Abstract
Background
Neonatal sepsis is a leading cause of newborn mortality in the developing world. Most of the newborn babies admitted to a neonatal ICU for different reasons acquire hospital-acquired infections. Early and optimal management is pivotal for successful outcomes. However, most of the places lack advanced automated culture facilities. Procalcitonin could potentially be used for early diagnosis of such infection.
Objective
To study the diagnostic role of serum procalcitonin in newborn hospital-acquired sepsis.
Materials and methods
A case–control study was conducted in a tertiary care hospital in northern India.
Results
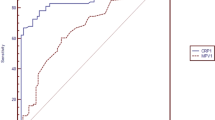
Culture-positive nosocomial sepsis group consisted of 59 patients and the control group of 41 patients. Gram-negative organisms were the most commonly isolated organisms (91.5%). The baseline median and interquartile range (IQR) serum PCT of the study population was 0.3 (0.18–.44) ng/ml. The median (IQR) serum PCT values at the time of clinical deterioration in the nosocomial sepsis and the sepsis-like illness groups are 4 (6.5) ng/ml and 1.2 (1.6) ng/ml, respectively (p = 000). The area under the ROC curve for the prediction of bacterial infection for PCT was 0.864. On the ROC curve, the PCT level that combined the greatest sensitivity and comparatively good specificity was 1.95 ng/ml, with a sensitivity of 88%, and specificity of 79%.
Conclusion
We conclude that serum procalcitonin is a reliable marker for the diagnosis of neonatal nosocomial sepsis.
Similar content being viewed by others
Background
The neonatal intensive care unit (NICU) is a conducive place for disseminating infections, due to a range of patient-specific, disease-specific, and treatment-specific factors [1, 2]. The problem is further compounded in the developing world by the lower availability of resources, low nurse-to-patient ratio, poor infection control practices, and lack of antimicrobial stewardship policies [1]. Some studies from the developing world have reported rates of hospital-acquired sepsis as high as 51–52% among all NICU admissions [3, 4]. These infections are associated with very high mortality rates, high treatment costs, and prolonged hospital stays [5, 6]. Successful treatment of hospital-acquired infections is based on early initiation of appropriate antibiotic therapy. However, due to the stereotypic nature of the illness in neonates, diagnosis of the infection remains challenging [7]. The gold standard for the diagnosis of such infection is blood culture or culture of other sterile body fluids [8]. However, culture reports are available only after 48–72 h making this investigation less useful in guiding the treatment. To avoid delay in the treatment or avoid unnecessary antibiotic use, a rapid, point-of-care, sensitive, and specific laboratory test would be helpful to guide clinicians in deciding whether or not to add antibiotics [9, 10].
Procalcitonin (PCT) is the prohormone of calcitonin and has been reported to be an excellent predictor of infection across different age groups. Previous studies also suggested that PCT may have a high sensitivity for nosocomial neonatal infections [11, 12]. The lower cutoff value for PCT in predicting neonatal sepsis varies from study to study. However, most of the studies have found a procalcitonin threshold of 1 ng/mL or above as a strong predictor of late-onset sepsis in neonates. We conducted a case–control study with the objective to find the usefulness of serum PCT as a reliable diagnostic test for the diagnosis of nosocomial neonatal sepsis.
Methods
This was a case–control study conducted in a tertiary care hospital in northern India, over a period of 24 months from June 2020 to May 2022. The study subjects included babies of all gestational ages admitted in the neonatal ICU of the hospital for various indications, with a negative initial septic screen (defined as negative initial screening blood culture or other sterile body fluid cultures, first-day serum PCT level less than 1 ng/mL and Hs-CRP level less than 6 ng/mL), who developed presumed hospital-acquired sepsis (nosocomial sepsis) while in the hospital. We excluded babies who were on prior antibiotics or various cultures taken after the 1st dose of the antibiotic, post-surgical babies, babies with necrotizing enterocolitis, an inborn error of metabolism, and babies with major congenital anomalies from the study. Suspected hospital-acquired sepsis included patients who developed any one of the following during their hospital course: poor feeding, lethargy, poor neonatal reflexes, temperature instability, respiratory distress, tachycardia, and poor perfusion. These patients were enrolled in the study and were further divided into 2 groups: the confirmed nosocomial sepsis group (a neonate with clinically suspected sepsis and positive blood culture and/or CSF culture and/or urine culture (supra-pubic tap) and the control group (a baby with suspected nosocomial sepsis and negative blood and/or CSF, and/or urine culture). A standard data extraction form was prepared to capture the baseline demographic and clinical data from the studied population. All the enrolled patients underwent full baseline septic work which included complete blood count (CBC), blood culture, and baseline procalcitonin. CSF analysis and urine culture were done at baseline only when clinically indicated. Patients who developed any sign of nosocomial sepsis underwent repeat full septic profiles which included blood culture, CSF analysis, and/or urine culture (supra-pubic tap). The blood culture specimen was cultured using BacTAlert (Biome Rieux, India®) automated blood culture system. Blood culture was considered negative only after 4 days of incubation. CSF and urine culture was done using the semi-quantitative method in which urine was inoculated on the CLED agar plat, and incubated at 35℃, overnight. PCT was measured by a fluorescence immunoassay using QDX Instacheck.
The recorded data was compiled and entered in a spreadsheet (Microsoft Excel) and then exported to the data editor of SPSS Version 20.0 (SPSS Inc., Chicago, Illinois, USA). Shapiro Wilk test was done for the normality test in the case of continuous variables. Parametric data has been represented by mean ± SD and non-parametric data by median (IQR). Nominal data is represented by N (%). The receiver operating characteristic (ROC) curve was constructed to find the AUC for procalcitonin. Statistical significance is taken as 0.05, and data with a value < 0.05 is taken as significant. The sample size was calculated by using Statulator, a free online sample calculator (https://statulator.com/SampleSize/s1P.html). Assuming the 92% sensitivity of the blood PCT for the diagnosis of neonatal sepsis, and an expected prevalence rate of hospital-acquired neonatal sepsis of 30%, the study required a minimum sample size of 95 patients.
The study got ethical approval from the Institutional Ethics Committee (IEC-SKIMS) (No. SIMS 1131/1EC-SKIMS/2021). Written informed consent was taken from the legal guardians before enrolling the subjects into the study.
Results
During the study period, a total of 1110 inborn patients were admitted to our NICU. A total of 143 patients developed suspected nosocomial sepsis during the study period. Forty-three patients were excluded after applying the inclusion and exclusion criteria. A total of 100 patients were enrolled in the study. On the basis of the results of the various culture studies, study patients were divided into two groups: the “nosocomial sepsis group” (culture positive), with 59 patients in the group, and the “sepsis like illness group” (negative culture reports) consisting of 41 patients. The baseline demographic and clinical characteristics of the study population are shown in Table 1. Nosocomial sepsis was diagnosed by positive blood culture for different organisms in 45 patients, positive CSF culture for 10 patients, and positive urine culture for four patients. The organism profile of the culture-positive group was Acinetobacter Baumannii (33), Klebsiella pneumoniae (12), Escherichia coli (7), staphylococcus aureus (3), Pseudomonas aeruginosa (2), and Candida albicans (2). The baseline laboratory variables are shown in Table 2. The median (IQR) baseline (1st day of admission) serum PCT of the study population (N = 100) was 0.3 (0.18–0.44) ng/ml. The median (IQR) serum PCT values at the time of clinical deterioration in the nosocomial sepsis and the sepsis-like illness groups are 4 (6.5) ng/ml and 1.2 (1.6) ng/ml, respectively. The difference was statistically significant (P = 0.00). It can be seen from the above results that the median baseline PCT value of the study cohort was 0.3 ng/ml only. However, the median PCT value in the nosocomial sepsis group showed statistically significant elevation compared to the “sepsis-like illness” group. The ROC curve was elaborated for PCT at a 95% confidence interval. The area under the ROC curve (Fig. 1) for the prediction of bacterial infection for PCT was 0.864 (95% confidence interval 0.79 to 0.93; p = 0.0001). On the ROC curve, the PCT level that combined the greatest sensitivity and comparatively good specificity was 1.95 ng/ml, with a sensitivity of 88%, specificity of 79%, positive predictive value of 74%, and a negative predictive value of 87%.
Discussion
Nosocomial sepsis in a nursery is a common phenomenon in developing countries and carries very high mortality [6]. The clinical features of sepsis in this population are highly nonspecific, resembling many non-infective disorders like the inborn error of metabolism, ductus-dependent circulation, and birth asphyxia, etc. This often leads to an overuse of high-end antibiotics which includes carbapenems, colistin, glycylcycline class drugs, etc., leading to the emergence of extended drug-resistant bugs in the NICU environment [13]. Blood culture is the gold standard for the diagnosis of sepsis; however, culture reports would be available only after 48–72 h making this investigation less useful in guiding the treatment. Besides, culture facilities may not be available in many sick newborn care units (SNCUs) of the country, thus further limiting its role in the diagnosis. Many acute inflammatory markers which typically rise in sepsis like micro ESR, high-sensitivity C-reactive protein (hs-CRP), and procalcitonin have been extensively studied in neonatal sepsis [9, 10]. Serum procalcitonin particularly has been studied in the diagnosis of systemic bacterial infections in various age groups, the aforementioned marker rises specifically in invasive bacterial infections, particularly in gram-negative sepsis [12], which are the most common organisms seen in our cohort, as well in different places across India [6]. One area that remains largely unexplored is finding the role of serum PCT in differentiating true nosocomial sepsis among clinically suspected patients from “sepsis-like illness” which are very common among admitted neonates. The results of our study found that the said investigation is a reasonably sensitive and specific tool for achieving the said objective. At the cutoff value of 2 ng/ml, PCT was 88.4% sensitive to diagnose culture-positive sepsis among clinically suspected patients. A few studies on the preterm population observed similar results. A retrospective study by Fendler WM [12] et al. on preterm babies found PCT a good parameter that could differentiate between the ‘sepsis-like’ episode and bacterial sepsis. Similarly, in another study by Turner D [11] et al. again on preterm infants with suspected nosocomial sepsis, elevated serum Procalcitonin was associated with a high likelihood for neonatal sepsis, and advocated continued antibiotic therapy. Our study was different from most of the previous studies in terms of the control population and gestational age of the studied population. We included a homogeneous group of newborn babies across all gestations with suspected nosocomial sepsis on the basis of clinical symptoms who were later on divided into culture positive sepsis group and sepsis-like illness group. This indeed represents the common clinical scenario for the use of PCT levels for further management.
Serum PCT rise also depends on the class of organism causing systemic infection with gram-negative sepsis leading to the highest elevation followed by gram-positive sepsis. The coagulase-negative staphylococcal infection causes the least PCT rise. Fendler et al. [12] found the highest elevation in gram-negative sepsis compared to gram-positive sepsis and no sepsis. This is a relevant finding as the gram-negative organisms were isolated in 91.5% of our sepsis patients and are also frequently isolated organisms from most of the NICUs across India. Since the risk of death is higher in gram-negative septicemia, its early identification and aggressive treatment are the cornerstone to a favorable outcome [14, 15]. We collected blood samples for PCT estimation immediately after suspicion of hospital-acquired sepsis and before instituting the antibiotic therapy because appropriate antibiotic therapy is known to rapidly decrease serum PCT levels, thus giving erroneously low levels.
Some studies however have not found serum PCT a good tool for the diagnosis of neonatal sepsis. In a study by Franz et al. [16], the sensitivity and specificity of PCT for patients evaluated after 72 h of life were only 38% and 59%, respectively. They found the highest sensitivity to diagnose culture-positive sepsis with IL8. The possible reason for the low sensitivity and specificity in their cohort was the inclusion of all suspected sepsis patients in their study irrespective of the positive culture report. Of a total of 46 included patients only nine patients were culture positive. IL8 is still not available in most developing countries making the investigation inaccessible for routine use.
The optimal cutoff values for serum PCT varies widely between different studies; therefore, we aimed to define a “cutoff” for serum PCT in nosocomial sepsis that can reliably guide us about the immediate management of the suspected patient. We observed, at a value of 1.95 ng/ml, serum PCT has a sensitivity of 88%, specificity of 79%, positive predictive value of 74%, and a negative predictive value of 87%. Most of the studies have reported sensitivity and specificity values ranging from 60 to 100% and from 79 to 100%, respectively [17,18,19,20]. The most likely explanations for the wide heterogeneity of the sensitivity and specificity in different studies are variations in the study design including the diverse age range, the definition of nosocomial sepsis, and the different nature of the control groups. We studied a homogeneous group of neonates with clinically suspected nosocomial sepsis in which confirmed nosocomial sepsis was made based on culture studies, an approach that closely resembles the clinical scenario where the diagnostic test is intended to be used.
Limitations of the study
The main limitation of our study was the limited sample size and single-centric nature of the study.
Conclusion
We conclude that the serum procalcitonin is a reliable marker for the diagnosis of neonatal nosocomial sepsis. At a value of 1.95 ng/ml, serum PCT has a sensitivity of 88%, a specificity of 79%, a positive predictive value of 74%, and a negative predictive value of 87%. The above results would be invaluable for early optimal treatment of nosocomial sepsis pending culture results and withholding antibiotics in patients with the sepsis-like illness.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Vincent JL, Sakr Y, Singer M, Martin-Loeches I, Machado FR, EPIC III investigators et al (2020) prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 323(15):1478–1487
Wang L, Du KN, Zhao YL, Yu YJ, Sun L, Jiang HB (2019) Risk factors of nosocomial infection for infants in neonatal intensive care units: a systematic review and meta-analysis. Med Sci Monit 1(25):8213–8220
Sjahrodji AM (1990) Nosocomial infections in the Neonatal Intensive Care Unit Department of Child Health, Dr. Hasan Sadikin General Hospital, Bandung. Paediatr Indones 30:191–97
Nagata E, Brito AS, Matsuo T (2002) Nosocomial infections in a neonatal intensive care unit: incidence and risk factors. Am J Infect Control 30(1):26–31
Pessoa Silva CL, Richtmann RR, Santos RM et al (2004) Healthcare-associated infections among neonates in Brazil. Infect Control Hosp Epidemiol 25:772–777
Neonatal morbidity and mortality: report of the National Neonatal-Perinatal Database (2005). National Neonatology Forum (NNPD Network), India. https://www.newbornwhocc.org/pdf/nnpd_report_2002-03.PDF.
Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P et al (2014) Every newborn: progress, priorities, and potential beyond survival. Lancet 384(9938):189–205
Celik IH, Hanna M, Canpolat FE, Pammi M (2022) Diagnosis of neonatal sepsis: the past, present and future. Pediatr Res 91(2):337–350
Eichberger J, Resch E, Resch B (2022) Diagnosis of neonatal sepsis: the role of inflammatory markers. Front Pediatr 8(10):840288
Verboon-Maciolek MA, Thijsen SF, Hemels MA, Menses M, van Loon AM et al (2006) Inflammatory mediators for the diagnosis and treatment of sepsis in early infancy. Pediatr Res 59(3):457–461
Turner D, Hammerman C, Rudensky B, Schlesinger Y, Schimmel MS (2006) The role of procalcitonin as a predictor of nosocomial sepsis in preterm infants. Acta Paediatr 95(12):1571–1576
Fendler WM, Piotrowski AJ (2008) Procalcitonin in the early diagnosis of nosocomial sepsis in preterm neonates. J Paediatr Child Health 44(3):114–118
Banerjee T, Wangkheimayum J, Sharma S, Kumar A, Bhattacharjee A (2021) Extensively drug-resistant hypervirulent Klebsiella pneumoniae from a series of neonatal sepsis in a tertiary care hospital, India. Front Med (Lausanne) 8(8):645955
Wen SCH, Ezure Y, Rolley L, Spurling G, Lau CL, Riaz S, Paterson DL, Irwin AD (2021) Gram-negative neonatal sepsis in low- and lower-middle-income countries and WHO empirical antibiotic recommendations: a systematic review and meta-analysis. PLoS Med 18(9):e1003787
Ershad M, Mostafa A, Dela Cruz M, Vearrier D (2019) Neonatal sepsis. Curr Emerg Hosp Med Rep 7(3):83–90
Franz AR, Kron M, Pohlandt F, Steinbach G (1999) Comparison of procalcitonin with interleukin 8, C-reactive protein and differential white blood cell count for the early diagnosis of bacterial infections in newborn infants. Pediatr Infect Dis J 18(8):666–671
Hatherill M, Tibby SM, Sykes K, Turner C, Murdoch IA (1999) Diagnostic markers of infection: comparison of procalcitonin with C reactive protein and leucocyte count. Arch Dis Child 81:417–421
Linda L Belling, RN, NNP (2006) Neonatal sepsis. Pediatr Neonatol 26:1–27
Adib M, Bakhshiani Z, Navaei F, Saheb Fosoul F, Fouladi S, Kazemzadeh H (2012) Procalcitonin: a reliable marker for the diagnosis of neonatal sepsis. Iran J Basic Med Sci 15(2):777–782
Park IH, Lee SH, Yu ST, Oh YK (2014) Serum procalcitonin as a diagnostic marker of neonatal sepsis. Korean J Pediatr 57(10):451–456
Acknowledgements
Nil.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
JIB and ZMT conceived the idea of the study and wrote the manuscript; SMB was involved in the sample collection. IAQ contributed to the data analysis. BAC supervised the implementation of the study and contributed to the writing of the manuscript. All authors approved the final version of the manuscript and are accountable for all aspects related to the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study got ethical approval from the Institutional Ethics Committee (IEC-SKIMS) (No. SIMS 1131/1EC-SKIMS/2021). Written informed consent was taken from the legal guardians before enrolling the subjects into the study parents before enrolling patients in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhat, J.I., Bhat, S.M., Tramboo, Z.M. et al. Role of procalcitonin in predicting newborn hospital-acquired sepsis: a case–control study. Egypt Pediatric Association Gaz 71, 48 (2023). https://doi.org/10.1186/s43054-023-00193-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00193-8