Abstract
The incidence of button battery ingestion in children less than 6 years, from year 1985 to 2019 was 59,000 and it is still a clinical challenge for pediatricians. Objects which are commonly ingested are large amounts of food, coins, toy parts, jewels, batteries, sharp materials and non-metallic sharp objects. It is an increased incidence of mortality and morbidity due to button battery ingestion, compared to accidental ingestion of other objects, due to its small size, and because of its potent source of energy. A literature search was carried out to evaluate the challenges in diagnosing, treatment, and follow-up of button battery ingested cases in children. A total of 36 original articles were included for the review.
Conclusions: Button batteries can quickly cause severe damage to the mucosal lining of the GI tract. Esophageal button batteries require emergency removal because they can cause serious complications leading to hemorrhage, and death. In children, where the button battery has passed the esophagus watchful management should be made. In the majority of cases, the button batteries with a diameter less than 2 cm lodged in the stomach will pass spontaneously with no complications. However, asymptomatic children may be followed up with X-rays to assess progression up to 10–14 days after ingestion. Endoscopic or surgical removal may be required to prevent intestinal perforation with peritonitis. Symptomatic children will always need a consultation with a pediatric surgeon for surgery no matter where the button battery is placed in the GI tract. Developing countries shall adopt surveillance and reporting systems for BBI ingestion and related complications and it is recommended as essential to have management protocols in place for button batteries ingestion.
Similar content being viewed by others
Background
Foreign body (FB) ingestion is a clinical challenge for pediatricians. In 2019, the ingestion of button batteries is more than three times higher than the cases reported in 1985 with three times higher of major complications or death [1]. American Association of Poison Control Centers reported that more than 110,000 cases were reported in children less than 5 years of age [2]. By a retrospective study of people who were admitted due to foreign body ingestion, Cheng W et al. (1999) identified that foreign body ingestion is predominant in preschool toddlers, with a mean age of 3 years and 8 months old [3]. Khorana et al. (2019) in their retrospective study noted it was common in children with a mean age of 43.5 months [4] Objects which were commonly ingested are large amounts of food, coins (most common), toy parts, jewels, batteries, sharp materials like pins, needles, non-metallic sharp objects such as fish or chicken bone [3,4,5]. The incidence was more common in boys compared to girls. About 10% of ingested foreign bodies usually get lodged in the gastrointestinal tract [6, 7], the upper third of the esophagus, or more specifically the post-cricoids region, followed by retropharyngeal spaces [4].
Litovitz et al. reported that the incidence of button battery ingestion in children less than 6 years, from 1985 to 2019 was 59,000 [8]. In a retrospective study, Krom et al. (2018) identified that there is an increased incidence of mortality and morbidity due to button battery ingestion vs. accidental ingestion of other objects, challenges posed due to its small size, and because of its potent source of energy [9]. The lesions due to the button battery were usually located at the esophagus, by a battery that was either 20mm or bigger [10]. We can also add here the most common locations of the ingested batteries are the esophagus, stomach, and intestines.
The leakage of an alkaline electrolyte, the generation of an external current that causes electrolysis of tissue fluids, and pressure necrosis have been implicated in battery-induced tissue injuries [9, 11, 12]. The generation of hydroxide through electrolysis is thought to be the most important mechanism.
We want to report this case of large-button battery ingestion in the pediatric age to raise awareness of the dangerous complications that may arise from these accidental events. Button battery ingestions in childhood are very frequent nowadays and the importance of timely diagnosis, management, and follow-up is essential.
We aim to highlight the need for protocols to be in place and follow, especially in developing countries where these protocols are missing.
Case report
We are introducing the case of a 3-year-old boy who was presented to our outpatient clinic by both his parents, after their suspicions that the child could have ingested a button battery approximately 40 min before the time of presentation. The child at the time of presentation was hemodynamically stable and not in distress. He presented in a good overall health condition, had no evidence of stridor or hoarseness, and was playful. A physical examination was made and the child assessment was done. Immediately, the child was referred to the Emergency Department for further evaluation and to have a chest and abdominal radiograph done.
In his previous medical history, the child had a history of bronchiolitis but was otherwise healthy. Upon questioning, the father reported that the child was playing with his toy that contained a button battery and a few minutes later he noticed the battery was missing.
After doing his chest radiograph in the emergency room, we noticed the presence of a round metallic density over the topography of the stomach showing regular contour (Fig. 1). The lung fields appeared clear.
Because of the placement of the button battery at the time of presentation, and non-having the possibility of endoscopic retrieving of the button battery, the decision of a watchful waiting of the child was made. The parents were counseled to observe and report any symptoms, i.e abdominal pain, bloody stools, vomiting, nausea, fever immediately to the doctor that was following the case. Twelve hours later, the child was followed up and a 2nd abdominal radiograph was done to make sure the foreign body had passed the pyloric part of the stomach (Fig. 2). The child continued to be in good health and no symptoms were reported.
Five hours after the 2nd abdominal radiograph, the foreign body was found by the parents in the child’s stools and was confirmed to be a 20-mm button battery (Fig. 3).
Discussions
According to the National Poison Data System Reports, results show that in 2019 the ingestion of button batteries is more than three times higher than the cases reported in 1985 with three times higher of major complications or death [1]. This might be related to the advancement of technology and more electronic devices/toys working with button batteries nowadays. As of the year 2019, a total of 59,751 button battery ingestion is reported in children less than 6 years old. The most common sources of button batteries are toys, hearing aids, lights, remote controls, etc [1]. Button batteries are the second most frequently ingested foreign bodies, secondary to the coins [5].
Watchful management has been reported earlier. All button cells that have reached the stomach will be passed spontaneously without any symptoms or complications, no vomiting should be induced giving emetics [9,10,11,12,13] and no hospitalization is needed if the cell has reached the stomach [13]. According to the National Capital Poison Center Button Battery Ingestion Triage and Treatment Guideline if the child is asymptomatic, has passed esophageal stricture, and is lodged in the stomach, the patient can be managed at home with a normal diet and normal activity. Parents should confirm battery passage through stools inspection. If no passage is observed, an abdominal XR should be repeated in 10–14 days. If a patient is symptomatic of bloody stools, the battery should be removed either with endoscopy or surgically [1]. The type and voltage of the battery, the location, size, the patient’s age, symptoms, or complications should be considered every time before deciding whether endoscopy is required to remove a button battery from the stomach. If a child has ingested a lithium battery, urgent endoscopic removal is important to prevent complications. Endoscopic removal is recommended even if the child is asymptomatic children and the lithium battery is smaller than 2 cm in these cases [14]. Usually, button batteries with a diameter <2 cm located in the stomach will pass spontaneously with no complications. However, it is recommended to prompt removal of any battery with a diameter less than 2 cm that stayed too long in the pylorus or duodenum due to concern of increased risk of perforation [15]. The guidelines have been revised many times through the years [14]. Parents should be attentive to supervise their children because 61.8% of ingested batteries by children were obtained from different products [8].
The first case of a button battery ingestion (BBI) was reported in 1977 in a child swallowing camera battery logged on the proximal esophagus [16]. Foreign body (FB) ingestion is prevalent in children, while in recent years there is a steep rise in the number of debilitating or fatal battery ingestions in children [8, 17, 18]. Less than 2% of the foreign bodies ingested by children are reported to be button batteries, with a peak incidence between the age group of 6 months-3 years [19, 20]. This condition is presumably a life-threatening medical emergency requiring prompt medical intervention, especially lodgment of BBI in the esophagus. Button batteries (BB) being common domiciliary items with easy access to the pediatric population, possibly lead to significant morbidity and mortality on ingestions [17, 21, 22]. The rate of significant complications and death resulting from BBI has increased almost 7-fold [23]. Injury can occur rapidly and children can be with or without symptoms until catastrophic injuries develop over a period of hours or days [24]. BBs are able to create a local tissue pH environment of 10 to 13 inducing liquefactive necrosis at the negative pole. This injury can progress even after removal [25]. Although button batteries have different sizes and shapes and also discrete chemical profiles, all those might cause significant injury when placed in children’s esophagus [25]. The latest data analyzed from 1995 to 2019 regarding the incidence of BB ingestion, has reported a disproportionate surge in BBI from 0.14% to 10.46 %, with nearly 30% among these BBI requiring hospitalization and 7.5% with major complications or deaths [26].
Presentation
The symptoms during the initial presentation can range from being completely asymptomatic to being fatal. Unfortunately, patients may present with vague viral-like symptoms [25], dysphagia, odynophagia, fever, cough, or gastrointestinal illness with vomiting, feeding difficulty, stridor, and choking [8, 27]. Generally, BB ingestions are unwitnessed and clinicians find it difficult to get details regarding the battery. Infants and toddlers may also present with dyspnea, drooling, irritability, and anorexia. Older children may be able to articulate symptoms such as throat, chest, or abdominal pain and provide a FB ingestion history. After the button battery is ingested it can generate hydroxide ions at the negative pole. The accumulation of hydroxide ions can produce a local alkaline corrosive injury causing tissue liquefaction and necrosis [28]. Corrosive injury can happen as soon as 2 h of lodgment. Patients or parents shall be carefully asked regarding details of the battery ingested. It is important to know the number, type, charge state; time of ingestion, magnet co-ingestion, and past medical history of esophageal pathology or previous surgery [1, 28]. The National Capital Poison Center (NCPC) guidelines recommended forethought of diagnosis of BBI for children presenting with symptoms of wheezing, regurgitation/vomiting, dysphagia, loss of appetite, aphasia, dysphagia, chest discomfort, coughing, choking, or gagging with eating or drinking and possibly with respiratory distress [9, 29]. The negative battery pole can cause the most severe, necrotic injury. Unexplained nasal, ear, rectal, vaginal, or eye discharge/bleeding are possible complications, depending on the site of lodgement [28, 30].
Diagnosis
Button battery ingestions are classified among the most dangerous foreign bodies encountered in pediatrics. To differentiate from coin ingestion and other foreign bodies, these patients undergo anteroposterior and lateral X-ray films of the chest and airway and look for a double ring or halo sign to distinguish it from a coin [1, 24, 31]. Double-rim or halo-effect on AP radiograph and step-off on the lateral view can be diagnostic for BBI. Careful examination of these films for the halo sign, and the step-off between the positive and negative nodes of BBs, should be performed to help with the diagnosis. If a BB is identified, the orientation of the negative pole should be noted, cause there is most likely to occur a serious injury. A specialized handheld metal detector device is under potential consideration for the detection of BB, especially for children with nonspecific symptoms of viral illness, as a ubiquitous triage screening tool to minimize exposure to XRs [25, 26].
Management
Timely endoscopic removal is the gold standard of treatment in BBI. Interdisciplinary and coordinated care approach according to medical teams of ED, pediatric surgery, otolaryngology, anesthesia, pediatric gastroenterology, radiology, and cardiothoracic surgery physician is a strategy to successful management of BBIs [1, 23, 24]. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition recommend the removal of batteries in the esophagus within 2 h of ingestion endoscopically [31, 32].
Complications
The ongoing progression of injury due to BBI ingestion that can occur even after removal might place patients at risk of the catastrophic aorto-esophageal fistula or other severe sequelae of perforation, bleeding, and stricture. There is a diverse range of reported complications i.e esophageal stenosis or perforation, tracheo-esophageal fistula, mediastinitis, spondylodiscitis, intestinal perforation with peritonitis, vocal cord paresis and paralysis, cardiovascular and respiratory failure, pneumothorax, vascular fistula leading to hemorrhage, pneumoperitoneum, anterior spinal artery syndrome with bilateral lower extremity paralysis, and death [1, 25, 26]. Complications of BBI lodged in the esophagus included mucosal burns, perforations, stricture, vocal cord paralysis, formation of aorto-esophageal fistula, major hemorrhage & death [31, 33]. Most deaths reported due to BBI are possibly attributed to catastrophic hemorrhage secondary to the development of aorto-enteric fistula. According to the NCPC retrospective study, 12.6% of children younger than 6 years old who ingested a 20-mm diameter lithium BB developed a major complicatio n[24, 31]. It is crucial to anticipate, promptly identify, and manage all possible serious complications secondary to BBI.
Prevention approach
Along With Health Care Providers, Government and industry commitments were vital for the implementation of control measures at various hierarchical levels to prevent complications of BBI and serious sequelae.
Advocacy
The National Button Battery Task Force has put in place prevention strategies such as educational safety outreach campaigns, warning labels, and child-resistant packaging changes. Governmental regulation and industry reforms are solutions to curb the amount of BBI along with taking the edge of complications secondary to BBI [25].
Industrial innovations
Major BB industrial companies such as Energizer and Duracell have added child-resistant double packaging also added warning label stickers to keep BBs away from children. Duracell has released three lithium BBs (CR2016, CR2025, CR2032) that are covered by a nontoxic bitter coating trying to help prevent accidental ingestions in children [34].
Technological advancements
Introduction of composite coating to BB has emerged as a unique design alternate option to prevent injuries especially deterrent of the hydrolysis reaction, subsequent liquefaction tissue necrosis. This might prove a long-term solution to the elimination of complications secondary to BBI [24, 35].
Surveillance and monitoring
National capital poison center has introduced the National Battery Ingestion Hotline at 800-498-8666 to provide immediate recommendation and formulation of the Battery Statistics repository from the National Poison Data System (NPDS) resources. To effectively mitigate injuries secondary to BBI, a formalized, multi-disciplinary national task force was established in 2012 in the US, inclusive of members of the American Broncho-Esophagological Association (ABEA), American Academy of Pediatrics (AAP), American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS), American College of Surgeons (ACS), American Society of Pediatric Otolaryngology (ASPO), and representatives from industry, government, poison control, and public health with a multipronged approach to address outreach and education of the medical and non-medical community, secure button battery compartment design, effective electronic product, and button battery warning labels and button battery packaging [1, 24].
Reporting of BB injuries anonymously through the Global Injury Research Collaborative is made convenient and centralized through a user-friendly smartphone iOS/App Store and Android/GooglePlay application called the “GIRC App” [25]. Developing countries shall adopt surveillance and reporting systems for BBI ingestion and related outcomes [36].
Conclusions
Button batteries can quickly cause severe damage to the mucosal lining of the GI tract. Esophageal button batteries require emergency removal because they can cause serious complications. The most common and serious complications include esophageal perforation, mediastinitis, trachea-esophageal fistula, cardiovascular and respiratory failure, stenosis, intestinal perforation with peritonitis, pneumothorax, vascular fistula leading to acute hemorrhage and death. In children, where the button battery has passed the esophagus watchful management should be made. In the majority of cases, the button batteries with a diameter less than 2 cm lodged in the stomach will pass spontaneously with no complications. However, asymptomatic children may be followed up with X-rays to assess progression up to 10–14 days after ingestion. Only in a few children, endoscopic or surgical removal may be required to prevent intestinal perforation with peritonitis. Symptomatic children will always need a consultation with a pediatric surgeon for surgery no matter where the button battery is placed in the GI tract. Developing countries shall adopt surveillance and reporting systems for BBI ingestion and related complications and it is recommended as essential to have management protocols in place for button batteries ingestion.
Availability of data and materials
Not applicable.
Abbreviations
- FB:
-
Foreign body
- NCPC:
-
National Capital Poison Center
- BBI:
-
Button battery ingestion
- BB:
-
Button batteries
- ABEA:
-
American Broncho-Esophagological Association
- AAP:
-
American Academy of Pediatrics
- AAO-HNS:
-
American Academy of Otolaryngology-Head and Neck Surgery
- ACS:
-
American College of Surgeons
- ASPO:
-
American Society of Pediatric Otolaryngology
References
https://www.poison.org/battery/stats. Accessed on May 2021.
Lee JK (2018) Foreign Body Ingestion in Children. Clin Endosc 2018;51(2): 129-136. https://www.e-ce.org/journal/view.php?doi=10.5946/ce.2018.039
Cheng W, Tam PK (1999) Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg. 34(10):1472–1476. https://doi.org/10.1016/s0022-3468(99)90106-9
Khorana J, Tantivit Y et al (2019) Foreign Body Ingestion in paediatrics: Distribution, Management and Complications. Medicina. https://doi.org/10.3390/medicina55100686
Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y (2001) Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 160(8):468-72. doi: 10.1007/s004310100788. PMID: 11548183
Alexander WJ, Kadish JA, Dunbar JS (1969) Ingested foreign bodies in children. Prog Pediatr Radiol 2:256–285
Panieri E, Bass DH (1995) The management of ingested foreign bodies in children--a review of 663 cases. Eur J Emerg Med. 2(2):83–87. https://doi.org/10.1097/00063110-199506000-00005
Litovitz T, Whitaker N (2010) ClarkL, White NC, Marsolek M. Emerging battery ingestion hazard: clinical implications. Paediatrics 125(6):1168–1177 Epub 2010 May 24
Krom H, Visser M, Hulst JM et al (2018) Serious complications after button battery ingestion in children. Eur J Pediatr 177:1063–1070. https://doi.org/10.1007/s00431-018-3154-6
Lahmar J, Célérier C, Garabédian EN, et al. (2018) Esophageal lesions following button-battery ingestion in children: Analysis of causes and proposals for preventive measures. Eur Ann Otorhinolaryngol Head Neck Dis. 135(2):91-94. doi: 10.1016/j.anorl.2017.09.004. Epub 2017 Oct 18. PMID: 29054752.
Tanaka J, Yamashita M, Yamashita M (1998) Esophageal electrochemical burns due to button type lithium batteries in dogs. Vet Hum Toxicol. 40(4):193–196
Langkau JF, Noesges RA (1985) Esophageal burns from battery ingestion. Am J Emerg Med. 3(3):265
David TJ, Ferguson AP (1986) Management of children who have swallowed button batteries. Archives of disease in childhood. 1986 Apr;61(4):321. https://adc.bmj.com/content/archdischild/61/4/321.full.pdf, Accessed on May 2021.
Lee JH, Lee JH, Shim JO, Lee JH, Eun BL, Yoo KH (2016) Foreign Body Ingestion in Children: Should Button Batteries in the Stomach Be Urgently Removed? Pediatr Gastroenterol Hepatol Nutr. 19(1):20–28. https://doi.org/10.5223/pghn.2016.19.1.20
Seo JK (1999) Endoscopic management of gastrointestinal foreign bodies in children. Indian J Pediatr. 66(1 Suppl):S75–S80
Blatnik DS, Toohill RJ, Lehman RH Fatal complication from an alkaline battery foreign body in the esophagus. Annals of Otology, Rhinology & Laryngology, 86(5), 611-615.
Varga Á, Kovács T, Saxena AK (2018 Jun 1) Analysis of complications after button battery ingestion in children. Pediatric emergency care. 34(6):443–446
Majola NF, Kong VY, Mangray H, Govindasamy V, Laing GL, Clarke DL. An audit of ingested and aspirated foreign bodies in children at a university hospital in South Africa: The Pietermaritzburg experience. South African Medical Journal, 108(3), 205-209
Delport CD, Hodkinson PW, & Cheema B Investigation and management of foreign body ingestion in children at a major paediatric trauma unit in South Africa. African journal of emergency medicine, 5(4), 176-180
Timmers M, Snoek KG, Gregori D, Felix JF, van Dijk M, van As SA (2012 Dec 1) Foreign bodies in a pediatric emergency department in South Africa. Pediatric emergency care. 28(12):1348–1352
Hamilton JM, Schraff SA, Notrica DM (2009) Severe injuries from coin cell battery ingestions: 2 case reports. Journal of Pediatric Surgery 44(3):644–647
Soerdjbalie-Maikoe V, van Rijn RR (2010) A case of fatal coin battery ingestion in a 2-year-old child. Forensic Science International 198(1–3):e19–e22
Leinwand K, Brumbaugh DE, Kramer RE (2016) Button Battery Ingestion in Children: A Paradigm for Management of Severe Pediatric Foreign Body Ingestions. Gastrointestinal endoscopy clinics of North America 26(1):99–118. https://doi.org/10.1016/j.giec.2015.08.003
Jatana KR, Litovitz T, Reilly JS et al (2013) Pediatric button battery injuries: 2013 task force update. Int J Pediatr Otorhinolaryngol. 77(9):1392–1399. https://doi.org/10.1016/j.ijporl.2013.06.006
Sethia R, Gibbs H, Jacobs IN, Reilly JS, Rhoades K, Jatana KR (2021). Current management of button battery injuries. Laryngoscope Investigative Otolaryngology
Buttazzoni E, Gregori D, Paoli B et al (2015) Symptoms associated with button batteries injuries in children: an epidemiological review. Int J Pediatr Otorhinolaryngol. 79(12):2200–2207. https://doi.org/10.1016/j.ijporl.2015.10.003
Haddad N, Wilson JD, Fard D, Levi JR (2020 Jan) Pediatric button battery ingestion: Publication trends in the literature. American journal of otolaryngology. 22:102401
Ettyreddy AR, Georg MW, Chi DH, Gaines BA, Simons JP (2015) Button batteryinjuries in the pediatric aerodigestive tract. Ear Nose Throat J. 19(12):486–493. https://doi.org/10.1177/014556131509401207
Moral L, Serna JV, Castillo B (2010) Aspiración de pila de botón: caso único en la literatura médica. Arch Bronconeumol. 46:153–154. https://doi.org/10.1016/j.arbres.2009.09.006
Acosta Díaz HG, Trinidad Ruíz G, Pantoja Hernández CG, Samaniego B, Pando J, Rejas E (2013) Lesión bronquial por aspiración de una pila alcalina (pila de botón). An Pediatr. 79:267–268. https://doi.org/10.1016/j.anpedi.2012.10.014
Thabet MH, Basha WM, Askar S (2013 Jan) Button battery foreign bodies in children: hazards, management, and recommendations. BioMed research international. 1:2013
Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, Gibbons TE, Pall H, Sahn B, McOmber M, Zacur G, Friedlander J, Quiros AJ, Fishman DS, Mamula P (2015) North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Endoscopy Committee.Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 60(4):562–574
Banerjee R, Rao GV, Sriram PV, Reddy KS, Nageshwar Reddy D (2005 Feb) Button battery ingestion. Indian J Pediatr. 72(2):173–174
https://www.duracell.com/en-us/techlibrary/safety-data-sheets/ Accessed on July 2021.
Jatana KR, Barron CL, Jacobs IN (2019) Initial clinical application of tissue pH neutralization after esophageal button battery removal in children. The Laryngoscope 129(8):1772–1776
https://www.facs.org/-/media/files/clinical-congress/2019/cc2019_program_planner.ashx Accessed on July 2021.
Acknowledgements
We want to thank our host institution for the support.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
Study conception and design of the work: OA and AA. Analysis and interpretation of data were performed by OA, AA, NH, and KA. Drafting of the manuscript: OA, AA, NH, and KA. Critical revision: OA and AA. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed written consent from the child’s parent for publication was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
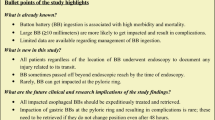
Summary key points
• Button batteries are one of the most common foreign bodies ingested in children less than 6 years old.
• There is an increased incidence of mortality and morbidity due to button battery ingestion, compared to accidental ingestion of other objects, because of its potent source of energy.
• Esophageal button batteries require emergency removal because they can cause serious complications.
• If button battery has passed the esophagus, a watchful management should be made.
• In developing counties, there is a need for protocols to be in place.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agolli, O., Agolli, A., Hange, N. et al. Therapeutic dilemma and clinical issues in management of the button battery ingestion: a case report and literature review. Egypt Pediatric Association Gaz 69, 37 (2021). https://doi.org/10.1186/s43054-021-00084-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-021-00084-w