Abstract
Background
Nutrition of critically ill children is a frequently ignored issue. The purpose of this study was to describe nutritional practices in the pediatric intensive care unit (PICU) in a resource-limited country and evaluate their association with prognosis.
Methods
This was a prospective observational study, conducted on critically ill children admitted into PICU. Nutritional status was assessed, and nutritional practices (enteral and parenteral) were recorded. The primary outcome was PICU mortality.
Results
Two hundred twenty-one patients were recruited. Mortality rate was 17.6%. Parenteral nutrition (PN) administration and longer PN duration were associated with mortality (p<0.001 for each). Early enteral nutrition was associated lower rates of mortality (5.6% vs 26.9%, p<0.001); hospital-acquired infections (18.9% vs 67.3%, p<0.001); and enteral feeding intolerance (13.3% vs 28.8%, p=0.018), compared with late enteral nutrition. Enteral nutrition onset correlated with length of PICU stay (rs=0.66, p<0.001); mechanical ventilation duration (rs=0.53, p<0.001); vasoactive infusion days (rs=0.25, p<0.001); central venous catheter days (rs=0.69, p<0.001); and time to full enteral caloric intake (rs=0.63, p<0.001). Bolus nasogastric feeding was superior to continuous nasogastric feeding since it was associated with a shorter time to full enteral caloric intake, without a higher risk of feeding intolerance or mortality. Malnutrition was associated with higher PN (75.4% vs 60.3%, p=0.03) and mortality (26.2% vs 14.1%, p=0.032) rates, in addition to longer mechanical ventilation duration (p=0.041) and time to full enteral caloric intake (p=0.010).
Conclusion
Malnutrition, PN, and late enteral nutrition are associated with poor outcome of PICU patients. Bolus nasogastric feeding appears to be superior to continuous feeding.
Similar content being viewed by others
Background
Compared with adults, children have a need for growth and have higher energy requirements, but their energy reserves per unit of body mass are more limited [1].
Feeding of critically ill children, in particular, continues to draw attention and raise controversies despite extensive research. Many critically ill children have underlying chronic health disorders which predispose to nutritional deficiencies. Prevalence of acute malnutrition among hospitalized pediatric patients varies between 6.1% and 32% [1]. Among critically ill children, the rate is 24–45% [2, 3]. Previous studies demonstrated that the nutritional status and nutrient delivery have a great impact on clinical outcomes in the pediatric intensive care unit (PICU), including mortality, length of PICU stay, mechanical ventilation duration, and incidence of hospital-acquired infections [3,4,5].
Strictly speaking, the term “malnutrition” includes both “undernutrition’ and “overweight.” However, the term is usually used to refer specifically to “undernutrition.”
The physiologic basis for malnutrition-associated mortality and morbidity includes dysfunction of the heart, liver, and kidney; impaired nutrient digestion and absorption; atrophy of muscles (including respiratory muscles); impaired heat generation and loss; atrophy of glands; and reduced activity of sodium pump, with increased permeability of cell membranes [6].
Unfortunately, many pediatricians still ignore nutritional issues while dealing with critically ill children, paying exclusive attention to such issues as mechanical ventilation, vasoactive medications, and antibiotics. The aim of the present study was to have a global look at the feeding practices inside the PICU of a resource-limited country and to investigate their association with outcomes, which can be of help in updating nutritional protocols and improving quality of care.
Methods
This was a prospective cohort study conducted on 221 patients admitted into a tertiary PICU, belonging to a university hospital from January 2019 to February 2021. The research was reviewed and approved by the Menoufia University Faculty of Medicine Research Ethics Committee, and a written informed consent was obtained from parents. Critically ill children admitted into PICU were eligible for inclusion in the study. Exclusion criteria were expected PICU stay <3 days or age <1 month or >16 years. Upon admission, patients were carefully evaluated. Sepsis screening was performed. Illness severity was determined through pediatric Sequential Organ Failure Assessment (pSOFA) score at the end of first 24 h [7]. Anthropometric measurements were recorded on admission. Malnutrition was diagnosed if body mass index-for-age z score (or weight-for-length for children<2 years) was <−2SD. If accurate height/length was not available (e.g., contractures), weight-for-age z score <-2SD was used to define malnutrition [8].
Nutritional support of critically ill children was instituted according to our local protocol. Initially, enteral feeding was withheld in such conditions as severe respiratory distress, shock, multiple organ dysfunction syndrome, gastric bleeding, intestinal obstruction, persistent vomiting, convulsive status epilepticus, recent surgery, and severe hypernatremic dehydration. If patients were deemed more stable, enteral feeding was initiated orally, but if this seemed unsafe (tachypnea, poor sucking, or swallowing dysfunction), nasogastric feeding was given by continuous or bolus methods according to physicians’ preferences. Enteral feeding onset was classified as either “early” or “late”. “Early” enteral feeding was defined as initiation of enteral feeding within the 1st 48 h of PICU admission. Patients were monitored for enteral feeding intolerance like increased gastric residual, significant abdominal distention, bloody gastric aspirate, vomiting, and increased respiratory distress related to feeding.
Parenteral nutrition (PN) was given through central venous catheter (CVC) to supplement, or replace, enteral feeding, but no definite time was specified for its initiation. Amino acid solution (Aminoven® 10% - Fresenius Kabi Egypt) was started at 1.5 g/kg/day and increased gradually to 3 g/kg/day. Carbohydrate was given as 25% glucose solution at a rate of 5–7 mg/kg/min, which was changed according to plasma glucose level. Insulin infusion was occasionally added to keep glucose level <180 mg/dL. Lipid emulsion (SMOFlipid® - Fresenius Kabi Egypt) was infrequently given because of limited availability. Trace elements solution (Pediatrace- Fresenius Kabi Egypt) consisted of zinc, manganese, fluoride, copper, iodine, and selenium, at a dose of 1 mL/kg/day (maximum 15 mL/day). Water soluble vitamins dose (Soluvit® N - Fresenius Kabi Egypt) were administered at 1 ml/kg/day (maximum 10 ml/day). PN was monitored through periodic laboratory tests, like serum electrolytes, glucose, hemoglobin, hematocrit, creatinine, blood urea nitrogen, bilirubin, albumin, triglycerides, and liver enzymes. Patients were monitored for two main PN complications, namely PN-associated liver disease (PNALD) and central line-associated bloodstream infections (CLABSI). PNALD was diagnosed when serum direct bilirubin was ≥2 mg/dL for ≥2 weeks, after exclusion of other causes [9, 10]. CLABSI was defined according to previous guidelines [11]. Ventilator-associated pneumonia (VAP) was defined according to the Center for Disease Control (CDC) guidelines [12]
Target caloric intake for enteral and parenteral nutrition was 120 kcal/kg/day for children <1 year. For children 1–10 years, the target was 100 kcal/kg/day. For children >10 years, the target was 35 and 65 kcal/kg/day for females and males, respectively. For children with malnutrition, the target in 1st 7 days was 80–100 kcal/kg/day, but was later increased to 150–220 kcal/kg/day.
Primary outcome of the study was PICU mortality. Secondary outcomes included PICU stay, mechanical ventilation duration, vasoactive infusion days, hospital-acquired infections, CVC days, time to full enteral caloric intake, and feeding intolerance.
Statistical methods
A sample size of 140 was found to be needed, using Epicalc2000 software, based on a previous study, and assuming an alpha level (type I error) of 0.05 and a power of 80%.
Number and percent were used to present qualitative variables. Non-normally distributed data were expressed as median and interquartile range. Chi-square test or Fisher exact test was used to evaluate the association between qualitative variables. Mann-Whitney U test was used for comparing non-normally distributed quantitative variables. Correlations between non-normally distributed variables were performed by Spearman’s correlation coefficient. A two-tailed p-value<0.05 was considered statistically significant. All data were analyzed by SPSS version 23 (Statistical Package for Social Science) (Chicago, Inc, IL).
Results
Characteristics of the study population
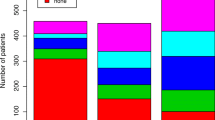
Two hundred twenty-one patients were enrolled. Their demographic, clinical, and baseline laboratory characteristics are shown in Table 1. Patients were admitted to PICU for various reasons, mostly respiratory (30.3%), neurological (29%), and cardiac (10.9%) disorders. Surgery, trauma, and hematology/oncology cases represented 3.2%, 2.3%, and 3.6%.
The overall mortality rate was 17.6%. Mortality rate was 33.3%, 25%, 20.8%, 20%, 19.4%, 18.8%, 12.5%, and 11.1% among patients admitted for renal, toxicological, cardiac, trauma, respiratory, neurologic, infectious, and metabolic disorders, respectively. None died in other patient categories.
Early versus late enteral nutrition
Table 2 compares between “early” and “late” enteral nutrition. The “late” subgroup had significantly higher pSOFA. The rates of mechanical ventilation, vasoactive medication use, and mortality were significantly higher among the “late” group. Mechanical ventilation duration, vasoactive infusion days, CVC days, and PICU stay were significantly longer among the “late” group. The “late” group had significantly higher rates of hospital-acquired infections (mainly CLABSI and VAP) and took a significantly longer time to reach full enteral caloric intake. Enteral nutrition onset demonstrated significant positive correlations with pSOFA score [Spearman correlation coefficient (rs)=0.21, p=0.003], PN duration [rs=0.82, p<0.001], mechanical ventilation duration [rs=0.53, p<0.001], length of PICU stay [rs=0.66, p<0.001], CVC catheter days [rs=0.69, p<0.001], vasoactive infusion days [rs=0.25, p<0.001], and time to full enteral caloric intake [rs=0.63, p<0.001].
General characteristics of survivors and non-survivors
Non-survivors had significantly higher frequencies of malnutrition, acute respiratory distress syndrome (ARDS), mechanical ventilation, hospital-acquired infections, and vasoactive medication use. Non-survivors had also significantly higher pSOFA, vasoactive infusion days, mechanical ventilation duration, CVC days, and PICU stay (Table 3).
Nutritional variables in relation to mortality
Table 4 shows that PN was not given to some patients due to a lack of CVC. PN frequency and duration were significantly greater among non-survivors. Non-survivors had significantly shorter oral feeding duration and a significantly higher incidence of enteral feeding intolerance. 17.9% of non-survivors reached full enteral caloric intake, compared with 87.4% among survivors (p<0.001). No case of PNALD was diagnosed. The frequency of CLABSI among patients who received PN was 30.8%, compared with 5.1% among other children (p<0.001).
Type of nasogastric feeding
No association was found between the initial type of nasogastric feeding (continuous vs bolus) and mortality (Table 4). Bolus feeding was associated with a shorter time to full enteral caloric intake, compared with continuous feeding: median (interquartile range) were [1 (1–3) vs 4 (3–6) days, p<0.001]. The frequency of enteral feeding intolerance was 20.5% among the continuous subgroup, compared with 11.5 % among the bolus subgroup (p=0.090). The mechanical ventilation rate among the continuous group was 21.8%, compared with 38.5% among the bolus group (p=0.019).
Malnutrition and outcome
Malnourished children had significantly younger ages. No significant difference was found between patients with malnutrition and other patients in pSOFA or in the prevalence of sepsis or complex chronic condition. Malnourished children had significantly higher rates of PN, mechanical ventilation, and mortality. They also took a significantly longer time to reach full enteral intake (Table 5). CLABSI rate among malnourished children was 27.9/1000 catheter days, compared with a rate of 29.9/1000 catheter days for other children. VAP rate was 12.9 and 13.3/1000 ventilator days, respectively.
Discussion
Although frequently overlooked, the nutritional status of critically ill children and the feeding practices applied to them in the PICU are of paramount importance since they can affect the clinical outcome.
We found that the frequencies of PN and PN duration were significantly greater among non-survivors. This might reflect the increased incidence of enteral feeding intolerance among non-survivors, which entailed institution of PN. Equally possible, PN contributed to mortality through increasing CLABSI incidence. Similarly, previous studies showed that nutritional status and nutrient delivery exert an appreciable impact on the clinical outcome of critically ill children, including mortality, length of stay, and hospital-acquired infections [13]. Of note, no patients developed PNALD which could be partially explained by infrequent use of lipid emulsions [10].
The absence of a significant difference in PN onset between survivors and non-survivors in our study is consistent with a pediatric multicenter randomized controlled trial (RCT) that failed to find a significant difference in mortality between early and late PN. However, late onset of PN was surprisingly associated with shorter mechanical ventilation duration, shorter length of hospital stay, and less need for renal replacement therapy [14]. Of note, in the latter trial, enteral feeding was attempted, and micronutrients were administered intravenously for both groups. Moreover, it was criticized for several methodological issues [8].
Unlike PN, enteral nutrition appeared to be protective: early enteral nutrition was associated with lower mortality, which is consistent with previous adult [15] and pediatric [16] studies. Early enteral nutrition was also associated with lower rates of mechanical ventilation and vasoactive medication use as well as shorter vasoactive infusion days, mechanical ventilation duration, PICU stay, CVC days, and time to reach full enteral caloric intake.
The link between late enteral nutrition and adverse outcome might not only be nutrient deficiency but also “hospital-acquired infections.” Enteral feeding is known to reduce bacterial translocation and sepsis: lack of enteral feeding creates nutrient scarcity in the distal intestinal tract where the highest burden of intestinal commensal microflora exists, which normally compete with pathogens for nutrients and epithelial cell adhesion sites, in addition to releasing antibacterial substances. Meanwhile, gut ischemia/reperfusion can cause villous injury, increased intestinal permeability, and bacterial translocation [17].
However, it is possible to understand the association of late enteral nutrition with morbidity and mortality as follows: the risk of aspiration and feeding intolerance led physicians to withhold enteral nutrition from the more critically ill children, who are inherently at higher risk of mortality and morbidity and are, meanwhile, more likely to require CVC and mechanical ventilation which predispose to infections. Undoubtedly, RCTs are required to prove the causal association of enteral nutrition with outcomes.
Noteworthy, although enteral nutrition onset was significantly delayed among non-survivors, no significant difference was found in the frequency of enteral nutrition administration between survivors and non-survivors, implying that physicians were aware of the value of enteral nutrition for all patients, including the more critically ill. However, these efforts were thwarted due to a higher rate of enteral feeding intolerance among non-survivors who were also less able to reach full enteral caloric intake. Similarly, in a multicenter study of mechanically ventilated children, intake of a higher percentage of energy target through the enteral route was associated with lower mortality, while PN was associated with higher mortality [13]. It is, therefore, possible to consider enteral feeding intolerance a clinical prognostic marker.
Comparing the initial method of nasogastric feeding, we found that bolus feeding was superior since it was associated with shorter time full enteral intake compared with continuous feeding, without a significant increase in the rate of feeding intolerance or mortality. Importantly, feeding tolerance was more common among the bolus group although they had significantly higher mechanical ventilation rate, which lends more weight to the safety of bolus feeding. Our findings are consistent with a small RCT of mechanically ventilated children wherein bolus feeding was associated with higher energy and protein delivery, and faster time to goal volume, without increased risk of aspiration causing additional lung injury [18]. However, among premature infants, no significant difference was found between the two methods in weight gain, incidence of necrotizing enterocolitis, or time to full oral feeds [19, 20].
Although the frequency of malnutrition in our study was high (29.4%), it was lower than in earlier studies [3, 21]. Additionally, malnutrition was associated with mortality and morbidity. This association with mortality cannot be attributed to greater illness severity on admission (pSOFA score) or underlying chronic illness.
Similarly, the younger age of malnourished children does not seem to have contributed to their higher mortality since “age” was not risk factor for death among the whole study population. Most probably, the younger age of malnourished children reflects greater survival of normally nourished children to older ages.
Consistent with our findings, another study found that malnutrition predicted mortality after adjustment for age, Pediatric Index of Mortality-2, and complex chronic conditions [22]. Similarly, an earlier multicenter study reported an association of malnutrition with mortality after adjustment for illness severity [5]. Conversely, one study failed to replicate the association of malnutrition with mortality [3].
Immune dysfunction is a leading cause of death in malnutrition [5]. It is caused by impaired gut-barrier function, reduced exocrine secretion of protective substances, reduced microbicidal activity of granulocytes, low levels of plasma complement, and atrophy of lymphatic tissues. A vicious circle occurs, whereby malnutrition leads to recurrent infections which, in turn, leads to more severe malnutrition through decreasing appetite, inducing a catabolic state, and increasing demand for nutrients [23].
Surprisingly, we found no association of malnutrition with hospital-acquired infection. This could be attributed to the small size of our study population or to the significantly higher PN rate among malnourished children which might have improved their nutritional status during PICU stay in comparison with other children. If this explanation proves true, it will mean that the liability of malnourished children to infection is not fateful, and proper nutritional interventions inside the PCIU can significantly change the scene. Regrettably, we did not record weight changes throughout the PICU stay.
The higher rate of PN among our malnourished children was not due to poorer tolerance of enteral feeding, but out of caution about advancing enteral feeding to malnourished children whose digestion and absorption are impaired and who have limited tolerance of gastroesophageal reflux. Therefore, to achieve certain caloric intake target, physicians had to rely more on PN.
Consistent with previous studies [3, 5], we noted greater mechanical ventilation rate and mechanical ventilation duration among malnourished children. Malnutrition adversely affects respiratory function through reducing muscle mass and the lack of antioxidant trace elements and vitamins that might ameliorate ventilator-induced diaphragmatic dysfunction [24]. Furthermore, malnourished children frequently have hypophosphatemia which causes muscle weakness and extubation failure through decreasing intermediary compounds for energy production [25].
Finally, we found, in line with a previous study [22], that malnutrition was associated with a significantly longer length of PICU stay, although other researchers failed to replicate this association [3].
The link between nutritional status and prognosis suggests that feeding is a therapy not less important than usual medications. Nevertheless, a question that can’t be answered by data available in the current study is: “Which is more important: acute or chronic malnutrition?”
Importantly, our study population was heterogeneous. Of course, the relation of nutrition to the prognosis of specific groups of PICU patients should be adequately studied, but this was beyond the scope of the current research. In fact, it is desirable, in many situations, to deal with all PICU patients as one lump since many factors (like acidosis, hypoxia, hypoglycemia, shock, and nosocomial infections) influence their outcome regardless of their specific underlying disease states. Nutrition is similarly postulated to influence the outcome of various PICU patients.
In sum, the present study demonstrates that nutrition is a mirror through which one can have a general look at the prognosis of critically ill children. It is hoped that the study will succeed in raising questions and reviving nutritional issues among pediatric intensivists who sometimes feel that such issues can be safely ignored in the context of more serious conditions like mechanical ventilation and shock.
The present study had some limitations. It represents a single center’s experience. Undoubtedly, a multicenter study would yield firmer conclusions. Furthermore, we assessed several nutritional variables simultaneously, and it might be preferred to investigate each variable in a separate study, but our aim from the beginning was to have a comprehensive, rather than a limited, view on the importance of nutrition to PICU patients. Another limitation of the study is its observational nature. Although RCTs remain the best method of proving causality, it is prudent to consider the observational study design as complementary, rather than rival, analytic technique [26]. RCTs will eventually be required to answer the question of whether delayed enteral feeding actually contributed to poor outcome or delayed enteral feeding was just an epiphenomenon accompanying illness severity without a real effect on the outcome. Other patients’ characteristics, like hospital-acquired infections, might have similarly confounded the effect of nutrition on the outcome. Of critical importance, RCTs can reveal whether the practice of withholding enteral feeding from the sicker patients, as followed in the current study, is harmful or useful. Finally, the study was conducted in a country with limited resources, which might have influenced some findings. For instance, lipid emulsions were not consistently included in PN.
Conclusion
PN is associated with mortality while early enteral nutrition is associated lower risk of mortality and morbidity. Bolus nasogastric feeding is superior to continuous feeding in that it was associated with a shorter time to full enteral caloric intake, without increasing feeding intolerance or mortality. Malnutrition is a risk factor for mortality, longer mechanical ventilation duration, and longer time to full enteral caloric intake. The causal association of nutrition with outcome needs to be established by RCTs.
Availability of data and materials
Not applicable
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CDC:
-
Center for disease control
- CLABSI:
-
Central line-associated bloodstream infections
- CVC:
-
Central venous catheter
- PICU:
-
Pediatric intensive care unit
- PN:
-
Parenteral nutrition
- PNALD:
-
Parenteral nutrition-associated liver disease
- pSOFA:
-
Pediatric Sequential Organ Failure Assessment score
- RCT:
-
Randomized controlled trial
- VAP:
-
Ventilator-associated pneumonia
References
Joosten KF, Hulst JM (2008) Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr 20:590–596
Hulst J, Joosten K, Zimmermann L et al (2004) Malnutrition in critically ill children: from admission to 6 months after discharge. Clin Nutr 23:223–232
de Souza MF, Leite HP, Koch Nogueira PC (2012) Malnutrition as an independent predictor of clinical outcome in critically ill children. Nutrition 28:267–270
Castillo A, Santiago MJ, López-Herce J et al (2012) Nutritional status and clinical outcome of children on continuous renal replacement therapy: a prospective observational study. BMC Nephrol 13:125
Bechard LJ, Duggan C, Touger-Decker R et al (2016) Nutritional Status Based on Body Mass Index is associated with morbidity and mortality in mechanically ventilated critically ill children in the PICU. Crit Care Med 44:1530–1537
World Health Organization (1999) Management of severe malnutrition: a manual for physicians and other senior health workers. World Health Organization. https://apps.who.int/iris/handle/10665/41999. Accessed 28 May 2021. ISBN 92 4 154511 9
Matics TJ, Sanchez-Pinto LN (2017) Adaptation and validation of a Pediatric Sequential Organ Failure Assessment Score and evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr 171(10):e172352
Mehta NM, Skillman HE, Irving SY et al (2017) Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. Pediatr Crit Care Med 18(7):675–715
Gura KM, Lee S, Valim C et al (2008) Safety and efficacy of a fish-oil-based fat emulsion in the treatment of PN-associated liver disease. Pediatrics 121:e678–e686
Sanchez SE, Braun LP, Mercer LD, Sherrill M, Stevens J, Javid PJ (2013) The effect of lipid restriction on the prevention of PN associated cholestasis in surgical infants. J Pediatr Surg 48:573–578
O’Grady NP, Alexander M, Burns LA et al (2011) Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 39:S1–S34
Center for Disease Control (CDC) (2022). Identifying Healthcare-associated Infections (HAI) for National Health Care Safety Network Surveillance. Available at:https://www.cdc.gov/nhsn/PDFs/pscManual/2PSC_IdentifyingHAIs_NHSNcurrent.pdf; Accessed 23 Sept 2022.
Mehta NM, Bechard LJ, Cahill N et al (2012) Nutritional practices and their relationship to clinical outcomes in critically ill children--an international multicenter cohort study. Crit Care Med 40:2204–2211
Fivez T, Kerklaan D, Mesotten D et al (2016) Early versus Late PN in Critically Ill Children. N Engl J Med 374:1111–1122
Artinian V, Krayem H, DiGiovine B (2006) Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest 129:960–967
Mikhailov TA, Kuhn EM, Manzi J et al (2014) Early enteral nutrition is associated with lower mortality in critically ill children. JPEN J Parenter Enteral Nutr 38(4):459–466
Papoff P, Ceccarelli G, d'Ettorre G et al (2012) Gut microbial translocation in critically ill children and effects of supplementation with pre- and pro biotics. Int J Microbiol 2012:151393
Brown AM, Fisher E, Forbes ML (2019) Bolus vs continuous nasogastric feeds in mechanically ventilated pediatric patients: A pilot study. JPEN J Parenter Enteral Nutr 43:750–758
Premji SS, Chessell L (2011) Continuous nasogastric milk feeding versus intermittent bolus milk feeding for premature infants less than 1500 grams. Cochrane Database Syst Rev 2011(11):CD001819
van der Star M, Semmekrot B, Spanjaards E, Schaafsma A (2012) Continuous versus bolus nasogastric tube feeding in premature neonates: Randomized controlled trial. Open J Pediatr 2:214–218
Leite HP, Isatugo MKI, Sawaki L, Fisberg M (1993) Anthropometric nutritional assessment of critically ill hospitalized children. Rev Paul Med 111:309–313
Ventura JC, Hauschild DB, Barbosa E et al (2020) Undernutrition at PICU admission is predictor of 60-day mortality and PICU length of stay in critically ill children. J Acad Nutr Diet 120:219–229
Rytter MJ, Kolte L, Briend A, Friis H, Christensen VB (2014) The immune system in children with malnutrition--a systematic review. PLoS One 9(8):e105017
Boles JM, Bion J, Connors A et al (2007) Weaning from mechanical ventilation. Eur Respir J 29:1033–1056
Santana e Meneses JF, Leite HP, de Carvalho WB, Lopes JE (2009) Hypophosphatemia in critically ill children: prevalence and associated risk factors. Pediatr Crit Care Med 10:234–238
Ligthelm RJ, Borzì V, Gumprecht J, Kawamori R, Wenying Y, Valensi P (2007) Importance of observational studies in clinical practice. Clin Ther 29(6 Pt 1):1284–1292
Acknowledgements
None
Funding
No funding or grants were received for conducting this study
Author information
Authors and Affiliations
Contributions
Study conception and design: Muhammad Said Elmekkawy and Alyaa Ahdy Abdelaziz; data collection: Gamal Ibrahim Shabaan, Muhammad Said Elmekkawy, and Alyaa Ahdy Abdelaziz; analysis and interpretation of results: Muhammad Said Elmekkawy and Alyaa Ahdy Abdelaziz; and draft manuscript preparation: Muhammad Said Elmekkawy. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Menoufia University Faculty of Medicine Research Ethics Committee: approval number: 1/2019PEDI
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Mekkawy, M.S., Shabaan, G.I. & Abdelaziz, A.A. Feeding: the hidden variable affecting prognosis of critically ill children. Egypt Pediatric Association Gaz 70, 40 (2022). https://doi.org/10.1186/s43054-022-00136-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-022-00136-9