Abstract
Objectives
Naltrexone prophylaxis is a well-established treatment for opioid use disorder. Our study aimed to track patients on naltrexone and investigate the factors predictive of retention.
Materials and methods
The study comprised 100 participants initiated on naltrexone, who underwent a 12-week follow-up. We analyzed a range of socio-demographic and clinical variables at 04 and 12 weeks to compare those who remained in treatment program with those who experienced relapse.
Results
The results revealed a predominantly young, unmarried, male, rural-dwelling sample with heroin as the primary opioid. Intravenous use was common (75%), with 57% of the participants exhibiting positive serology results for infections by hepatitis C (HCV), hepatitis B (HBV), and/or human immunodeficiency virus (HIV), and a significant proportion initiating opioids before the age of 20 (31%). The retention rates at 04 and 12 weeks were 83% and 64%, respectively. Several socio-clinical factors including age of initiation of use, rural residence, and comorbid psychiatric illness significantly influenced retention at 04 and 12 weeks.
Conclusion
The findings highlight the importance of tailored interventions that take into consideration the age, residence, socio-economic status, and psychiatric comorbidity to enhance retention rates. Identifying these factors can help improve the effectiveness of treatment programs and promote sustained recovery efforts.
Similar content being viewed by others
Introduction
Substance use is a behavior characterized by an individual experiencing a strong psychological and/or physiological desire to continue using a substance despite facing adversities, leading to prioritization of obtaining and using the substance over important aspects of life [1]. Substance use disorder (SUD) presents as a chronic illness marked by recurring patterns of recovery and relapse, frequent non-attendance at appointments, and untimely withdrawal from engagement, resulting in a progressive decline in the holistic health of both the patients and their familial support systems [2,3,4]. Opioid use disorder (OUD) is a significant public health issue, with fatal overdoses being a major concern. Other causes of mortality include suicide and blood-borne infections like hepatitis C (HCV), hepatitis B (HBV), and acquired immunodeficiency syndrome caused by HIV [5]. Recent studies estimate that globally, 40.5 million people are dependent on opioids, with approximately 109,500 deaths occuring due to opioid overdose, annually. [6, 7].
Long-term management of OUD involves maintenance therapy, which utilizes medications like buprenorphine, methadone, or naltrexone (NTX) [8]. Research indicates that maintenance treatment offers advantages over alternative options such as detoxification, residential programs, behavioral therapies, or no long-term treatment [9, 10]. While buprenorphine and methadone have been the primary choices, there is a growing interest in examining the efficacy of alternative approaches such as NTX and slow-release oral morphine [11,12,13,14]. Naltrexone, an antagonist at mu-opioid receptors, was approved by the US FDA in 1984 for preventing relapse in OUD and can be administered orally or via intramuscular (IM) injection. It lacks reinforcing effects, making it suitable for individuals pursuing complete abstinence and an opioid-free lifestyle [15,16,17].
The concept of treatment retention serves a dual purpose, functioning both as a process and an outcome measure [18]. The assessment of treatment retention holds paramount importance across various domains: it facilitates the evaluation of treatment effectiveness, enables the optimization of interventions, assists in the efficient allocation of resources, enhances patient satisfaction and adherence, improves healthcare practices, and ensures the maintenance of ethical standards in healthcare delivery. Despite the huge burden of opioid dependence in India, there remains a significant gap in understanding the factors that influence individuals to stay engaged in treatment programs. Furthermore, no study has been conducted within our population; this study was initiated to address this gap.
Materials and methods
This study was a hospital-based study, conducted at the drug addiction center of a tertiary care hospital which has an in-patient facility for individuals with SUD. The study had a fair representation of the population from the entire region and was longitudinal and prospective in design, conducted over a period of 18 months. Consecutive recruitment of 100 participants diagnosed with OUD was done from the out-patient and in-patient departments of the center. The diagnosis of OUD was done using DSM-5 criteria, and the diagnosis was confirmed by the in-charge psychiatrist of the OPD/IPD. The participants were assessed at three times during the study: at the time of entry into the study (on the day of starting NTx), at 04 weeks, and 12 weeks afterward. Individuals were interviewed when they were stable, not in intoxication/withdrawal. Written informed consent was obtained in the local understandable language, and rigorous measures were taken to maintain confidentiality. Participants were briefed about the purpose of the interview, and incomplete interviews were not considered. The inclusion criteria included (i) patients greater than 18 years of age, (ii) fulfilling the DSM-5 criteria for OUD, and those willing to participate in the study by providing written informed consent. The following participants were excluded: (i) those with acute intoxication, withdrawal, and/or delirium, (ii) those already on NTx; (iii) those having any contraindication to the use of NTx and those with a history of leprosy, tuberculosis, COPD, bronchial asthma, or severe liver disease.
Sample size
The sample size was determined using a formula with a 95% confidence interval, a 5% margin of error, and an anticipated prevalence of opioid use disorder based on previous studies, resulting in a calculated value of 80.
Study aims
-
(i)
To study the socio-demographic and clinical profile of patients initiated on oral Naltrexone.
-
(ii)
To determine the predictors of retention in patients on naltrexone at 04 and 12 weeks.
Operational definitions
-
a)
Opioid use disorder: Opioid use disorder (OUD) is defined as a problematic pattern of opioid use leading to clinically significant impairment or distress. Diagnosis requires meeting at least two of eleven outlined criteria within 12 months, with severity categorized as mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria) [19].
-
b)
Relapse:relapse was defined as the recurrence of opioid use after a period of abstinence or control [20].
Measures
The following instruments were utilized in the study:
-
a)
A semi-structured proforma was used to collect demographic data and clinical information on the age, residence, marital status, age of onset of use, duration of use, type of opioid, route of use, and serology status. At 04 and 12 weeks, the proforma also collected the side effect burden. This information was obtained through a semi-structured interview schedule.
-
b)
Kuppuswamys Socio-demographic Scale: It is a measurement tool that calculates a composite score based on the education and occupation of the head of the family, and the monthly income of the household. The scale categorizes groups into five distinct social classes: Upper (I), Upper Middle (II), Lower Middle (III), Upper Lower (IV), and Lower (V) socio-economic status [21, 22].
-
c)
The Mini-International Neuropsychiatric Interview is a structured diagnostic interview, with high reliability and validity, for DSM-5 and ICD-10 psychiatric disorders. It is designed to meet the need for a short and accurate structured psychiatric interview for multicenter clinical trials and epidemiological studies. This scale was used for the assessment of psychiatric comorbidities and all the diagnoses were confirmed by a consultant psychiatrist [23].
-
d)
Clinical Opioid Withdrawal Score (COWS): It is a clinician-administered instrument that rates 11 common opiate withdrawal signs or symptoms. The summed score of these items can be used to assess a patient's level of opiate withdrawal. This tool can be used in both inpatient and outpatient settings [24].
-
e)
Multidimensional Scale for Perceived Social Support (MDPSS): It is a 12-item questionnaire to identify an individual’s perceived level of social support with family, friends, and significant others. It is a Likert type of scale and has demonstrated good reliability and validity across diverse populations [25].
-
f)
Severity of Opioid Dependence Questionnaire (SODQ): It is a self-report assessment tool designed to measure the severity of opioid dependence in individuals, and comprises 14 items that assess various aspects of opioid dependence. It provides a quantitative measure of the severity. It has been widely used in both clinical and research settings and serves as a valuable tool [26].
Statistical analysis
Data was entered in Statistical Package for Social Sciences (SPSS) V27. Descriptive statistics was used for continuous variables and the chi-square and Fischer’s exact test were applied for categorical variables. Group differences in scores were compared on the chi-square test and the Student’s t-test. All p-values were two-sided, and p-value < 0.05 was considered statistically significant.
Results
Socio-demographic characteristics
The study sample consisted of 100 participants with a mean age of 23.45 ± 6.02 years. The majority of the participants were unmarried (79%), males (99%), from a rural background (55%), of middle socio-economic status (48%), employed (52%), and belonging to nuclear families (64%), as evident in Table 1.
Clinical characteristics
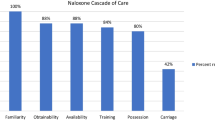
The primary opioid used by the participants was heroin, in 91 participants, accounting for 91% of the sample. Among all study participants, 09 individuals had a history of use of pharmaceutical opioids. Specifically, 03 patients exclusively used tramadol, 02 used tapentadol, and 04 used both tramadol and tapentadol. Seventy-five percent of the study population had intravenous as the major route of administration and 57% had positive serology tests for HCV, HBV, and/or HIV. Twenty-one percent of the sample had a history of comorbid medical illness, with hypertension (6%), diabetes (3%), and seizure disorder (3%) observed among participants, while 25% had a history of comorbid psychiatric illnesses with MDD, ADHD, and personality disorders being the commonest, seen in 11%, 4%, and 4% of the sample, respectively. As is evident from Table 2, 31% of the individuals had a history of early initiation of opioid use, before the age of 20 years. Seventy-nine percent of the sample had a COWS score of 0 at the time of initiation of NTx. Severe dependence was seen in 56% of the study sample. Eighty-three percent of the participants were retained at 4 weeks and 64% at 12 weeks of oral naltrexone therapy.
Association of socio-clinical variables with retention at 4 weeks
Table 3 presents a comparison of socio-clinical variables between participants who were retained and those who experienced relapse at 4 weeks. The results indicate that socio-economic status (χ2 = 11.09, p-value < 0.01), residence (χ2 = 3.213, p-value = 0.07), and comorbid medical illness (χ2 = 12.59, p-value < 0.01) significantly influenced retention at 4 weeks. Additionally, participants who retained had a higher mean age (T = 2.060; CI = − 5.58, − 0.10; p-value = 0.04) and higher mean scores on MDPSS (T = − 5.420; CI = − 3.88, − 1.80; p-value < 0.01) than patients who experienced relapse.
Association of socio-clinical variables with retention at 12 weeks
An early age of initiation of opioid use (χ2 = 4.753, p-value = 0.03), rural residence (χ2 = 4.04, p-value = 0.06), lower socio-economic status (χ2 = 5.395, p-value = 0.04), comorbid medical illness, (χ2 = 10.85, p-value < 0.01), comorbid psychiatric illness (χ2 = 5.786, p-value < 0.01), serology for HCV/HBV/HIV (χ2 = 7.43, p-value < 0.01), comorbid substance use (χ2 = 2.952, p-value = 0.08) significantly influenced retention on univariate analysis, as can be seen in Table 4. A higher mean age (T = − 1.62; CI = − 4.07, 0.24; p-value = 0.08), higher MDPSS score (T = − 8.208; CI = − 3.67, − 2.24; p-value = 0.00), and a higher mean COWS score at baseline (T = − 2.192; CI = − 4.62, − 0.23; p-value = 0.03) favored retention at 12 weeks.
Discussion
Opioid dependence is a lifelong, chronic, relapsing, and remitting disorder. To keep these patients free from drugs, substantial therapeutic efforts are the need of the hour [27]. In general, treatment with methadone plays a critical role in the detoxification or maintenance of subjects with opioid dependence; however, methadone is not a perfect medicine, and some patients on methadone continue to abuse drugs and indulge in criminal activities [28]. Naltrexone is a long-acting opioid antagonist that is devoid of addiction and usually does not produce a sense of well-being. It is approved for use in the treatment of patients with opioid dependence [29]. Naltrexone is more suitable to prevent relapse in the category of patients in which poor compliance with treatment may have major consequences; these include health professionals, business executives, and individuals under legal supervision [30].
The present prospective study evaluated the retention rates and predictive factors (clinical and socio-demographic) for oral naltrexone in patients with opioid use disorder at a tertiary care teaching hospital in the northern part of the subcontinent. Studies have found variable results in medication compliance and retention rates with oral naltrexone [31].
Our study revealed several key findings: (a) predominant use of injection heroin, (b) high retention rates at 04 and 12 weeks with naltrexone, (c) an early age of initiation of opioid use, lower SES, comorbid psychiatric illness and high side effect rates affecting retention at 12 weeks, (d) no impact on retention at 4 and 12 weeks due to family type, residence, type of opioid, and severity of dependence or withdrawal.
The mean age of the participants was 23.45 years with a standard deviation of 6.02 years. The majority fell within the age range of 20 to 25 years, with only 6% being over 30 years old, consistent with findings from similar studies emphasizing the prevalence of substance use among early adults [32,33,34,35,36,37,38,39]. Almost all the participants were males, highlighting the challenges females face in treatment access due to lack of awareness and stigma. Studies have indicated that women face more difficulties in access to substance use treatment [33, 34]. The majority of participants were literate, unmarried, and living in nuclear families from rural areas, explained by the fact that Kashmir is predominantly rural and the sample primarily consisted of individuals in early adulthood, a demographic more likely to be educated. Additionally, living in nuclear families exposes individuals to increased life stresses without the support of extended family, potentially heightening vulnerability to substance use.
Early retention, at 04 weeks was seen in 83% of the patients with significant results in favor of various socio-demographic and clinical variables. Identification of these variables is important as this could help in the selection of suitable patients for long-term maintenance with naltrexone [40, 41]. Retention at 04 weeks was not significantly associated with occupation and marital status of the patient and serology status, comorbid psychiatric illness, type, and route of use of opioids, similar to results from other studies conducted [42,43,44]. However, rural residence, comorbid medical illness, and middle SES significantly impacted retention at 04 weeks. Participants with higher scores on the MDPSS scale also had a higher chance of retention.
There were many socio-clinical predictors significant on univariate analysis at 12 weeks, a later age of initiation, lower SES, and rural residence significantly predicted retention at 12 weeks. An early age of initiation of opioid use is associated with neurocognitive deficits including deficits in executive functions such as problem-solving, decision-making, and development of reward system and self-control, which could contribute to poorer retention [45]. It may be prudent to mention that such patients may benefit from more intensive treatment strategies, those aimed at assuring swift transition to and maintenance on naltrexone therapy [46].
Side effect score was predictive of retention at both 04 and 12 weeks, indicating that participants who develop side effects are more likely to relapse while on naltrexone. The most often reported adverse symptoms included nausea, abdominal pain, trouble sleeping, headaches, low energy, depressed mood, and palpitations [47]. It may thus be considered that patients continue taking clonidine and other complementary medicines during the initial weeks of treatment [46]. Good social support also predicted retention at 04 and 12 weeks, similar to results from past studies [32, 47]. Generally, it is considered that participants who receive supervised medication have longer retention to treatment and supervision is an aid in treatment retention.
The severity of opioid dependence and severity of withdrawal symptoms did not significantly influence retention at 04 and 12 weeks in our study with similar results from many other studies highlighting that naltrexone could be a good treatment option in patients with severe dependence and dismissing the myth that patients retain in long-term treatment for prevention of withdrawals only [42].
The presence of a comorbid psychiatric illness predicted retention at 12 weeks with significantly lower retention in patients with comorbid psychiatric illness, which could be because patients with dual diagnosis have poor social support and a lack of insight into their drug-seeking behavior, leading to a poorer follow-up and thus retention. Patients with a comorbid psychiatric illness have worse substance use outcomes and poorer psychosocial functioning than those without, stressing the need for mental health assessment and treatment for psychiatric conditions in patients undergoing pharmacotherapy for opioid use disorders [43]. The common psychiatric illnesses found included mood disorders, personality disorders, and ADHD. Comorbid psychiatric illnesses also leads to some degree of socio-occupational dysfunction and loss of follow-up, translating into poorer retention. Patients with comorbid substance use also had poorer retention to therapy; this is a well-known fact that people with dependence on multiple substances have poorer outcomes than the ones with single substance use.
Employment, marital status, and type of family were not found to be predictors of retention at 04 and 12 weeks. Studies have found that the retention rates were better among those who were employed, married, and living in a joint family type highlighting the possible role of family and spouse support in ensuring treatment adherence [48, 49]. However, our study failed to demonstrate such association.
Residence was also not found to be a predictor of retention at 12 weeks, a longer distance to the treatment center implies a longer time needed to commute to get prescription medicine which might act as a deterrent against follow-up. This scenario is true for rural settings in the subcontinent [50,51,52]. However, in the present study, distance of residence from the treatment center was not found to be predictive of retention at 12 weeks which could be because NTX is available at the treatment center and is provided for longer durations of time when required. Lower socio-economic status was found to be predictive of retention at 12 weeks but not 04 weeks.
The route of use and type of opioid used also did not impact retention significantly; however, positive serology status was found to be a positive predictor of retention at 12 weeks. Positive serology for HCV/HBV/HIV in opioid use has been strongly associated with impulsivity and the presence of high-risk behaviors like sharing of paraphernalia and unprotected sexual intercourse. Patients with impulsivity have higher chances of becoming non-compliant with therapy and relapse [17].
There is a need for a long-term follow-up study to assess sustained effectiveness in comparison with other treatments, and explore factors influencing retention. Studies should also focus on elucidation of underlying mechanisms of action and implementation to optimize real-world utilization, all aimed at enhancing treatment outcomes for OUD.
Strengths
The strengths of the current study lie in its high baseline completion rate, extensive assessment of heroin users, and comprehensive analysis of multiple and varied clinical and psychosocial predictors, offering valuable insights into retention on naltrexone treatment in this population.
Limitations
The assessment was conducted at a single center so the findings cannot be generalized to the community. The sample size was relatively small and cannot be considered representative of the entire North Indian population. Small sample sizes may also lead to type II errors and cause overestimation. The study design, although prospective, was a non-randomized one with the absence of a control arm; this could potentially lead to selection bias.
Conclusion
In conclusion, lower age of initiation (odds ratio = 4.3), lower socio-economic status (OR = 1.6), comorbid psychiatric illness (OR = 3.1), and additional substance use (OR = 5.2) were predictors for poor retention to naltrexone maintenance therapy in subjects with opioid use at 12 weeks of oral naltrexone therapy.
Availability of data and materials
The data sets used and analyzed during this study are available from the Corresponding Author upon reasonable request.
References
Volkow ND, Blanco C (2023) Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry 22(2):203–229. https://doi.org/10.1002/wps.21073. PMID:37159360;PMCID:PMC10168177
Fleury MJ, Djouini A, Huỳnh C, Tremblay J, Ferland F, Ménard JM, Belleville G (2016) Remission from substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend 168:293–306
Sliedrecht W, de Waart R, Witkiewitz K, Roozen HG (2019) Alcohol use disorder relapse factors: a systematic review. Psychiatry Res 278:97–15
Milward J, Lynskey M, Strang J (2014) Solving the problem of non-attendance in substance abuse services. Drug Alcohol Rev 33(6):625–636
Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M et al (2011) Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction 106(1):32–51
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P et al (2017) Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health 5(12):e1192–e1207
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL et al (2019) Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet 394(10208):1560–1579. https://doi.org/10.1016/S0140-6736(19)32229-9
Bisaga A, Mannelli P, Sullivan MA, Vosburg SK, Compton P, Woody GE, Kosten TR (2018) Antagonists in the medical management of opioid use disorders: Historical and existing treatment strategies. Am J Addict 27(3):177–187. https://doi.org/10.1111/ajad.12711. PMID:29596725;PMCID:PMC5900907
Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH et al (2020) Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open 3(2):e1920622. https://doi.org/10.1001/jamanetworkopen.2019.20622
Mittal ML, Jain S, Sun S, DeBeck K, Milloy MJ, Hayashi K et al (2019) Opioid agonist treatment and the process of injection drug use initiation. Drug Alcohol Depend 197:354–360
Dematteis M, Auriacombe M, D’Agnone O, Somaini L, Szerman N, Littlewood R et al (2017) Recommendations for buprenorphine and methadone therapy in opioid use disorder: a European consensus. Expert Opin Pharmacother 18(18):1987–1999
Kampman K, Jarvis M (2015) American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med 9(5):358–367
Klimas J, Gorfinkel L, Giacomuzzi SM, Ruckes C, Socias ME, Fairbairn N et al (2019) Slow-release oral morphine versus methadone for the treatment of opioid use disorder. BMJ Open 9(4):e025799. https://doi.org/10.1136/bmjopen-2018-025799
Jarvis BP, Holtyn AF, Subramaniam S, Tompkins DA, Oga EA, Bigelow GE et al (2018) Extended-release injectable naltrexone for opioid use disorder: a systematic review. Addiction 113(7):1188–1209
Shufman EN, Porat S, Witztum E, Gandacu D, Bar-Hamburger R, Ginath Y (1994) The efficacy of naltrexone in preventing reabuse of heroin after detoxification. Biol Psychiat 35(12):935–945
Krupitsky E, Zvartau E, Woody G (2010) Use of naltrexone to treat opioid addiction in a country in which methadone and buprenorphine are not available. Curr Psychiatry Rep 12:448–453
Cousins SJ, Radfar SR, Crèvecoeur-MacPhail D, Ang A, Darfler K, Rawson RA (2016) Predictors of continued use of extended-released naltrexone (XR-NTX) for opioid-dependence: an analysis of heroin and non-heroin opioid users in Los Angeles County. J Subst Abuse Treat 1(63):66–71
Chou CP, Hser YI, Anglin MD (1998) Interaction effects of client and treatment program characteristics on retention: an exploratory analysis using hierarchical linear models. Subst Use Misuse 33:2281–2301
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5, 5th edn. American Psychiatric Publishing, Washington, D.C.
Chalana H, Kundal T, Gupta V, Malhari AS (2016) Predictors of relapse after inpatient opioid detoxification during 1-year follow-up. J Addict. 2016:7620860. https://doi.org/10.1155/2016/7620860. Epub 2016 Sep 18. PMID: 27722007; PMCID: PMC5046044
Khairnar M, Wadgave U, Shimpi P (2017) Kuppuswamy’s Socio-Economic Status Scale: a revision of occupation and income criteria for 2016. Indian J Pediatr 84:3–6
Saleem SM (2018) Modified Kuppuswamy Scale updated for 2018. Indian J Med Res 7:435–436
Sheehan DV, Lecrubier Y, Sheehan KH et al (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–57
Wesson DR, Ling W (2003) The Clinical Opiate Withdrawal Scale (COWS). J Psychoactive Drugs 35(2):253–259. https://doi.org/10.1080/02791072.2003.10400007
Wongpakaran T, Wongpakaran N, Ruktrakul R (2011) Reliability and validity of the Multidimensional Scale of Perceived Social Support (MSPSS): Thai version. Clin Pract Epidemiol Ment Health 7:161–6. https://doi.org/10.2174/1745017901107010161. Epub 2011 Oct 26. PMID: 22114620; PMCID: PMC3219878
Burgess PM, Stripp AM, Pead J, Holman CP (1989) Severity of opiate dependence in an Australian sample: further validation of the SODQ. Br J Addict 84(12):1451–1459. https://doi.org/10.1111/j.1360-0443.1989.tb03926.x
McLellan AT, Lewis DC, O’Brien CP, Kleber HD (2000) Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 284(13):1689–1695
Rawson RA, McCann MJ, Hasson AJ, Ling W (2000) Addiction pharmacotherapy 2000: new options, new challenges. J Psychoactive Drugs 32(4):371–377
Lihi R, Yael D, Silviu B, Anat S, Marsha W, Stacy S, Shaul S, Miriam A, Einat P (2023) Stigma, and level of familiarity with opioid maintenance treatment (OMT) among specialist physicians in Israel. Harm Reduct J 20(1):134. https://doi.org/10.1186/s12954-023-00869-9. PMID:37715237;PMCID:PMC10503015
Heikman PK, Muhonen LH, Ojanperä IA (2017) Polydrug abuse among opioid maintenance treatment patients is related to inadequate dose of maintenance treatment medicine. BMC Psychiatry 17(1):245. https://doi.org/10.1186/s12888-017-1415-y. PMID:28683783;PMCID:PMC5501578
Edinoff AN, Nix CA, Orellana CV, StPierre SM, Crane EA, Bulloch BT, Cornett EM, Kozinn RL, Kaye AM, Murnane KS, Kaye AD (2021) Naltrexone implant for opioid use disorder. Neurol Int 14(1):49–61. https://doi.org/10.3390/neurolint14010004. PMID:35076607;PMCID:PMC8788412
Chaudhry ZA, Sultan J, Alam F (2012) Predictors for retention in treatment with a UK community-based naltrexone programme for opioid dependence. Psychiatrist 36(6):218–224. https://doi.org/10.1192/pb.bp.111.035063
Rather YH, Bashir W, Sheikh AA, Amin M, Zahgeer YA (2013) Socio-demographic and clinical profile of substance abusers attending a regional drug de-addiction centre in chronic conflict area: Kashmir India. Malays J Med Sci MJMS 20(3):31–38
Rather YH, Bhat FR, Malla AA, Zahoor M, Ali Massodi PA, Yousuf S (2021) Pattern and prevalence of substance use and dependence in two districts of Union Territory of Jammu & Kashmir: special focus on opioids. J Fam Med Prim Care 10(1):414–420
Farhat S, Hussain SS, Rather YH, Hussain SK (2015) Sociodemographic profile and pattern of opioid abuse among patients presenting to a de-addiction centre in tertiary care Hospital of Kashmir. J Basic Clin Pharm 6(3):94–97
Randhawa A, Brar MS, Kumari B, Chaudhary N (2020) Sociodemographic profile and pattern of substance abusers: a retrospective study to unveil the public health problem of Punjab. J Fam Med Prim Care 9(7):3338–3342
Majumder U, Das J, Barman SC, Ghosh J, Bhowmic BK (2021) Sociodemographic and clinical profile of drug treatment seekers attending the state psychiatric hospital and drug de-addiction center at Agartala, Tripura. Indian J Psychiatry 63(1):80
Jumade P, Kasbe A, Giri P (2016) Socio-demographic profile of male drug abusers residing in Mumbai city, Maharashtra, India. Int J Community Med Public Health 1:1115–1118
Kumar V, Nehra D, Kumar P, Sunila GR (2013) Prevalence and pattern of substance abuse: a study from de-addiction center. Delhi Psychiatry J 16:110–4
Chand P, Murthy P (2013) Short-term outcome of take-home prescriptions for opioid dependence: a clinic-based study. J Subst Use 18(2):108–118
Dayal P, Balhara YPS, Mishra AK (2016) An open label naturalistic study of predictors of retention and compliance to naltrexone maintenance treatment among patients with opioid dependence. J Subst Use 21(3):309–316
Shouan A, Ghosh A, Singh SM, Basu D, Mattoo SK (2021) Predictors of retention in the treatment for opioid dependence: a prospective, observational study from India. Indian J Psychiatry 63(4):355–365
Zhu Y, Mooney LJ, Yoo C, Evans EA, Kelleghan A, Saxon AJ, Curtis ME, Hser YI (2021) Psychiatric comorbidity and treatment outcomes in patients with opioid use disorder: results from a multisite trial of buprenorphine-naloxone and methadone. Drug Alcohol Depend 1(228):108996
Bhat BA, Dar SA, Hussain A (2019) Sociodemographic profile, pattern of opioid use, and clinical profile in patients with opioid use disorders attending the de-addiction center of a tertiary care hospital in North India. Indian J Soc Psychiatry 35:173–178
Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S et al (2008) A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics 121(Suppl 4):S290-310. https://doi.org/10.1542/peds.2007-2243D.121/Supplement_4/S290
Sullivan MA, Rothenberg JL, Vosburg SK, Church SH, Feldman SJ, Epstein EM, Kleber HD, Nunes EV (2006) Predictors of retention in naltrexone maintenance for opioid dependence: analysis of a stage I trial. Am J Addict 15:150–159
Maremmani I, Pacini M, Giuntoli G, Lovrecic M, Perugi G (2004) Naltrexone as maintenance therapy for heroin addiction: predictors of response. Heroin Add and Rel Clin Probl 6(1):43–52
Aklin WM, Severtson SG, Umbricht A, Fingerhood M, Bigelow GE, Lejuez CW, Silverman K (2012) Risk-taking propensity as a predictor of induction onto naltrexone treatment for opioid dependence. J Clin Psychiatry 73(8):e1056–e1061. https://doi.org/10.4088/JCP.09m05807. PMID:22967782;PMCID:PMC3985274
Mannelli P, Patkar AA, Peindl K, Murray HW, Wu LT, Hubbard R (2007) Effectiveness of low-dose naltrexone in the post-detoxification treatment of opioid dependence. J Clin Psychopharmacol 27(5):468–474. https://doi.org/10.1097/jcp.0b013e31814e5e9d. PMID: 17873678
Schmitt SK, Phibbs CS, Piette JD (2003) The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addict Behav 28(6):1183–1192. https://doi.org/10.1016/s0306-4603(02)00218-6. PMID: 12834661
Tatara E, Lin Q, Ozik J, Kolak M, Collier N, Halpern D, Anselin L, Dahari H, Boodram B, Schneider J (2023) Spatial inequities in access to medications for treatment of opioid use disorder highlight scarcity of methadone providers under counterfactual scenarios. medRxiv [Preprint]. 2023.05.12.23289915. https://doi.org/10.1101/2023.05.12.23289915
Rosenblum A, Cleland CM, Fong C, Kayman DJ, Tempalski B, Parrino M (2011) Distance travelled and cross-state commuting to opioid treatment programs in the United States. J Environ Public Health 2011:948789
Acknowledgements
Not applicable.
Funding
We verify that this research was not funded by any institution or organization.
Author information
Authors and Affiliations
Contributions
BBL, MuK, and NY collected the data and were major contributors in writing the manuscript. FeR and UR reviewed all the relevant research and analyzed and interpreted the data. YHR guided the whole research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research work was initiated only after approval by the Institutional Ethical Committee, GMC Srinagar. Only those were taken for the study who gave the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lone, B.B., Jan, N., Kousar, M.U. et al. A study of predictors of retention to naltrexone maintenance therapy in patients with opioid use disorder: a prospective study. Middle East Curr Psychiatry 31, 61 (2024). https://doi.org/10.1186/s43045-024-00450-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-024-00450-5