Abstract
Background
Obsessive–compulsive disorder (OCD) is usually associated with insight’s heterogeneity, and those with poor insight showed lower BDNF and cognitive deficiencies. The aim was to detect the relation between insight to executive dysfunction and BDNF.
Materials and methods
Forty patients diagnosed with OCD and forty matched healthy controls. Also, both poor and good insight groups (assessed by The Brown Assessment of Belief Scale) were compared as regard Trail Making Test and serum level of BDNF).
Results
OCD patients group gave a significant worse performance in TMT and lower BDNF serum level than healthy control. Also, OCD patients with poor insight had lower BDNF level than patients with good to fair insight. ROC curve analysis confirmed that BDNF is a valuable diagnostic biomarker of insight in patients with OCD with 100% sensitivity and 72.41% specificity, p value < 0.001. Insight of OCD patients was not significantly associated with executive dysfunction detected by Trail Making Test.
Conclusions
OCD patients with poor insight had longer duration of illness, severe OCD symptoms, lower serum BDNF level, and longer time on TMTA-B than good insight patients. BDNF is a valuable diagnostic biomarker of insight in patients with OCD.
Similar content being viewed by others
Background
Obsessive–compulsive disorder (OCD) is defined as recurring, intrusive beliefs, urges, visions, or mental activities or behaviors that cause substantial suffering and psychosocial damage [5].
The approximate life expectancy incidence of OCD is about 2.3% [38]. 15–30% of cases with OCD are suggested to be correlated with inadequate understanding of one’s symptoms’ nature and severity [4, 8, 12]. This is associated with the insight's heterogeneity in the disorder [8, 12].
Insight was known as a possible reason for the poor success of intervention in OCD, with 20–25% as an inefficacy rate. In addition, emphasis has been brought to the various elements impacting insight, including the brain-derived neurotrophic factor (BDNF) [23, 24]. Cognitive deficiencies and neuropsychological issues may also contribute to poor insight [2].
Individuals with OCD perform worse in a number of executive function domains, such as processing speed, working memory, and sustained attention, as well as verbal memory/fluency and visuospatial abilities recall [1].
In contrast to OCD cases with excellent understanding and healthy control subjects, [23, 24] discovered that cases with OCD who had poor understanding could have worse executive performance in the Wisconsin Card Sorting Test (WCST) and Trail Making Test (TMT).
Many neuropsychiatric illnesses, particularly OCD, have been connected to the pathophysiology of BDNF. Much interest has revealed regarding BDNF in the pathophysiology of OCD due to its role in brain development, its documented role in the serotonergic neurons’ development and growth, and the proven influence of SRIs on levels of peripheral BDNF [26, 33].
This study aimed to assess executive functions and BDNF in patients with OCD and control group and to find the relation between both of them and insight in patients with OCD.
Materials and methods
This study is an observational, case–control study.
Procedure
The study passed through the following phases:
-
1-
Preparation phase
After a through literature review, the study question was formulated and the study protocol was prepared. The methods used in the current study were chosen based on the availability in Arabic Language, feasibility of application, and validity of the tools.
The research protocol was then granted the approval of the scientific and ethical committee of the Faculty of Medicine), Fayoum University (No. (M 587) in its session 93 on 10/4/2022).
-
2-
Data collection
The patients were enrolled from the Psychiatry Outpatient Clinic, Fayoum University that is conducted 3 days weekly through the period from first April 2022 till first of September 2022 by consecutive sampling.
The patients fulfilling the inclusion criteria were interviewed using the semi-structured interview derived from the psychiatric sheet of Fayoum Psychiatry Department, Relevant data involve (age at illness beginning, socio demographic data, duration of illness, family history), Clinical Interview dependent on DSM-5 to diagnose OCD, Yale-Brown Obsessive Compulsive Scale to evaluate severity of OCD, The Brown Assessment of Belief Scale (BABS) to detect insight among OCD cases. Then both of cases group and Control group were evaluated for cognition utilizing trail making test, and determining serum brain-derived neurotrophic factor level in both groups.
-
3-
Data analysis
Data was gathered, encoded, and secured in a personal computer with only the primary investigator having access. The suitable statistical tests were then selected after the data had been analyzed utilizing SPSS (Statistical Package for Social Sciences).
Each group’s minimum sample size was 40 individuals, based on the findings of prior study (Experimental Psychology Department, University of Heinrich Heine in Düsseldorf, Germany, used G power software version 3.1,7 to verify the sample size). Type 1 mistake with two tails, a power of 95%, and two sides. 1.2 impact size.
-
4-
Data interpretation
Discussion of the results was carried out to detect the significant findings and find out whether they support or refuse the study hypothesis. Conclusions, limitations, and recommendations were then addressed.
Subjects
Group A (patients group)
Inclusion criteria
Forty patients diagnosed with OCD (both genders, 18–50 years old, and drug naïve according to DSM 5 and severity was detected using the Yale-Brown Obsessive Compulsive Scale and was divided into two groups according to insight into patients with good insight and inadequate insight according to The Brown Assessment of Belief Scale.
Exclusion criteria
Other psychiatric comorbidities, substance use disorders, and inflammatory illness were excluded as they can affect executive functions and BDNF levels.
Group B (control group)
Forty healthy volunteers with absence of any psychopathology were selected among medical and paramedical health workers from Fayoum University Hospital and matched with the patients group in age, gender, education, socio-demographic, and economic status.
-
1
Psychometric assessment
-
➢ Semi-structured clinical interview depending on DSM-5: it is used diagnose OCD and to rule out other comorbidities.
-
➢ Yale-Brown Obsessive Compulsive Scale [14]: Arabic Version by [31] To evaluate OCD severity: it contains five items on obsessions and five items on compulsions(score 0:4 for each item). The highest t0tal score is 40. Patients who have both compulsions and obsessions fall into the following severity score ranges: score of subclinical = 0–7, mild = 8–15, moderate = 16–23, severe = 24–31, while extreme cases have 32–40. The threshold value for clinically significant symptoms is higher than 16.
-
➢ The Brown Assessment of Belief Scale (BABS): [10] to estimate insight: this was translated and back translated by colleagues in Psychiatry Department, Kasr El Eini Hospital, the arabic version was prepared for publication but not submitted.
The total BABS number is calculated by adding the first six items out of the seven items. The final score does not take into account an extra item (ideas of reference). Each object has a rating from 0 to 4 (from least to most severe). The final response chosen for each item relies on the interviewer’s clinical judgment; however, the items are generally rated depending on the patient’s statement.
-
➢ Trail Making Test (quoted by [35] (Arabic Version) by [39]: to detect executive function: the task is divided into two parts, and the subject must associate a group of 25 dots instantaneously and precisely. The exam can reveal details about executive functioning as well as scanning, processing speed, visual search speed, and mental flexibility.
-
-
2
Biochemical measures to assess BDNF: The Department of Clinical Pathology, Fayoum University conducted the study of the clinical chemistry parameter. A nurse used aseptic venipuncture to gather venous samples from each participant. The blood sample was then put in serum separator vacutainer tubes, and then an experienced laboratory technician centrifuged the specimens at a speed of 3000 rpm, within 30 min. The separated serum was kept and frozen in an Eppendorf tube until analysis at – 20 °C. BDNF was quantified using a widely available enzyme-linked immunosorbent assay (ELISA) kit.
Statistical analysis
Statistical analysis was done by SPSS version 28 (IBM Co., Armonk, NY, USA). The normality for each variable was tested by Wilk-Shapiro test and for every non-parametric variable, the median was used. Numerical variables such as median and interquartile range (IQR) were studied by Mann–Whitney test. Categorical variables were showed as frequency and percentage (%) and tested using the chi-square test.
Spearman’s rank correlation coefficient was used to estimate the correlation between two non-parametric quantitative variables. The overall diagnostic performance of BDNF was evaluated by ROC curve analysis. A two tailed P value < 0.05 was considered statistically significant.
Results
The two studied groups show no statistically significant difference regarding socio-demographics represented by (age, gender, marital status, occupation, residence, educational level, and socio-economic level) (Table 1).
Out of the forty OCD patients, 27.5% had family history of OCD. The onset of OCD occurred at a median age of 22.5 years with IQR from 20–31.5 years. The median duration of illness was 4 years with IQR from 3–6 years. Symptoms’ severity was assessed by Y-BOCS which gave a median score of 22 with IQR from 16 to 28 as demonstrated in Table 2.
Executive functions were evaluated via tests as TMT. OCD patients had a problem adapting to the rules change, therefore gave a worse performance in TMT with significantly longer time as compared to healthy participants (P values < 0.001) (Table 3). BDNF serum level is lower in OCD patients (0.51) than healthy control (0.75) with p value 0.013 (Table 3).
The forty OCD patients were divided and further analyzed according to The Brown Assessment of Belief Scale that evaluates insight into good insight group which included 29 patients and poor insight group that included 11 patients.
No statistically significant association between insight and sociodemographic data was found in OCD patients as shown in Table 4.
There was no significant relation between insight and family history and age at onset of OCD. Duration of illness showed statistically significance difference as, OCD patients who with poor insight had OCD with higher median 6 years and IQR from 4 to 8 years than patients with good to fair insight with median 4 years and IQR from 2 to 5 years, p value = 0.003. Also, insight of OCD patients was not significantly associated with executive function detected by Trail Making Test (Table 5).
The correlation between BDNF and both executive function and severity of symptoms in OCD patients was demonstrated in Table 6, showing a significant negative correlation between BDNF and Y-BOCS severity (r = − 0.430, P = 0.006) in all OCD patients (Table 6).
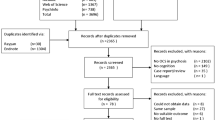
ROC curve analysis confirmed that BDNF is a valuable diagnostic biomarker of insight in patients with OCD with 100% sensitivity and 72.41% specificity, p value < 0.001 as shown in Fig. 1.
Discussion
Serum brain-derived neurotrophic factor levels
As regard the median serum brain-derived neurotrophic factor there was statistically significant difference in which case group was lower than control group (Table 3). This result was in accordance with those obtained by [15, 42] who found OCD sufferers have lower plasma amounts of BDNF than healthy controls. Additionally, patients had significantly lower blood levels of BDNF contrasted to healthy controls, according to a random-effects meta-analysis (Hedges’ g = − 0.722, 95% confidence interval [CI] = − 1.152 to − 0.292, P 0.001). These outcomes indicate that BDNF may be a prospective biomarker for OCD [17].
However, these findings were inconsistent with [3] as serum BDNF concentrations in the OCD patients group were greater than in the control group. The present study was different with [3] study whose OCD patients were under SRIs medications, had demonstrated that SRIs elevate peripheral BDNF levels in humans while cases in the present study were drug naïve.
Executive functions deficit in OCD
In the present study, as regard the median scores of TMT-A and TMT-B, they were significantly greater in OCD patients than in controls (Table 3). These results agreed with [19] who stated that both TMT A and B were greater in cases with OCD (with significant p value = 0.01, and p value = 0.0005, consecutively).
The length of time it takes for OCD cases and controls, to respond to TMT-A was observed to be significantly different between them [37] in which the OCD cases responded more slowly than the controls did. Also, Spalletta et al. 2014 found selective impairments in executive functioning measures of cognitive flexibility (TMT part B) with OCD patients (171.40 s) and control group (110.95 s) with (p value = 0.007) [16]; discovered that OCD samples performed inadequately on set-shifting tasks like the TMT-B.
The present study was in line with [7] who exhibit that OCD cases had a great dysfunctions across all cognitive domains (flexibility, decision-making, inhibition, attention, memory, verbal fluency, and planning). [34] had been recommended that deficits in cognitive flexibility might express a cognitive endophenotype for OCD.
The insight’s belief has been the controversy’s object so the forty OCD patients were divided and further analyzed according to The Brown Assessment of Belief Scale that evaluates insight into good insight group which included 29 patients and poor insight group that included 11 patients.
Insight and sociodemographic factor
There was no statistically significant correlation between insight and sociodemographic in OCD represented by age, gender, marital status, occupation, residence, educational level, and socioeconomic level (Table 4).
These results were consistent with [22, 40], and [21] who observed that no significant group differences (good, poor, and controls) in different socio-demographic aspects of age, gender, and education levels, background (urban/rural), and marital status.
Insight and family history in OCD patient
Regarding he present study, there was no significant correlation between insight, family history of OCD and age of onset (Table 5).
These findings contradicted those of [8, 21], in which poor insight had been correlated with an early-age of beginning. Poor insight cases with obsessive–compulsive disorder (OCD) were linked to worse OCD symptoms, a younger age of onset, comorbid depression, and poor medication outcomes, according to [18]. The difference between the present study and their studies as regard age of onset may be owing to small sample size (poor insight patients = 11).
Regarding family history, these results were in line with [21] who observed that family history did not differ significantly with (p value = 0.76) between cases with poor insight and patients with good insight).
Regarding duration of illness, our results showed statistically significance difference as OCD cases who with poor insight had OCD with higher median 6 years than patients with good to fair insight with median 4 years (p value = 0.003) (Table 5) this finding was in line with that observed in [6, 21, 27, 32].
Also, [8] stated that poor insight had been linked to longer period of illness.
Insight and severity of OCD symptoms
Our findings stated a potent correlation between poor insight and OCD severity according to Y-BOCS (Table 5).
These results were consistent with [32] study in which the severity was the greatest indicator of poor insight, making poor insight the severest obsessive–compulsive continuum. Also [8], discovered that OCD cases with poor insight demonstrated an obsessive–compulsive’s extreme severity. As regards [41]’s study, poor insight was linked to severe prevalence of OCD and a greater medication resistance.
Insight and serum BDNF
In this study, regarding median serum BDNF level there was statistically significant difference between poor and good patients insight (Table 5).
This outcome was consistent with that of Manarte et al. [23, 24] who discovered that the BDNF levels in the poor-insight group were lower than in the control groups and good-insight.
Marinova et. al [25] showed that glutamate-modulating drugs in OCD (memantine) demonstrated a positive impact as an augmentation treatment in intense cases of OCD which may have poor insight. [36] demonstrated elevated BDNF protein levels in the prefrontal cortex which shed light for the relation between BDNF and OCD.
Insight and executive function deficit in OCD patient
Regarding (TMT), TMT A and B scores were higher in poor insight cases but not statistically significant than good insight patients.
Manarte et al. [23, 24] found clear differences between good and poor insight group with p value for TMT-A and TMT-B = 0.003, 0.002 respectively. The difference may be due to small sample size (poor insight patient (11) for good insight (29)).
Additionally, Kashyap et al. [20] discovered that on the Trail Making test (TMT), the OCD patients whom had poor insight was worst in the test than patients with good insight.
Correlative results
In the present study, as regards association between BDNF and symptoms' intensity in OCD patients there is a significant negative relationship between BDNF and YBOCS severity (p value = 0.006) (Table 6). There is a negative correlation between BDNF in poor insight patient and OCD severity which indicate low BDNF serum level associated with poor insight patient and severe OCD symptom. These findings were similar to [9], in validating the association between intensity of OCD and serum BDNF levels, particularly in sexual/religious symptom’s dimension. However [42], found that there was no significant relation between illness severity and plasma levels of BDNF (Y-BOCS score).
Regarding Trail Making Test (A-B) there was a negative correlation between BDNF in all OCD patient and trail making test (A-B) but not statistically significant (Table 6) which indicate patient took longer time to perform TMT associated with low BDNF serum level.
This result was in accordance with those obtained by [13] and [29, 30],their study found that BDNF Val66Met genotype has been linked with changes in variety cognitive functions as EF. Additionally, Mohapatra et al. 2020 revealed that patients with OCD whose serum BDNF level is significantly lowered (p value = 0.002) have significantly lower levels of visuospatial capability, attention, and concentration.
Diagnostic performance of BDNF in predicting poor insight in OCD
Different levels of understanding of the biological causes of diseases result in significantly different conditions for successful treatment [43].
The present study confirmed that BDNF is a valuable diagnostic biomarker of insight in patients with OCD with 100% sensitivity and 72, 41% specificity (Fig. 1). Our results support findings from [23, 24] shown that the poor-insight group’s BDNF values were lower than good-insight group. This is a likely path for future research for medication of poor insight OCD cases. This is also, supported by genetic studies as [11] found that the genotypic frequency of Val66Met of the BDNF gene differed between people with OCD and healthy participants and MJ et al. [28] observed that protective impact of the ‘Met’ allele in OCD especially at the Val66Met locus.
Limitation of the study
The whole sample size in our study and those with poor insight were relatively small, which may affect the meaningful associations. This study enrolled only clinically based participants and they may have sufficient ability to detect their insight and to acknowledge symptom severity which may lead to skewed insight scores. This may affect the power to detect significant associations among the predictor variables.
Conclusion
OCD patients with poor insight had longer duration of illness, severe OCD symptoms, lower serum BDNF level, longer time on TMTA-B than good insight patients. BDNF is a valuable diagnostic biomarker of insight in patients with OCD with 100% sensitivity and 72.41% specificity (p value < 0.001).
Availability of data and materials
Not applicable.
Abbreviations
- BABS:
-
Brown Assessment of Beliefs Scale
- BDNF:
-
Brain-derived neurotrophic factor
- CI:
-
Confidence interval
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders-5
- OCD:
-
Obsessive compulsive disorder
- P-value:
-
Probability value
- SCID-5-RV:
-
Structure clinical interview 5
- SRIs:
-
Serotonin reuptake inhibitors
- TMT:
-
Trail Making Test
- Y-BOCS:
-
Yale-Brown Obsessive Compulsive Scale
References
Abramovitch A, Abramowitz JS, Mittelman A (2013) The neuropsychology of adult obsessive–compulsive disorder: a meta-analysis. Clin Psychol Rev 33(8):1163–1171. https://doi.org/10.1016/j.cpr.2013.09.004
Aigner M, Zitterl W, Prayer D, Demal U, Bach M, Prayer L et al (2005) Magnetic resonance imaging in patients with obsessive–compulsive disorder with good versus poor insight. Psychiatry Res Neuroimaging 140(2):173–179. https://doi.org/10.1016/j.pscychresns.2005.03.002
Akimoto T, Sutoh C, Kuno M, Matsuzawa D, Niitsu T, Iyo M, Shimizu E (2021) Serum levels of brain-derived neurotrophic factor in patients with obsessive-compulsive disorder in a Japanese population. Open J Psychiatry 11(1):20–28. https://doi.org/10.4236/ojpsych.2021.111003
Alonso P, Menchón JM, Segalàs C, Jaurrieta N, Jiménez-Murcia S, Cardoner N et al (2008) Clinical implications of insight assessment in obsessive-compulsive disorder. Compr Psychiatry 49(3):305–312. https://doi.org/10.1016/j.comppsych.2007.09.005
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Bellino S, Patria L, Ziero S, Bogetto F (2005) Clinical picture of obsessive-compulsive disorder with poor insight: a regression model. Psychiatry Res 136(2–3):223–231. https://doi.org/10.1016/j.psychres.2004.04.015
Benzina N, Mallet L, Burguière E, N’Diaye K, Pelissolo A (2016) Cognitive dysfunction in obsessive-compulsive disorder. Current Psychiatry Report 18(9):80. https://doi.org/10.1007/s11920-016-0720-3. PMID: 27423459
Catapano F, Perris F, Fabrazzo M, Cioffi V, Giacco D, De Santis V, Maj M (2010) Obsessive–compulsive disorder with poor insight: a three-year prospective study. Prog Neuropsychopharmacol Biol Psychiatry 34(2):323–330. https://doi.org/10.1016/j.pnpbp.2009.12.007
Dos Santos IM, Ciulla L, Braga D, Ceresér KM, Gama CS, Kapczinski F, Ferrão YA (2011) Symptom dimensional approach and BDNF in unmedicated obsessive-compulsive patients: an exploratory study. CNS spectrums 16(9):179–189. https://doi.org/10.1017/S1092852912000363
Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA (1998) The brown assessment of beliefs scale: reliability and validity. Am J Psychiatry 155(1):102–108. https://doi.org/10.1176/ajp.155.1.102
First MB, Williams JB, Karg RS, Spitzer RL (2015) User’s guide for the structured clinical interview for DSM-5 disorders, research version (SCID-5-RV). American Psychiatric Association, Arlington
Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA & Rasmussen SA. (1995). Erratum: DSM-IV field trial: Obsessive-compulsive disorder (American Journal of Psychiatry (January 1995)(90–96)). Am J Psychiatry. 152(4).
Gajewski PD, Hengstler JG, Golka K, Falkenstein M, Beste C (2011) The Met-allele of the BDNF Val66Met polymorphism enhances task switching in elderly. Neurobiol Aging 32(12):2327-e7. https://doi.org/10.1016/j.neurobiolaging.2011.06.010
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989) The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Arch Gen Psychiatry 46(11):1006–1011. https://doi.org/10.1001/archpsyc.1989.01810110048007
Guo HR, Huang BL, Wang YL, Zhang YY, Ma QG, Lv PP, Ren YM (2020) Effect of escitalopram on serum GDNF and BDNF levels and 5-HT level of brain tissue of obsessive–compulsive disorder rats. Cell Mol Neurobiol 40:991–997. https://doi.org/10.1007/s10571-020-00788-4
Hamo N, Abramovitch A, Zohar A (2018) A computerized neuropsychological evaluation of cognitive functions in a subclinical obsessive-compulsive sample. J Behav Ther Exp Psychiatry 59:142–149. https://doi.org/10.1016/j.jbtep.2018.01.004
Hao LS, Du Y, Chen L, Jiao YG, Cheng Y (2022) Brain-derived neurotrophic factor as a biomarker for obsessive-compulsive disorder: a meta-analysis. J Psychiatr Res. https://doi.org/10.1016/j.jpsychires.2022.05.026
Jakubovski E, Pittenger C, Torres AR, Fontenelle LF, do Rosario MC, Ferrão YA et al (2011) Dimensional correlates of poor insight in obsessive–compulsive disorder. Prog Neuro Psychopharmacol Biol Psychiatry 35(7):1677–1681. https://doi.org/10.1016/j.pnpbp.2011.05.012
Karagüzel EÖ, Arslan FC, Uysal EK, Demir S, Aykut DS, Tat M, Karahan SC (2019) Blood levels of interleukin-1 beta, interleukin-6 and tumor necrosis factor-alpha and cognitive functions in patients with obsessive compulsive disorder. Compr Psychiatry 89:61–66. https://doi.org/10.1016/j.comppsych.2018.11.013
Kashyap H, Kumar JK, Kandavel T, Reddy YJ (2012) Neuropsychological correlates of insight in obsessive–compulsive disorder. Acta Psychiatr Scand 126(2):106–114. https://doi.org/10.1111/j.1600-0447.2012.01845.x
Kishore VR, Samar R, Reddy YJ, Chandrasekhar CR, Thennarasu K (2004) Clinical characteristics and treatment response in poor and good insight obsessive–compulsive disorder. Eur Psychiatry 19(4):202–208. https://doi.org/10.1016/j.eurpsy.2003.12.005
Liu W, Gan J, Fan J, Zheng H, Li S, Chan RC et al (2019) Associations of cortical thickness, surface area and subcortical volumes with insight in drug-naive adults with obsessive-compulsive disorder. NeuroImage Clinical 24:102037. https://doi.org/10.1016/j.nicl.2019.102037
Manarte L, Andrade AR, do Rosário L, Sampaio D, Figueira ML, Morgado P, Sahakian BJ (2021) Executive functions and insight in OCD: a comparative study. BMC psychiatry 21(1):1–11. https://doi.org/10.1186/s12888-021-03227-w
Manarte L, Saldanha J, Andrade AR, Tanqueiro S, Morgado P, Sahakian BJ (2021) Plasma BDNF and insight in OCD: a promising path for future research. Acta Neuropsychiatrica 33(5):277–279. https://doi.org/10.1017/neu.2021.17
Marinova Z, Chuang DM, Fineberg N (2017) Glutamate-modulating drugs as a potential therapeutic strategy in obsessive-compulsive disorder. Curr Neuropharmacol 15(7):977–995. https://doi.org/10.2174/1570159X15666170320104237
Matrisciano F, Bonaccorso S, Ricciardi A, Scaccianoce S, Panaccione I, Wang L et al (2009) Changes in BDNF serum levels in patients with major depression disorder (MDD) after 6 months treatment with sertraline, escitalopram, or venlafaxine. J Psychiatr Res 43(3):247–254. https://doi.org/10.1016/j.jpsychires.2008.03.014
Matsunaga H, Kiriike N, Matsui T, Oya K, Iwasaki Y, Koshimune K et al (2002) Obsessive-compulsive disorder with poor insight. Compr Psychiatry 43(2):150–157. https://doi.org/10.1053/comp.2002.30798
MJ RJT, Ganesh S, Shukla T, Deolankar S, Nadella RK, Sen S, Viswanath B (2018) BDNF gene and obsessive compulsive disorder risk, symptom dimensions and treatment response. Asian J Psychiatr 38:65–69. https://doi.org/10.1016/j.ajp.2017.10.014
Montag C, Felten A, Markett S, Fischer L, Winkel K, Cooper A, Reuter M (2014) The role of the BDNF Val66Met polymorphism in individual differences in long-term memory capacity. J Mol Neurosci 54:796–802. https://doi.org/10.1007/s12031-014-0417-1
Montag C, Weber B, Fliessbach K, Elger C, Reuter M (2009) The BDNF Val66Met polymorphism impacts parahippocampal and amygdala volume in healthy humans: incremental support for a genetic risk factor for depression. Psychol Med 39(11):1831–1839. https://doi.org/10.1017/S0033291709005509
Okasha A, Saad A, Khalil AH, El Dawla AS, Yehia N (1994) Phenomenology of obsessive-compulsive disorder: A transcultural study. Compr Psychiatry 35(3):191–197. https://doi.org/10.1016/0010-440X(94)90191-0
Ottoni R, Pellegrini C, Mora L, Marchesi C & Tonna M. (2022). Psychopathology of insight in obsessive–compulsive disorder. Curr Psychol. 1–9. https://doi.org/10.1007/s12144-022-02806-8
Piccinni A, Marazziti D, Catena M, Domenici L, Del Debbio A, Bianchi C et al (2008) Plasma and serum brain-derived neurotrophic factor (BDNF) in depressed patients during 1 year of antidepressant treatments. J Affect Dis 105(1–3):279–283. https://doi.org/10.1016/j.jad.2007.05.005
Rajender G, Bhatia MS, Kanwal K, Malhotra S, Singh TB, Chaudhary D (2011) Study of neurocognitive endophenotypes in drug-naïve obsessive–compulsive disorder patients, their first-degree relatives and healthy controls. Acta Psychiatr Scand 124(2):152–161. https://doi.org/10.1111/j.1600-0447.2011.01733.x
Reitan RM (1956) Trail Making Test: Manual for administration, scoring and interpretation. Indiana University, Bloomington, p 134
Réus GZ, Abelaira HM, Stringari RB, Fries GR, Kapczinski F, Quevedo J (2012) Memantine treatment reverses anhedonia, normalizes corticosterone levels and increases BDNF levels in the prefrontal cortex induced by chronic mild stress in rats. Metab Brain Dis 27:175–182. https://doi.org/10.1007/s11011-012-9281-2
Roh KS, Shin MS, KIM MS, HA TH, SHIN YW, Lee KJ & Kwon, JS, (2005) Persistent cognitive dysfunction in patients with obsessive-compulsive disorder: a naturalistic study. Psychiatry Clin Neurosci 59(5):539–545. https://doi.org/10.1111/j.1440-1819.2005.01411.x
Ruscio AM, Stein DJ, Chiu WT, Kessler RC (2010) The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 15(1):53–63. https://doi.org/10.1038/mp.2008.94
Stanczak DE, Stanczak EM, Awadalla AW (2001) Development and initial validation of an Arabic version of the Expanded Trail Making Test: Implications for cross-cultural assessment. Arch Clin Neuropsychol 16(2):141–149. https://doi.org/10.1016/S0887-6177(99)00060-8
Türksoy N, Tükel R, Özdemir Ö, Karali A (2002) Comparison of clinical characteristics in good and poor insight obsessive–compulsive disorder. J Anxiety Disord 16(4):413–423. https://doi.org/10.1016/S0887-6185(02)00135-4
Visser H, van Megen H, van Oppen P, Hoogendoorn A, Glas G, Neziroglu F, van Balkom A (2017) The impact of poor insight on the course of obsessive-compulsive disorder in patients receiving naturalistic treatment. J Obs Compuls Relat Disord 13:42–48. https://doi.org/10.1016/j.jocrd.2017.03.003
Wang Y, Mathews CA, Li Y, Lin Z, Xiao Z (2011) Brain-derived neurotrophic factor (BDNF) plasma levels in drug-naïve OCD patients are lower than those in healthy people, but are not lower than those in drug-treated OCD patients. J Affect Disord 133(1–2):305–310. https://doi.org/10.1016/j.jad.2011.04.002
Zink M (2014) Comorbid obsessive-compulsive symptoms in schizophrenia: insight into pathomechanisms facilitates treatment. Adv Med. https://doi.org/10.1155/2014/317980
Acknowledgements
The authors express their deep gratitude to all the participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MS prepared the main idea and contributed in writing the manuscript. MD and LM prepared the questionnaires, analyzed and interpreted the patient data regarding the clinical data and psychometric tools, and was a major contributor in writing the manuscript. HD was the major contributor in revising the manuscript. MA was the main supervisor of clinical chemistry work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Fayoum University Faculty of Medicine's Ethical Committee gave their stamp of approval to the study proposal (No. (M 587) in its session 93 on 10/4/2022). All participants were required to provide written informed permission. The primary investigator was in charge of going over consent forms that had been signed and examining the subject’s files and data.
Patient’s data was coded and secured in a personal computer with no access not including for principal and co-investigator.
Consent for publication
All authors approved the manuscript and give their consent for submission and publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soltan, M.R., Dessoki, H.H., Abbas, M.M. et al. Study of insight in patients with obsessive compulsive disorder and its relation to executive functions and serum brain-derived neurotrophic factor. Middle East Curr Psychiatry 30, 75 (2023). https://doi.org/10.1186/s43045-023-00348-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00348-8