Abstract
Background
Paroxysmal sympathetic hyperactivity (PSH) is the result of dysregulated autonomic function with sympathetic symptoms characterised by increased heart rate, respiratory rate, blood pressure and temperature with abnormal posture, which predominately occur periodically but can be persistent in severe cases. Common causes that present in similar fashion such as infectious process (bacteremia, meningitis, etc.); non-PSH neurological deterioration (increased intracranial pressure, intracranial haemorrhage, intracranial oedema, seizures, encephalitis); pulmonary embolism; thyrotoxicosis, alcohol or drug withdrawal; neuroleptic malignant syndrome; serotonin syndrome; and malignant hyperthermia need to be excluded before diagnosing PSH. The earlier the diagnosis made, the better the prognosis.
Case presentation
We report a case of a 3-year-old male child who was a diagnosed case of Tetralogy of Fallot presented with left focal seizure with secondary generalisation. Child also had respiratory complaints prior to convulsion. He had developed signs of raised intracranial pressure. Blood culture sent to rule out infective endocarditis was negative. CT brain showed bilateral diffuse cortical infarct. Child developed signs and symptoms of PSH such as fever, tachycardia, tachypnoea, hypertension, diaphoresis, dystonia and bilateral completely dilated pupils. Other common causes such as infective endocarditis, increased intracranial pressure, intracranial oedema, intracranial haemorrhage, seizure, encephalitis and infectious processes (bacteremia, meningitis and infective endocarditis) were ruled out. The diagnosis of PSH was made and started on propranolol along with clonidine. Child responded well to the treatment.
Conclusion
The complex pathophysiology of PSH warrants extensive work-up to rule out other common causes. The outcome of our patient shows the importance of early diagnosis and multidisciplinary treatment for better outcome.
Similar content being viewed by others
Background
Paroxysmal sympathetic hyperactivity (PSH) is a rare acquired clinical syndrome characterised by autonomic symptoms such as tachycardia, hypertension, diaphoresis, posturing and tachypnoea. It can be due to varied causes resulting in diffuse brain injury. It is mainly diagnosed by excluding other causes such as infectious process (bacteremia, meningitis, etc.); non-PSH neurological deterioration (increased intracranial pressure, intracranial haemorrhage, intracranial oedema, seizures, encephalitis); pulmonary embolism; thyrotoxicosis; alcohol or drug withdrawal; neuroleptic malignant syndrome; serotonin syndrome; and malignant hyperthermia (Table 1). PSH is well known in adult age group and least reported in paediatric age group because of lower incidence, lack of awareness of the condition, lower incidence of CNS strokes, physiological tachycardia and infections masking the manifestations. PSH was first described by Penfield in 1929. Various terminologies like diencephalic seizures, paroxysmal autonomic instability with dystonia (PAID) and paroxysmal sympathetic storms were used to describe the events. Most common causes of PSH are traumatic brain injury, stroke and hypoxic brain injury. The diagnosis of PSH is made by high index of suspicion by using paroxysmal sympathetic hyperactivity-assessment measure (PSH-AM) (Table 2) after thorough evaluation to rule out common causes (Table 1) [1]. Recently, few cases have been reported after traumatic brain injury in paediatric age group. Treatment is mainly aimed to control symptoms of excessive sympathetic activity and to prevent damage to peripheral nervous system. Delayed diagnosis may result in unnecessary investigations, prolong mechanical ventilation and hospital stay [2]. If left untreated, patient may develop secondary brain injury from hyperthermia and hypertension and eventually may lead to brain damage and even death [3, 4]. The exact pathogenesis of PSH is unknown until date. However, one of the proposed mechanisms include lack of parasympathetic inhibition because of extensive brain injury and possible damage to Edinger-Westphal nucleus leading to uninhibited action of sympathetic nervous system. We report a case of cerebral infarct presenting with PSH.
Case presentation
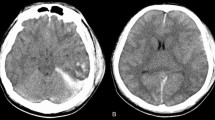
A 3-year-old baby boy with diagnosed Tetralogy of Fallot (TOF) presented with left focal seizure with secondary generalisation with loss of consciousness. Child had fever, cough and respiratory distress prior to admission. Child had history of cyanotic spells noticed from 6 months of age. Cyanosis did not worsen with age and did not seek treatment for TOF. There is no history of recurrent respiratory tract infection and similar complaints in the past. Child’s height, weight and weight for height were within normal range. Chest X-ray revealed boot-shaped heart, and child was started on antibiotics after collecting 3 site blood cultures for suspected infective endocarditis (Fig. 1). 2D echo was consistent with TOF, and there was no evidence suggestive of infective endocarditis or thrombus. Child’s sensorium did not improve after convulsion and developed signs of raised intracranial pressure (ICP). Noticing the pattern of presentation and history of cyanotic heart disease, stroke was suspected. CT brain was suggestive of bilateral massive cortical infarct, right more involved than left (Fig. 2). Child was treated for raised ICP. Child responded to treatment and developed fever on the 16th day of illness. Child was investigated to look for causes of fever. Investigations revealed normal total leukocyte counts (6400/µl), CRP (0.1 mg/dl), negative 3 site blood cultures and urine culture, normal cerebrospinal fluid (CSF) study (no cells, proteins — 10 mg/dl, glucose — 73 mg/dl) and negative CSF culture. He also had bilateral completely dilated pupil but reacting to light (Fig. 3). Child had fever, tachycardia, neurogenic breathing, tachypnoea, hypertension, diaphoresis and dystonia. All the above-mentioned signs were periodic in nature and occurred three or four times daily. Repeat investigations to rule out sepsis and infective endocarditis were negative. Rare possible diagnosis of sympathetic hyperactivity was suspected. Electroencephalogram (EEG) suggested excessive beta activity which can be secondary to hyperstimulation and increased pain perception due to PSH. Child was monitored for the clinical features, and trial of propranolol and clonidine was given. Fever intensity and tachycardia decreased and eventually normalised after increasing the dose of medications. Dystonia responded to clonidine and baclofen. Child eventually got discharged and planned surgical correction in near future.
Discussion
PSH manifests with fever, tachycardia, tachypnoea, hypertension, diaphoresis and dystonia after an acquired brain injury. PSH-AM score was 26 in our patient as described in Table 3. He had probable PSH as per criteria. We had ruled out all other possible causes (Table 1) presented in similar way (normal thyroid function). PSH is more commonly noticed in younger adults after brain injury [5]. PSH is an important clinical problem as case–control studies have shown that the occurrence of PSH leads to poor outcome and prolonged length of hospital stay [6]. In paediatric age group, cases have been published mentioning PSH after traumatic brain injury. Traumatic brain injury is the leading cause of PSH accounting for nearly 79% of PSH cases [2, 5]. Other known causes include stroke, hypoxic ischemic encephalopathy, hypoglycaemic brain injury, central nervous system infections, hydrocephalus and brain tumours [5]. If diagnosed early and treated appropriately, it may take weeks to several months to recover. Our patient developed signs of raised ICP developed after massive cerebral infarct. Child was diagnosed to have PSH during the 3rd week after acute event after ruling out other possible causes such as sepsis, infective endocarditis, neuro infection and convulsion. Trial of propranolol and clonidine was given, and child responded to the treatment which confirmed our diagnosis. While exact mechanism is not known, another proposed mechanism is that uninhibited action of sympathetic nervous system. Third proposed mechanism is excitatory-inhibitory ratio model which states that disconnection of descending inhibition produces maladaptive dendritic arborization and spinal circuit excitation. Sympathetic hyperexcitation causes excessive catecholamine release, manifesting as PSH [7]. The same elevated levels of catecholamine are seen in blood as well [8]. This complex mechanism may require combination of drugs. Most commonly used drugs include propranolol and clonidine. However, opioid, gabapentin and benzodiazepines are also equally effective. The treatment mainly focusses on symptom abortion, prevention of symptoms and refractory treatment. In our patient, we have started with low doses of propranolol and clonidine, and levels increased to get good response. Tachycardia, tachypnoea and hypertension responded to the treatment. However, patient required treatment with gabapentin and levodopa to abort dystonia. Simultaneous care was taken to avoid malnutrition and cyanotic spells. Definitive surgical intervention planned on follow-up for TOF.
Conclusion
PSH is less known entity in paediatric age group, and wide awareness among paediatrician is required as most of the cases goes unnoticed. Diffuse traumatic brain injury is well-known entity to cause PSH and needs further data to support other conditions causing PSH. Early suspicion, diagnosis and appropriate intervention may alter the course of the disease and decrease mortality. Multidisciplinary approach may significantly alter the course of illness and final outcome.
Availability of data and materials
Not applicable.
References
Zheng RZ, Lei ZQ, Yang RZ, Huang GH et al (2020) Identification and management of paroxysmal sympathetic hyperactivity after traumatic brain injury. Front Neurol 11(81):1–14
Hendricks HT, Heere AH, Vos PE (2010) Dysautonomia after severe traumatic brain injury. Eur J Neurol 17:1172–1177
Choi HA, Jeon SB, Samuel S et al (2013) Paroxysmal sympathetic hyperactivity after brain injury. Curr Neurol Neurosci Resp 13:370
Lump D, Moyer M (2014) Paroxysal sympathetic hyperactivity after severe brain injury. Curr Neurol Neurosci Resp 14:494
Perkes I, Baguley IJ, Nott MT et al (2010) A review of paroxysmal sympathetic hyperactivity after acquired brain injury. Ann Neurol 68:126–135
Verma R, Giri P, Rizvi I (2015) Paroxysmal sympathetic hyperactivity in neurological critical care. Indian J Crit Care Med 19(1):34–37
Kitagawa T, Ishikawa H, Yamamoto J et al (2019) Takotsubo cardiomyopathy and neurogenic pulmonary edema after carotid endarterectomy. World Neurosurg. 124:157–160
Feng Y, Zheng X, Fang Z (2015) Treatment progress of paroxysmal sympathetic hyperactivity after acquired brain injury. Pediatr Neurosurg 50:301–309
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
(1) JBJ, data curation, writing — original draft preparation and investigation. (2) VV, data curation and investigation. (3) ARS, data curation and investigation. (4) AV, data curation, investigation and conceptualization. (5) PU, conceptualization, investigation, supervision and reviewing and editing. (6) SK, investigation and supervision. (7) SR, investigation and supervision. (8) CTD, investigation and supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent from the child’s parent for publication was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jomalkar, J.B., Vijayan, V., Saoji, A.R. et al. Paroxysmal sympathetic hyperactivity in a child with stroke: a case report. Egypt Pediatric Association Gaz 71, 35 (2023). https://doi.org/10.1186/s43054-023-00184-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00184-9