 2023 Jul 22]. Available from: https://pubmed.ncbi.nlm.nih.gov/16322322/
Acknowledgements
N/A.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. MM: data collection, revision, and editing. ME: conceptualization, writing, and revision. OH and SA: editing and. KZ: preparation and editing of the pathology part.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the study involving human participants followed the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This is a case report in which ethical specific approval can be waived.
The work is original, has not been previously published, and is not currently being considered for publication in any format.
The authors know that publication in this journal is authorized and that they have read and accept the terms and conditions of the Publication Regulations.
Consent for publication
The patient signed written consent for the surgical maneuvers for resection and reconstruction. Consent for publication is available.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohsen, M., Hamdy, O., Ramadan, A. et al. Poorly differentiated papillary thyroid carcinoma in a 5-year-old girl: a case report. Egypt Pediatric Association Gaz 72, 10 (2024). https://doi.org/10.1186/s43054-024-00251-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00251-9