Abstract
Background
Cow’s milk is known to be the most frequent food allergen in infants in the first years of life. Eliminating cow milk protein from diets and reintroducing it with a challenge test are the main methods for sure diagnosis. Cow’s Milk-related Symptom Score (CoMiSS) has been developed for primary health care providers to improve their knowledge about CMPA.
Objective
This study was conducted to prescribe clinical presentation of cow’s milk allergy among infants.
Methods
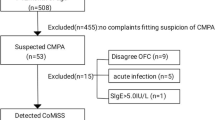
A cross-sectional study was conducted at Gastroenterology and Nutrition Unit, University Children Hospital, from the 1st of January 2020 to the 31st of December 2020. Forty infants, complaining of recurrent or persistent gastrointestinal manifestations, were included in our study (28 males and 12 females). Those infants were subjected to detailed medical and social patient history, comprehensive physical exam, and CoMiSS scoring as an awareness tool to suspect underlying cow milk allergy. Infants with a CoMiSS of more than 12 points and positive elimination rechallenge test were regarded as eligible to be part of our study.
Results
This study showed that the most frequently occurring gastrointestinal manifestations associated with CMPA were regurgitation (92%), diarrhea (80%), colic (75%), vomiting (67.5%), and lastly constipation which represents only (5%).
Conclusion
Regurgitation and diarrhea are the commonest presentations for infants proved to have cow milk allergy with CoMiSS score and elimination rechallenge test, where constipation is the least common presentation for those infants.
Similar content being viewed by others
Background
Cow’s milk protein (CMP) is the leading cause of food allergy in children younger than 3 years [1, 2]. According to a recent meta-analysis, the prevalence of cow’s milk protein allergy (CMPA) was 6% throughout life. Additionally, the rate of CMPA prevalence defined by the Cow milk protein reintroduction challenge was 0.6% [3]. Earlier reports estimated an incidence of 2–3% in the infancy period [4]. An Egyptian study was conducted in Damietta Governorate, and it showed that the frequency of CMPA in the first 2 years of life was 3.4%, as confirmed by the positive food elimination and oral food challenge (OFC) tests [5].
Infants with CMPA may experience a range of symptoms from mild to severe when exposed to CMP. The IgE-mediated immune system is more likely to be involved in immediate (early) reactions than delayed (late), which might take up to 48 h or even a week to develop after the allergen consumption. The latter could possibly involve immune systems that are not IgE-mediated. The same patient may experience both immediate and delayed reactions to the same allergen. Infants may experience a range of symptoms from mild to severe when exposed to CMPA. The IgE-mediated immune system is more likely to be involved in immediate (early) reactions than delayed (late), which might take up to 48 h or even a week to develop after the allergen consumption. The latter may also involve non-IgE-mediated immune mechanisms [6].
An OFC is followed by an elimination diet that lasts for 2 to 4 weeks in the standard diagnostic procedure for CMPA. In actual clinical practice, open challenges are typically seen as sufficient, particularly in infants and young children, even though the double-blind, placebo-controlled food challenge is the gold standard for the identification of a food allergy [7].
A tool called the “Cow’s Milk-related Symptom Score” has been developed to help primary healthcare providers identify cow’s milk-related symptoms in infants and young children since there are no other reliable diagnostic tests besides a food challenge with CM protein in infants doubtful of suffering from CMPA. It might improve one’s capacity to identify symptoms connected to sensitivity to the protein in cow milk. This tool will support good decision-making and effective management. It would be preferred by the parents because it will avoid both overdiagnosis and underdiagnosis and will also limit the infant’s suffering and parental disquiet. A too-late diagnosis of CMPA has an undesirable effect on the physical development of children [8, 9].
The Cow’s Milk-related Symptom Score (CoMiSS) measures a variety of symptoms, including general, dermatological, gastrointestinal, and respiratory aspects. It can also be adapted to assess and quantify the response of symptoms during therapeutic therapies. The CoMiSS instrument scores range from 0 to 33. CoMiSS cutoff (≥12) provides high sensitivity around 80–90% and moderate specificity in the range of 60–70% with AUC >0.75 to pick up the diagnosis of cow milk protein allergy [10, 11].
The CoMiSS score has shown to be a reliable instrument for raising primary healthcare providers’ awareness of more symptoms that could be caused by cow’s milk. The results do indicate that a CoMiSS of greater than 12 would be a reasonable cut-off point to identify infants who are exhibiting symptoms associated to cow’s milk. The drop in score to 6 or below was also connected to the response to a diet devoid of cow’s milk. The findings of the meta-analysis supported the hypothesis that CoMiSS may be a very sensitive and specific awareness tool for healthcare professionals to recognize infants who may be exhibiting symptoms associated with cow’s milk. The utility of the score as a diagnostic tool still requires confirmation through a validation study [10, 12].
Methods
This study is a cross-sectional study conducted at University Children’s Hospital, from January 1, 2020, to December 31, 2020. Forty infants less than 1 year of age were included in our study (28 males and 12 females) who presented to the gastroenterology and nutrition unit complaining of recurrent or persistent gastrointestinal symptoms.
This study is approved by the ethical review board of the faculty of medicine (IRB no: 17100593). Infants who met the selection criteria of the study were invited to participate. Parental consent from the caregiver of every infant that participates in this research was taken.
All the infants that participated were subjected to the following:
-
1.
A detailed history that includes detailed nutritional history, family history of allergic diseases, and detailed analysis of gastrointestinal complaints
-
2.
A thorough clinical examination.
-
3.
CoMiSS scoring, with the use of Bristol stool chart showing the seven categories of stool [10]. Infants with a CoMiSS of more than 12 points were included in our study.
-
4.
A food challenge test was done for suspected cases. An elimination diet was implemented for those infants for 4 weeks; then, after a symptomatic improvement, these infants undergo an OFC to confirm the diagnosis.
Statistical analysis
The data were analyzed using Statistical Package for the Social Sciences (SPSS) software program (version 26).
-
The qualitative variables are recorded as frequencies and percentages that are compared via the chi-square test.
-
The quantitative measure is displayed in the form of the mean value ± standard deviation (SD) and is compared via Student’s t test. A P value of less than 0.05 will be treated as statistically significant.
Results
There was a highly significant difference between infant sociodemographic characteristics. As regards the age at presentation, most of our studied infants started to complain and presented before 6 months of age (P = 0.0077 and <0.0001, respectively). The male gender was significantly higher than the female (P = 0.0004). Moreover, CMPA was more prevalent among infants with positive consanguinity (P = 0.0019). Thirty-three (82.5%) infants with a family history of allergic diseases have CMPA (P < 0.0001), as shown in Table 1.
Table 2 and Fig. 1 show that the most frequently reported GI manifestations are regurgitation (92%), followed by diarrhea (80%), colic (75%), vomiting (67.5%), and the least common presentation was constipation (5%).
Table 3 shows that the type of feeding was significantly associated with the presence of CMPA. 67.5% of the studied cases were artificially fed infants, and 12.5% were breastfed infants (P < 0.0001). Twenty percent of infants were mixed-fed infants (P = 0.028).
Although only 20 infants had started complementary feeding, CMPA was observed in infants who began complementary food after 6 months more than those who began before 6 months (60 vs 40%, P= 0.076).
Discussion
Cow milk protein allergy is considered to be the most common type of food allergy in infancy and childhood. The challenging point is the absence of a specific test for an accurate diagnosis of CMPA. OFC, with the elimination of cow milk protein for 4 weeks and then reintroduction with meticulous observation for resolution of symptoms after elimination and recurrence after reintroduction is still the gold standard test for diagnosis of CMPA. Our study showed that sociodemographic characteristics were significantly associated with CMPA. The male gender was more affected by CMPA than females. This agreed with Selbuz et al. who reported a significant male predominance in the CMPA among the male group. This can probably be explained by a genetic predisposition. An X-linked recessive trait associated with the allergic disease would be more likely to be unmasked in males (XY) and could explain why food allergies in males are more common at a very young age [13].
Regarding the age of presentation, this study showed that CMPA was more common in infants less than 6 months of age. Infants usually presented with CMPA during the first few months of life. CMPA most probably occurs at the time of addition of feeding (whatever its type) and decreases up to 1 year of age. Breastfed infants are more liable to food protein-induced allergic proctocolitis [14], whereas food protein-induced enterocolitis syndrome commonly occurs with artificial feeding [15].
Moreover, consanguinity and positive family history of allergic diseases play a crucial role. Our study showed that the incidence of CMPA was higher in infants with positive consanguinity and positive family history of allergic diseases. This finding agreed with various studies that found that a family history of atopy was significant in cases with CMPA, and the risk of atopy increases if a parent or sibling has an atopic disease. Furthermore, if both parents are atopic, the risk is even higher [16, 17]. As we have discussed before, allergy is an X-linked recessive trait, so CMPA was more prevalent among our studied infants with positive consanguinity and family history of allergic diseases. This is specifically important in countries such as Egypt, where parental consanguinity is common. A recent study conducted in South Sinai (Egypt) showed that 21 to 33% of the married couples were relatives and rural settings showed higher rates than urban settings [18].
Regarding the frequency of GI manifestations, the most frequent was regurgitation, then comes diarrhea, colic, vomiting, and least common presentation was constipation. Our study came in line with Dominguez-Ortega et al. who demonstrated that the majority of affected children with CMPA had other symptoms involving one or more organ systems, usually the gastrointestinal tract and/or skin [10]. Maksoud et al. reported that infants with suspected CMPA usually present with GI manifestations [12]. Additionally, Selbuz et al. reported a significant difference in the clinical presentation between infants with CMPA(+) and (−), with 60.4% of CMPA(+) infants reporting more than 5 episodes of regurgitation per day, which suggests that the severity of regurgitation may be a factor in determining whether to test the infant for CMPA [13]. ESPGHAN GI Committee practical guidelines stated that dysphagia, frequent regurgitation, colic, abdominal pain, vomiting, anorexia, refusal of food, diarrhea (with or without malabsorption or protein loss due to enteropathy), and constipation with or without perianal rash are common but nonspecific GI signs of CMPA in infants and toddlers [9].
Breastfeeding remains to prove that it is the best type of infant feeding, its protective effect against CMPA was pronounced in our study, where infants who were artificially fed exceeded infants who were breastfed. Jakaitis & Denning also stated that infants who were fed breast milk were found to have a reduced incidence of allergic disease [14]. The short-chain fatty acid produced by the degradation of breast milk oligosaccharides by colonizing bacteria, which has a function in strengthening tight-junctions integrity, can be used to explain this protective action of breast milk against infectious diseases and atopic disorders [15, 16].
Meanwhile, exclusive breastfeeding was shown to be protective against CMPA. Our study clearly showed a clear difference between the time of introduction of complementary food and the occurrence of CMPA that was statistically significant. The protective effect of exclusive breastfeeding was highlighted in previous studies who also reported that the risk of Allergy to cow milk protein was reduced in exclusively breastfed infants [12, 17]. CMPA was observed in infants who began complementary food after 6 months of age in our studied cases. According to Du Toit et al. 2015 study “the Learning Early About Peanut study (LEAP)” and the Enquiring About Tolerance study results, we found an agreement with our findings [18,19,20]. The introduction of complementary foods between the ages of 4 and 6 months is the best time to reduce the incidence of allergy, as advised by the majority of international guidelines, including The American and European allergy expert committee guidelines, as both have suggested that early complementary food introduction may be protective against allergy [21, 22].
This study was conducted in one of the largest university hospitals in Upper Egypt, and during recruitment of our cases, we notice the marked extremes in the diagnosis of CMPA with clearly obvious over and under-diagnosis. Many cases were misdiagnosed to have CMPA based on clinical criteria of persistent or recurrent GI manifestations and sometimes depending on some investigations, that proved to be irrelevant in the diagnosis of CMPA, like the occult blood in stool, fecal calprotectin level in the stool, skin prick test, or serum IgE food panel. On other hand, many of our cases proved to have CMPA by OFC test were misdiagnosed as lactose intolerance, persistent gastroenteritis, dysentery, pyloric stenosis, GERD, functional constipation, or anal fissure. A high index of suspicion, proper application of CoMiSS, and OFC are the cornerstones for early diagnosis and management of CMPA.
Conclusion
The diagnosis of CMPA should be considered in infants with persistent or recurrent GI manifestations. Regurgitation and diarrhea are the commonest presentations for infants proved to have cow milk allergy with CoMiSS score and OFC test, where constipation is the least common presentation for those infants.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its additional file.
References
Van Boxstael S, Habib I, Jacxsens L et al (2013) Food safety issues in fresh produce: bacterial pathogens, viruses and pesticide residues indicated as major concerns by stakeholders in the fresh produce chain. Food Control 32:190–197
Guler N, Cokugras FC, Sapan N et al (2020) Diagnosis and management of cow’s milk protein allergy in Turkey: region-specific recommendations by an expert-panel. Allergol Immunopathol (Madr) 48:202–210
Kelly C, Gangur V (2009) Sex disparity in food allergy: evidence from the PubMed database. J Allergy (Cairo) 2009:159845
Mennini M, Fiocchi AG, Cafarotti A et al (2020) Food protein-induced allergic proctocolitis in infants: literature review and proposal of a management protocol. World Allergy Organ J 13:100471
Feuille E, Nowak-Węgrzyn A (2014) Definition, etiology, and diagnosis of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 14:222–228
Björkstén B (2005) Genetic and environmental risk factors for the development of food allergy. Curr Opin Allergy Clin Immunol 5:249–253
Mushtaq I, Cheema HA, Malik HS, Waheed N, Hashmi MA, Malik HS (2017) Causes of chronic non-infectious diarrhoea in infants less than 6 months of age: rarely recognized entities. J Ayub Med Coll Abbottabad 29:78–82
Yamamah G, Abdel-Raouf E, Talaat A, Saad-Hussein A, Hamamy H, Meguid NA (2013) Prevalence of consanguineous marriages in South Sinai, Egypt. J Biosoc Sci 45:31–39
Koletzko S, Niggemann B, Arató A et al (2012) Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr 55:221–229
Domínguez-Ortega G, Borrelli O, Meyer R et al (2014) Extraintestinal manifestations in children with gastrointestinal food allergy. J Pediatr Gastroenterol Nutr 59:210–214
Vandenplas Y, Mukherjee R, Dupont C, Eigenmann P, Høst A, Kuitunen M, Ribes-Koninkx C, Shah N, Szajewska H, von Berg A, Heine RG, Zhao Z-Y (2018) Protocol for the validation of sensitivity and specificity of the Cow’s Milkrelated Symptom Score (CoMiSS) against open food challenge in a singleblinded, prospective, multicentre trial in infants. BMJ Open 8:e019968. https://doi.org/10.1136/bmjopen-2017-019968
Maksoud HMA, Al Seheimy LAF, Hassan KAG, Salem MF, Elmahdy EAM (2019) Frequency of cow milk protein allergy in children during the first 2 years of life in Damietta Governorate. Al-Azhar Assiut Med J 17:86
Selbuz SK, Altuntaş C, Kansu A et al (2020) Assessment fo cows milk-related symptom scoring awareness tool in young Turkish children. J Paediatr Child Health 56:1799–1805
Jakaitis BM, Denning PW (2014) Human breast milk and the gastrointestinal innate immune system. Clin Perinatol 41:423–435
Gao Y, Davis B, Zhu W, Zheng N, Meng D, Walker WA (2021) Short-chain fatty acid butyrate, a breast milk metabolite, enhances immature intestinal barrier function genes in response to inflammation in vitro and in vivo. Am J Physiol Gastrointest Liver Physiol 320:G521–G530
Ríos-Covián D, Ruas-Madiedo P, Margolles A, Gueimonde M, De Los Reyes-Gavilán CG, Salazar N (2016) Intestinal short chain fatty acids and their link with diet and human health. Front Microbiol 7:185
El Desouky AI, Anany HG, Mohammed ISI (2021) Assessment of CoMiSS among children with Cow’s milk allergy at Zagazig University Hospital. Egypt J Hosp Med 83:838–843
Logan K, Flohr C, Lack G, Perkin M (2011) The EAT Study-early introduction of allergenic foods to induce tolerance in infants. Clin Exp Allergy 41:1859–1860
Rosário FN (2015) Early introduction of food to prevent food allergy. The LEAP study (Learning Early about Peanut). Rev Paul Pediatr 33:493–494
Perkin MR, Logan K, Marrs T et al (2016) Enquiring About Tolerance (EAT) study: feasibility of an early allergenic food introduction regimen. J Allergy Clin Immunol 137:1477–1486 e8
Fleischer DM, Spergel JM, Assa’ad AH, Pongracic JA (2013) Primary prevention of allergic disease through nutritional interventions. J Allergy Clin Immunol Pract 1:29–36
Greer FR, Sicherer SH, Burks AW, Committee on Nutrition, Section on Allergy and Immunology (2019) The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of allergenic complementary foods. Pediatrics 143:e20190281
Acknowledgements
None
Funding
The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
Osama M. El-Asheer, Amira El-Gazzar, and Farouk Hassanein designed the study. Osama M. El-Asheer and Caroline M. Zakaria shared in the literature search, interpreted the data, and wrote the manuscript. Amira F. El-Gazzar did the statistical analysis and shared in the literature search and writing. Khalil A. Mohamed shared in writing and publication. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Faculty of Medicine, Assiut University (IRB no: 17100593). Written informed consent was taken from parents with an explanation of the benefits of the study, risks expected, and suggested treatment for each case.
Consent for publication
Infants who met the selection criteria of the study were invited to participate. Parental consent from the caregiver of every infant that participates in this research was taken.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Asheer, O.M., El-Gazzar, A.F., Zakaria, C.M. et al. Frequency of gastrointestinal manifestations among infants with cow’s milk protein allergy, Egypt. Egypt Pediatric Association Gaz 70, 34 (2022). https://doi.org/10.1186/s43054-022-00128-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-022-00128-9