Abstract
Background
Pyogenic liver abscess is a rare condition in children especially in early infancy. The diagnosis requires a high index of suspicion and treatment has to be aggressive to avoid fatality. There is a rarity of reports of the condition in infancy in the African population. Thus, we report a case of the hepatic abscess with documented hypergammaglobulinemia in a young infant seen at the Lagos University Teaching hospital.
Case presentation
We describe the case of a 38-day-old female infant who presented with 4 weeks history of fever and 2 weeks history of progressive abdominal distension. At the onset of illness abdominal ultrasound suggested hepatic abscess and abdominal CT scan confirmed multiple loculated collections in 3 segments of the liver. Patient had drainage of the abscess and additional investigations revealed hypergammaglobulinemia (IgM, IgG, and IgE) in the patient. She completed 6 weeks of antibiotics and made significant clinical improvement.
Conclusions
Pyogenic liver abscess should be considered in the differential diagnosis of an infant with pyrexia with abdominal swelling, even in the absence of well-established risk factors. A high index of suspicion for underlying primary immunodeficiency is important when the condition is diagnosed in early infancy.
Similar content being viewed by others
Background
Pyogenic liver abscess (PLA) is an uncommon complication in children and is rarely reported in the neonate or in early infancy [1, 2]. However, multiple abscesses may occur in the latter age group with resultant higher morbidity and mortality [3,4,5]. PLA is more common in the developing than developed countries but a recent study reported rising incidence in children in the USA [6,7,8]. Most cases have an identifiable risk factor namely, prematurity, low birth weight, umbilical catheterization, omphalitis, necrotizing enterocolitis, total parenteral nutrition, and immunosuppression. We report a case of an infant with PLA and documented hypergammaglobulinemia seen at the LUTH. Management challenges are also highlighted.
Case presentation
The 38-day-old female infant was referred to our facility with complaints of high-grade fever of 4 weeks and progressive abdominal distension of 2 weeks. She is a product of a normal vaginal delivery at term following an uncomplicated pregnancy. Her birth weight was 2500 g and was discharged a day after delivery. There was no history of omphalitis, umbilical catheterization, or surgery.
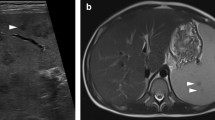
At the onset of illness she was given oral antipyretics (paracetamol) and presented in a private facility where an abdominal ultrasound scan (USS) suggested a diagnosis of hepatic abscess. She was subsequently referred to a tertiary center for expert care. At this facility, an abdominopelvic magnetic resonance imaging (MRI) was requested which revealed hepatomegaly (10.2 cm) and multiple loculated, thick-walled abscesses in 3 segments of the liver (Fig. 1).
Magnetic resonance imaging of the abdomen showing hepatic abscess. The arrows show multiple abscesses in segments 8 (4.0 × 4.3 × 4.8 cm, volume 42 mL), 7 (3.2 × 3.7 × 3.2 cm, volume 19.7 mL), and segment 2 (3.9 × 3.9 × 4.5 cm, volume 35.5 mL) of the liver. The spleen, kidneys, bowel, bile ducts and, the gall bladder were normal
However, by the 2nd day of admission, she developed oliguria and generalized body swelling and was referred to our facility on the clinical suspicion of acute kidney injury (AKI). Her AKI was managed conservatively, and renal function was restored by the 4th day of admission. She had ultrasound-guided needle aspiration of the abscesses on the 18th day of admission and a total of 10 ml and 8.5 ml of fluid was aspirated from the two largest abscesses. Both Gram stain and culture of the aspirate failed to identify any organism and blood cultures were negative. Serum transaminases (alanine and aspartate transaminase) were within normal limits. Table 1 shows abnormal laboratory investigations obtained in the patient while she was on admission.
Screening for hepatitis B, C and human immunodeficiency virus were negative. She had a 3-week course of intravenous levofloxacin, cloxacillin, and metronidazole. Repeat USS on the 21st day of admission showed reduced liver size (8.8 cm) and smaller-sized abscesses (1.9 × 1.8 × 2.2 cm, 1.4 × 0.6 × 1.6 cm, and 2.8 × 1.8.2.0 cm respectively). She was transfused with packed red blood cells twice while on admission and was subsequently discharged home after 25 days on oral medication to complete 6 weeks of antibiotics. Serial ultrasound was to be carried out during her follow-up appointments at the outpatient clinic to monitor the residual abscess. At the point of discharge, samples were also taken for serum immunoglobulins to screen for possible immunodeficiency and the results revealed high levels of IgE [138 (0.0–2.3)g/L], IgM [2.5(0.025–1.5)g/L], and IgG levels [47.9(2.0–7.0)g/L]. IgA level was normal [0.59 (0.59–0.9)g/L].
Discussion
Pyogenic liver abscess (PLA) often presents with non-specific symptoms and signs in children and can pose a diagnostic difficulty [9]. Thus, high clinical suspicion is required for prompt diagnosis and appropriate treatment [1, 2]. Systemic bacterial infection reaching the liver through the hepatic artery is the most common source of bacteria in PLA in children; approximately two-thirds are located in the right hepatic lobe, and in most cases, a predisposing factor is usually identified [3, 4, 6,7,8,9]. In a series of six cases reported by Simeunovic et al. improperly placed umbilical catheter and TPN was demonstrated in 50% of cases and two were HIV-expose [2]. Hendricks and associates reported protein-energy malnutrition as a major contributory factor to the high incidence of liver abscesses in children in the Western Cape [10]. In our patient, a rigorous attempt was made to document the etiology of the abscess but the possible potential risk factor appeared to be sepsis. However, the finding of high levels of serum immunoglobulins is also suspicious. It is not quite clear the cause or effect of this finding. However, it is known that elevated IgG levels can occur secondary to the pyogenic abscess itself. On the other hand, there lies the possibility of a primary immunodeficiency with associated polyclonal dysgammaglobulinemia. The occurrence of liver disease/abscess has been reported in patients with underlying hyper IgM and hyper IgE syndromes [11]. A repeat assay of the immunoglobulins and full immunodeficiency screen was desired in this patient but this was hindered by financial constraints.
Classically, liver abscess presents with fever, hepatomegaly, and right quadrant tenderness or mass as seen in our patient; but this classic presentation is usually rare in neonates and younger children [1, 2, 12]. As demonstrated in our patient, hypoalbuminemia and elevated ESR (and other inflammatory markers) are the most frequently seen laboratory anomalies in PLA [1, 4]. In addition, leukocytosis, anemia, and abnormal liver enzymes were demonstrated in our patient which is typical, although the hepatocellular functions were generally normal [7]. Blood cultures are often negative but abscess specimens commonly yield the offending organisms with Staphylococcus aureus, Klebsiella pneumoniae, Escherichia coli, Streptococcus spp, anaerobes, and Candida spp commonly isolated in children [1,2,3,4,5,6,7,8,9,10,11,12,13,14]. Curiously, neither blood culture nor abscess aspirate yielded the offending organism in our patient, thus we had to treat with empirical broad-spectrum antibiotics based on local experience. We ascribe this finding to the child’s prior exposure to antibiotics and the delayed percutaneous drainage, although this phenomenon may not be uncommon as sterile abscesses have previously been reported even in antibiotics naïve cases [4, 7, 14, 15]. Amebic liver abscess is rare in infants [6, 14].
Acute kidney injury is a common complication in adult patients with PLA [16] and was the reason for referral in our patient. However, although the patient was oliguric at presentation, serum chemistry failed to meet the criteria for AKI and her urine output improved with adequate hydration.
Even though abdominal radiographs can show features suggestive of PLA which include: gas in the abscess cavity, raised right hemidiaphragm, or right pleural effusion in up to 50% of cases [7], abdominal CT and MRI are considered to be more sensitive in detecting and characterizing liver abscesses. Sonography has been demonstrated to have a high yield in the diagnosis of liver abscess with the added advantage of cot side availability, avoids extensive preparation and exposure to ionizing radiation, and is a cheap tool for intervention and follow-up monitoring [1,2,3,4, 11, 13, 17]. Our patient had an abdominopelvic MRI done before being referred to our facility, likely to evaluate for other possible complications while avoiding ionizing radiation.
Without prompt diagnosis and appropriate therapy, PLA is ultimately fatal, and complications are relatively common [7, 18]. Possible complications include pyothorax, peritonitis, hemobilia, and cerebral abscess. Broad-spectrum parenteral antibiotics, initially based on suspected etiology and later adjusted based on results of cultures, is the mainstay of treatment [18]. The optimal duration of antibiotic therapy is usually 4–6 weeks depending on the patient’s clinical response. Parenteral therapy is given for about 2–4 weeks, followed by appropriate oral antibiotics for the remaining duration of therapy [1, 7, 18]. This was the regimen used for our patient with excellent clinical response.
Although multiple abscesses are usually treated conservatively, large abscesses (> 5–7 cm) may benefit from surgical drainage [1, 2]. The indications for intraoperative drainage of hepatic abscess include lack of clinical response after 4–7 days of conservative drainage, multiple large or loculated abscesses, thick-walled abscess with viscous pus, and concurrent intra-abdominal pathology requiring surgery [18]. Minimally invasive techniques, including percutaneous aspiration/drainage and laparoscopic drainage, are other highly effective and more acceptable alternatives with the advantage of less morbidity. As demonstrated in our patient, these minimally invasive techniques could be effective in the treatment of multiple and even loculated abscesses, and obviate the risk of anesthesia associated with open drainage.
Due to financial constraints, detailed investigations of markers of AKI and immunodeficiency screening were not carried out, even though features were sought clinically. The need for larger studies to establish the incidence and predisposing factors of the condition in our environment cannot be overemphasized.
Conclusions
Pyogenic liver abscess should be considered in the differential diagnosis of an infant with pyrexia with abdominal swelling, even in the absence of well-established risk factors. There should be a high index of suspicion for an underlying primary immunodeficiency when the condition is diagnosed in early infancy. Minimally invasive techniques, such as percutaneous aspiration or drainage, could be effective in the treatment of large multiple and even loculated abscesses.
Availability of data and materials
Not applicable.
Abbreviations
- PLA:
-
Pyogenic liver abscess
- MRI:
-
Magnetic resonance imaging
- USS:
-
Ultrasound
- IgG:
-
Immunoglobulin G
- IgE:
-
Immunoglobulin E
- IgM:
-
Immunoglobulin M
- IgA:
-
Immunoglobulin A
- Hb:
-
Hemoglobin
- WBC:
-
White blood cells
- Lym:
-
Lymphocyte
- Neu:
-
Neutrophils
- Eo:
-
Eosinophils
- Mo:
-
Monocytes
- BUN:
-
Blood urea nitrogen
- Na + :
-
Sodium
- K + :
-
Potassium
- Cl:
-
Chloride
- HCO3:
-
Bicarbonate
- Cr:
-
Creatinine
- Ca2 + :
-
Calcium
- PO3:
-
Phosphate
- PT:
-
Prothrombin time
- ESR:
-
Erythrocyte sedimentation rate
References
Kliegman RM, Geme JWS: Nelson Textbook of Pediatrics. E-Book. Elsevier Health Sciences, 2019. https://www.elsevier.com/books/nelson-textbook-of-pediatrics-2-volume-set/kliegman/978-0-323-52950-1.
Simeunovic E, Arnold M, Sidler D, Moore SW (2009) Liver abscess in neonates. Pediatr Surg Int 25:153–156. https://doi.org/10.1007/s00383-008-2307-5
Anand M, Kaur Sahi P, Mantan M (2021) Liver abscess in early infancy with no underlying risk factors: a case series. Trop Doct 51:223–226. https://doi.org/10.1177/0049475520959937
Tan NW, Sriram B, Tan-Kendrick AP, Rajadurai VS (2005) Neonatal hepatic abscess in preterm infants:a rare entity? Ann Acad Med 34(9):558–64.
Moss TJ, Pysher TJ (1981) Hepatic abscess in neonates. Am J Dis Child 135:726–728. https://doi.org/10.1001/archpedi.1981.02130320040014
Mishra K, Basu S, Roychoudhury S, Kumar P (2010) Liver abscess in children: an overview. World J Pediatr 6:210–216. https://doi.org/10.1007/s12519-010-0220-1
Cherry JD, Harrison GJ, Kaplan SL, Hotez PJ, Steinbach WJ: Textbook of pediatric infectious diseases. SeventhPhiladelphia, P.A. (ed): Elsevier/Saunders, [2014; https://www.elsevier.com/books/feigin-and-cherrys-textbook-of-pediatric-infectious-diseases/unknown/978-0-323-39281-5.
Thavamani A, Umapathi KK, Khatana J, Roy A, Augustin T, Radhakrishnan K (2020) Incidence trends, comorbidities, and outcomes of pyogenic liver abscess among children: a nationwide population-based analysis. J Pediatr Gastroenterol Nutr 71:106–111. https://doi.org/10.1097/MPG.0000000000002700
Abiodun M, Osarogiagbon W, Oviawe O (2012) Pyogenic liver abscess mimicking pleural effusion. South African Family Practice 54:459–462. https://doi.org/10.1080/20786204.2012.10874271
Hendricks MK, Moore SW, Millar AJW (1997) Epidemiological aspects of liver abscesses in children in the Western Cape Province of South Africa. J.Trop.Paediatr:103–105. https://doi.org/10.1093/tropej/43.2.103
Rasel M, Zahra F: Hypergammaglobulinemia (Polyclonal Gammopathy). Stat Pearls [Internet, Treasure Island (FL): Stat Pearls Publishing; 2022.
Sharma S, Mohta A, Sharma P (2007) Hepatic abscess in a preterm neonate. Indian Pediatr 44:226–228
Cascio A, Pantaleo D, Corona G et al (2014) Neonatal liver abscesses associated with candidemia: three cases and review of literature. J Matern Fetal Neonatal Med 27:743–749. https://doi.org/10.3109/14767058.2013.837878
Yeh P-J, Chen C-C, Lai M-W, Yeh H-Y, Chao H-C (2020) Pediatric liver abscess: trends in the incidence, etiology, and outcomes based on 20-years of experience at a tertiary center. Original Research Frontiers in Pediatrics 8:111. https://doi.org/10.3389/fped.2020.00111
Bayhan C, Takcı Ş, Ciftçi TT, Yurdakök M (2012) Sterile hepatic abscess due to umbilical venous catheterization. Turk J Pediatr 54:671–673
Sriramnaveen P, Sridhar A, Sandeep Y, et al (2001) Acute kidney injury in patients with pyogenic liver abscess. Renal Failure. 551–552. doi: https://doi.org/10.3109/0886022X.2011.569108.
Sharma MP, Kumar A (2006) Liver abscess in children. Indian J Pediatr. 813–7. doi:https://doi.org/10.1007/BF02790392
Heneghan HM, Healy NA, Martin ST, et al (2011) Modern management of pyogenic hepatic abscess: a case series and review of the literature. BMC Res Notes 4, 80. doi.:https://doi.org/10.1186/1756-0500-4-80
Acknowledgements
The authors acknowledge the contribution of the radiology and pediatric surgical units of the LUTH for their help in unraveling the diagnosis and giving optimal treatment to the patient.
Funding
None. Author funded.
Author information
Authors and Affiliations
Contributions
OF and ND contributed to the conceptualization and design of the study and drafted the initial manuscript. OF, ND, and OA collated the patients’ histories. OA and PA proof read the manuscript. OF, ND, and PA edited the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required for this study in accordance with national guidelines. Exemption was granted by the Lagos University Teaching Hospital Health Research Ethics Committee (LUTHHREC). Health Research Committee Assigned number: ADM/DSCST/HREC/APP/5650.
Written informed consent was obtained from the parent/guardian of these participants. All the information gathered from the patients was handled confidentially, and it was used only for research purposes.
Consent for publication
Written informed consent was obtained from the parent/guardian for the publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adeniyi, O.F., Daniel, N., Ashefor, O. et al. Cryptogenic hepatic abscess in an infant and management challenges in a resource limited setting: a case report. Egypt Pediatric Association Gaz 71, 40 (2023). https://doi.org/10.1186/s43054-023-00188-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00188-5