Abstract
Background
Children with Duchenne muscular dystrophy report a higher rate of cognitive and psychiatric disorders relative to general population. This study will describe and compare the psychiatric and cognitive problems in DMD patients with healthy controls.
Results
A statistically significant difference was found between the case and control groups regarding Total IQ (TIQ) with a mean of (82 ± 16) in cases compared to (94 ± 10) in controls, in which 58% of DMD boys had <90 TIQ and 40% less than 70. We also found that 58% of cases have delayed onset of speech, 38% have attention-deficit/hyperactivity disorder, 6% have autism spectrum disorder, 14% have anxiety disorders, and 22% have major depressive disorder. Ninety-two percent of cases had deletion mutations.
Conclusions
According to our results, we conclude that boys with DMD had a lower Total IQ and higher rate of psychiatric disorders than the general population. Also, school attendance and speech development are more affected in DMD patients compared to controls, with more speech delay and dropping out of school. So, the authors of this study recommend establishing cognitive and psychiatric screening as a routine in the evaluation and follow-up of DMD children.
Similar content being viewed by others
Background
Duchene muscular dystrophy (DMD), one of the most prevalent genetic diseases, affecting around 1 in 3600–6000 live male births [1]. It is an X-linked recessive disease brought on by genetic changes that alter the dystrophin (DYS) protein, a key component of the dystrophin-glycoprotein complex (DGC). Progressive muscular degeneration and non-progressive cognitive deficits are a hallmark of the disease. Brain comorbidities may have a more significant effect on the family than mobility for those with DMD [2]. Additionally, DYS has an important role in the architectural arrangement of the central nervous system (CNS). It is involved in the organization of gamma-aminobutyric acid type A (GABAA) receptors, which are normally expressed at the postsynaptic membrane in inhibitory synapses of structures related to cognition and emotional behavior, such as the hippocampus, amygdala, cerebellum, and sensory cortices [3].
The DMD gene has numerous separate, tissue-specific promoters that work to create a variety of isoforms with different lengths and splicing patterns. There are at least seven promoters and eight dystrophin isoforms in the DMD gene (Dp427p, c, m, Dp260, Dp140, Dp116, Dp71, and Dp40). These isoforms are expressed in various tissue types and have names that reflect their relative sizes. It is believed that the isoforms Dp140 and Dp71, which are only expressed in the brain, are crucial for fetal brain development [2, 4].
Although the expression of dystrophin in the brain is only 10% that of the muscle, the protein products of the dystrophin gene are significantly more variable in brain tissue. The primary protein expressed in the brain, Dp71, is one of them. It is probable that Dp71 has a role in blood brain barrier (BBB) function and the potential entry of peripheral inflammatory chemicals into the brain because it is present near perivascular astrocyte end foot. Dp427c is only found in neurons in the central nervous system (CNS) and only in particular parts of the brain, including the hippocampus, amygdala, cerebellar Purkinje cells, and neocortex. For the development and maintenance of new synaptic connections, Dp427’s interaction with DGC would be crucial [5].
Learning and behavioral issues in DMD can be identified early in infancy and can affect patients with cognitive impairment as well as those with IQs in the normal to high range. Consistent reports show that Full Scale IQ for DMD differs by one standard deviation from the general population [6]. However, screening for behavioral or learning issues in DMD patients is not always performed, and when it is, a range of different diagnostic tools are used. There is not yet a set of DMD-specific diagnostic tests available. Once it is, it will be possible to more accurately describe the incidence and severity of the cognitive profile. Understanding the potential relationships between dystrophin isoforms and the cognitive profile requires taking this important step [2].
In the meantime, dystrophin protein deficiency results in neurobehavioral disorders such as attention-deficit/hyperactivity disorder (ADHD), diseases of the autism spectrum, and obsessive-compulsive disorder [7].
Children with DMD encounter specific problems in cognitive functioning. A lower Verbal IQ (VIQ) than Performance IQ (PIQ) has been replicated numerous times. However, these discrepancies are not demonstrated by all children with DMD. Impairments have been reported in confrontational naming, verbal fluency, reading, phonological and graphological production, receptive language, expressive language, and verbal learning [8].
Furthermore, compared to other verbal or memory measures, boys with DMD do worse on tasks requiring attention to complicated verbal information. The potential for the missing dystrophin brain products to influence specific types of cognitive functioning is considered [9].
On the other hand, there are a percentage of boys with DMD who not only lack the full-length dystrophin protein, but also one or more of the five smaller dystrophin isoforms that are localized in the CNS. Study of the genotype–phenotype correlation in boys with DMD, especially in regard to behavior and cognition, is essential to understand the role of dystrophin in the CNS [10].
Surprisingly, the effect of neuromuscular diseases on the cognitive function spectrum is still poorly understood despite having a wide variety of clinical manifestations. In contrast to the studies on how altered executive functions in mental disorders such as anxiety, depression, and bipolar disorder can affect motor performance [11], in this study we aimed to describe the psychiatric and cognitive problems in DMD compared with healthy controls.
Methods
This is a cross-sectional analytical study conducted in Okasha Institute of Psychiatry and neuromuscular clinic of Ain Shams University hospitals; a hundred male children/adolescents, aged between 5 and 16 years, were enrolled. They were divided into two groups: 50 boys with genetically confirmed DMD in the case group compared to 50 healthy boys in control group. Sample size was calculated using PASS 11 program for sample size calculation, and according to [12], the expected proportion of psychosocial problems at children with DMD = 15–47% (30 ± 15%), sample size of 36 controls, can detect prevalence of cognitive psychosocial problems in cases with 95% confidence level; based on this, the needed sample size consisted of at least 36 patients in the case group and 36 participants in the control group to detect this difference.
All 100 boys had neuropsychological assessment by a single clinical psychologist. Excluded from both groups are patients who had any other medical or neurological condition, those with history of brain trauma or surgical condition that could potentially impact cognitive functioning, symptomatic carriers, patients of other types of muscular dystrophy, those who declined to take part in the study, and those with severe speech delay that prevent them from performing cognitive and psychological tests.
Procedures
A standardized structured interview was held for each patient covering domains including history of sociodemographic data such as age, consanguinity, educational status, current psychiatric history, current general medical history, speech development, and onset of motor symptoms.
Genetic testing strategies for the DMD patients included:
-
Multiplex ligation-dependent probe amplification (MLPA): to detect deletion/duplication of one or more exons of the DMD gene.
-
Sanger sequencing: if the pathogenic variant involved small variants such as missense, nonsense, small insertion and deletion, and splicing variants. The genetic testing was done in either Centogene laboratories in Germany or the Medical Research Centre of Excellence (MRCE) in Egypt.
-
Dystrophin gene isoform disruptions were predicted in accordance to Taylor et al. [13].
Cognitive assessment
All 100 boys had psychological assessment by a single clinical psychologist.
-
(1)
For boys aged 6 years and above, the Wechsler Intelligence Scale for Children WISC-IV. The WISC-IV is divided into 15 subtests, with 5 new subtests added to WISC-III. They include 3 core tests—Picture Concepts, Letter-Number Sequencing, Matrix Reasoning—and 2 supplemental tests—Cancellation and Word Reasoning. Full Scale IQ was depending on the total combined performance of the Verbal Comprehension Index, Perception Reasoning Index, Working Memory Index, and Processing Speed Index [14].
-
(2)
Benton Visual Retention Test (BVRT): An individually administered test that assesses visual memory and visual perception. It also helps in identifying possible learning disabilities among other afflictions that could affect a person’s memory. The subject is instructed to duplicate each of the ten drawings on plain paper as accurately as possible from memory after being shown each of them one at a time. The test has no time limit, and results are calculated professionally by form, shape, pattern, and arrangement [15].
Assessment of psychiatric disorders
-
(1)
The Mini International Neuropsychiatric Interview for children and adolescents (MINI KID) [16]: The version used in this study is the Arabic version that was translated into Arabic language and had the reliability and validity tests done by [17]: for diagnosis of presence of any psychiatric disorders.
-
(2)
Conners’ Parent Rating Scale-Revised: Long Version (CPRS-R:L) [18] (For Those who have ADHD symptoms in MINI KID) [19]. This is an 80-question rating scale that assesses symptom severity as reported by parents.
-
(3)
Children Depression Inventory (CDI) [20] (For Those who have Depression by MINI KID). It is a 27-item self-report screening measure for mood symptoms in children. The parent-rated Arabic version of the scale prepared by [21] was used.
-
(4)
The Childhood Autism Rating Scale (CARS) [22]. The Arabic version of this scale was prepared by [23].
-
(5)
The Taylor Manifest Anxiety Scale (TMAS) [24] (For Those who have Anxiety Disorders by MINI KID). The Arabic version of the scale was prepared by [25].
-
(6)
CHILDREN’S YALE-BROWN OBSESSIVE COMPULSIVE SCALE (CY-BOCS) [26]. The version used in this study is the Arabic version that was translated into Arabic language and used by [27] (For Those who have OCD symptoms by MINI KID).
Statistical analysis
The collected data was revised, coded, tabulated, and introduced to a PC using Statistical Package for the Social Sciences (SPSS 25). Data was presented and suitable analysis was done according to the type of data obtained for each parameter using mean, standard deviation, and range for parametric numerical data, while median and interquartile range (IQR) for non-parametric numerical data, the Student t test, the Mann-Whitney test, ANOVA test, the Kruskal-Wallis, post hoc test, chi-square test, Fisher’s exact test, correlation analysis (using Spearman’s rho method). The p-value was used to indicate the level of significance where p>0.05 is non-significant (NS) and p < 0.05 is significant (S).
Results
The study sample is composed of 100 boys distributed as 50 cases and 50 controls meeting the inclusion and exclusion criteria
-
A.
When comparing between the case and control groups: a statistical significance regarding school attendance (p<0.001) evident in that 19 (38%) of the boys with Duchene muscular dystrophy (DMD) were home-schooled and 8 (16%) stopped going to school compared to 0% of the control group. There was also a statistically significant difference in parental consanguinity showing 20% of cases with 1st degree consanguinity compared 0% in the control group. A statistical significance was also evident in speech development between cases and control with 92% of the control group having normal speech development compared to only 40% of cases, as shown in Table 1.
-
B.
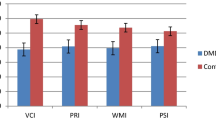
When comparing between the two groups regarding Full Scale IQ (FSIQ): our results showed that there was a highly significant difference in the TIQ and all its subsets except similarities as the case group had a median TIQ of (82±16) in comparison to (94±10) in the control group. Also, it was found that verbal IQ (VIQ) and Performance IQ (PIQ) had a mean of (82±22) and (83±17) respectively in the case group compared to a mean of (95±11) and (94±8) in the control group. The lowest scores in DMD boys were in general comprehension and vocabulary with a median of 6 and digit span with a mean of (6±2), as shown in Table 2 (at the end of the document text file).
-
C.
Regarding Total IQ (TIQ) distribution in the case group, we found that those with <90 TIQ represented 58% of DMD boys with those less than 80 representing 40% of cases, as shown in Table 3.
-
D.
During comparison of Benton Visual Retention Test (BVRT) and presence of psychiatric disorders and their severity by The Mini International Neuropsychiatric Interview for children and adolescents (MINI KID), we found that BVRT showed no statistical significance between the two groups. Yet there was a statistically significant difference (p=0.003) evident in that 29 boys (52%) of the case group had a positive MINI KID confirming the presence of psychiatric disorder compared to 16 boys (32%) of the control group.
-
E.
When comparing both groups regarding Conners’ assessment for ADHD and its subsets, there was a significant difference (p=0.047) between the 2 groups as the case group had 19 boys (38%) with ADHD compared to 10 boys (20%) of the control group, with the case group having the lowest score in oppositionality, yet with high scores in social aggression. When comparing different psychiatric disorders and their severity between the two groups, it was found that there was no statistically significant difference regarding autism spectrum disorder (ASD) as only 3 of the case group had positive The Childhood Autism Rating Scale (CARS); also according to Taylor’s scale for anxiety, there was no statistically significant difference as the number of boys with anxiety was equal in both groups and no cases or controls had obsessive-compulsive disorder (OCD). A statistically significant difference (p=0.007) was found in presence of major depressive disorder (MDD) as 11 boys (22%) of the case group had positive Children Depression Inventory CDI compared to 2 boys (4%) in the control group. Of those with MDD in the case group, 7 boys had moderate depression and 3 had mild depression while only 1 had severe depression as shown in Table 4.
-
F.
Genetic analysis
-
(1)
Mutation analysis of the dystrophin gene among the case group revealed: forty-six (92%) had exon deletions, 2 (4%) had had exon duplications, and 2 (4%) had point mutations (nonsense mutations) as shown in Table 5.
-
(2)
The full-length dystrophin isoform was not produced in all cases, Dp260 was disrupted in 86% of cases and Dp140utr was disrupted in 76%, while Dp140pc was disrupted in 64% of cases, with Dp71 only disrupted in 10% of cases, as shown in Table 6.
-
(1)
Discussion
Duchene muscular dystrophy )DMD( is characterized by the progressive loss of muscle strength and function [28]; moreover, cognitive function impairment and neuropsychiatric symptomatology are also prevalent. So, in this study, 50 boys with DMD were assessed aiming to assess cognitive functions and psychiatric symptoms suggestive of psychiatric disorders compared to 50 healthy boys.
Our results showed a statistical significance regarding school attendance evident in that 38% of the DMD boys were home-schooled and 16% stopped going to school compared to 0% of the control group. This was in contrast to Magliano and his colleagues who explored the burden in parents and healthy siblings of 4–17-year-old patients with Duchenne (DMD) and Becker (BMD) muscular dystrophies, data was collected using self-reported questionnaires administered to 246 parents of patients with DMD [29], and López-Hernández’s study which was a multistate, multiple source, retrospective study from the records of 432 patients with less than 30% of them obtaining definite DMD diagnosis, who reported a school attendance rate of 94.7% among boys with DMD [30]; this could be explained that our domestic schools are not ideally equipped to accommodate the needs of this type of disability [30, 31]. There was also a statistically significant difference in parental consanguinity showing 20% of cases with 1st degree consanguinity compared to 0% in the control group. A statistical significance was also evident in speech development between cases and control with 92% of the control group having normal speech development compared to only 40% of cases; this was consistent with Thangarajh and his team who evaluated 196 steroid naïve with dystrophinopathy, with the concerns and adjustment challenges analyzed in relation to DMD medication; found neurodevelopmental concerns were reported in 4 domains; and found that 39% of boys had speech delay with their mean age of speech onset at 28 months (range 7–66 months) [32], and in line with A. J. Darmahkasih’s study that was a retrospective case series of neurodevelopmental and behavioral/emotional symptoms obtained through review of systems of 700 DMD patients in relation to dystrophin gene mutations which estimated (24.4%) language/speech delays in DMD boys [33].
When comparing between the two groups regarding Full Scale IQ (FSIQ), our results showed that there the TIQ median in the case group was much lower than in control that indicates lower IQ in DMD compared to general population which matched the findings of the study by Orsini and his colleagues [3]. Moreover, we found that these findings presented in TIQ and all its subsets except similarities as the median of the case group were 82 in comparison to 94 in the control group, with those with <90 TIQ represented 58% of DMD boys with those less than 80 representing 40% of cases. The lowest scores in DMD boys were in general comprehension and vocabulary with a median of 6 and digit span with a mean of (6±2), which indicates more affection in their ability to understand complex questions, formulating answers, and ability to acquire, retain, and retrieve information, verbal expression, and working memory; these may suggest that these children have specific cognitive deficits as opposed to a global intellectual deficit. These findings were consistent with R. D’Alessandro and his colleagues who performed a cross-sectional study of 43 pediatric patients, affected by six neuromuscular diseases, 15 of which had DMD, and found that on Wechsler scales, lower FSIQ scores were seen in DMD patients, and 27% had an intellectual disability (ID) [34]. Also, in M. Mahadevappa’s study which evaluated genotype–phenotype correlations in DMD and BMD patients enrolled in the Canadian Neuromuscular Disease Registry from 2012 to 2019 with data from 342 DMD patients with genetic test results, after analysis, their results showed that boys with DMD had a significantly lower IQ (88.5). Verbal IQ (86.59) was found to be lower than Performance IQ (92.64) [35].
Authors of this study also found that patients with DMD have a higher prevalence of psychiatric disorders than the control group which was consistent with C. Pascual-Morena’s study who conducted a meta-analysis of twenty-three studies of individuals with DMD or BMD that estimated the prevalence of ASDs, ADHD, depression, anxiety disorders, and OCD in each population [30] and Orsini and his team’s findings who conducted a literature search up to October 2017 exploring cognitive impairment in neuromuscular disease [3]. Moreover, during comparison of both groups in the presence of different psychiatric disorders, there was a significant difference between the 2 groups as the case group had 19 boys (38%) ADHD compared to 10 boys (20%) of the control group, with the case group having the lowest score in oppositionality. Also, we found a significant difference in MDD as 11 boys (22%) of the case group compared to 2 boys (4%) in the control group, of those with MDD in the case group 7 boys had moderate depression, 3 had mild depression while only 1 had severe depression. Yet, only 3 (6%) of the case group had positive CARS, 14% had anxiety which was equal in both groups, and no cases or controls had OCD. This was partially consistent with C. Pascual-Morena and his colleagues who showed a prevalence of 7% ASDs, yet the same study showed prevalence of 18% of ADHD, 11% of depression, 24% of anxiety disorders, and 12% of OCD [30]. Also, A. J. Darmahkasih and his team indicated DMD patients’ inattention/hyperactive features (31.4%) and obsessive and compulsive features (25.0%) [33], and R. Banihani’s study who performed a rretrospective cohort of 59 boys investigating the cognitive and neurobehavioral profile of boys with Duchenne muscular dystrophy found attention-deficit/hyperactivity disorder in 32% of DMD patients; autism spectrum disorders in 15%; and anxiety in 27% [7]; the prevalence differences between studies may be due to randomization of the sample, different sample sizes, and different psychologists performing the assessment.
Moreover, we found that 92% of cases had deletion mutations. The most common genetic mutation present in our sample was deletion of exon 45–51 which represented 46% of our cases. Most other mutations present ranged from 2 to 6%. This was partially consistent with Kumar and his colleagues who identified large mutations and stated that the DMD gene showed deletion (66%) and duplication (7.5%) mutations in the majority of the patients [36]. Moreover, Bladen and team revealed the DMD gene has major deletion mutations in 68% of patients and large duplication mutations in 11% of patients [37]; different sample size and different countries may contribute to the percentage difference between studies, while all agree in that in general deletion mutations were the most prevalent.
In the distribution of patients within the case group regarding disrupted dystrophin gene isoforms, we found that 100% of our cases have disrupted Dp427m isoform, while addition of Dp260 was present in 86% of cases, Dp140utr was disrupted in 76%, and Dp140pc was present in 64% of cases, with Dp71 only disrupted in 10% of the case group. This was partially consistent with Doorenweerd N.’s who reviewed the latest findings on dystrophin isoform expression in the brain; specific DMD-associated learning and behavioural difficulties; and imaging and spectroscopy findings relating to brain structure, networks, perfusion, and metabolism, and identified that among the patients, half were missing only Dp427 while the other half were missing both Dp427 and Dp140; this may be also caused by different sampling, sample size, or patient’s origin [2].
Conclusions
In whole, we came to a conclusion that according to our findings, we confirmed the decrease in cognition in DMD and the increased prevalence of psychiatric disorders compared with healthy controls. Also, school attendance and speech development are more affected in DMD patients compared to controls, with more speech delay and dropping out of school. So, the authors of this study recommend establishing cognitive and psychiatric screening as a routine in the evaluation and follow-up of DMD children.
Strength
-
To our knowledge this is the first Egyptian study to describe the cognitive and neurobehavioral patterns in DMD.
-
Our study helped many families identify the importance of psychiatric assessment in DMD patients.
Limitations
-
The motor disability made it difficult for a number of patients to attend the assessment.
-
Lack of parental psychoeducation about the needs for psychiatric assessment in patients with DMD.
Availability of data and materials
Not available.
Abbreviations
- DMD:
-
Duchenne muscular dystrophy
- WISC-IV:
-
The Wechsler Intelligence Scale for Children
- BVRT:
-
Benton Visual Retention Test
- MINI KID:
-
The Mini International Neuropsychiatric Interview for children and adolescents
- CPRS-R:L:
-
Conners’ Parent Rating Scale-Revised: Long Version
- CDI:
-
Children Depression Inventory
- CARS:
-
The Childhood Autism Rating Scale
- TMAS:
-
The Taylor Manifest Anxiety Scale
- CY-BOCS:
-
Children Yale-Brown Obsessive Compulsive Scale
- ADHD:
-
Attention-deficit/hyperactivity disorder
- ASD:
-
Autism spectrum disorder
- MDD:
-
Major depressive disorder
- TIQ:
-
Total IQ
- VIQ:
-
Verbal IQ
- PIQ:
-
Performance IQ
- DYS:
-
Dystrophin
- CNS:
-
Central nervous system
- DGC:
-
Dystrophin-glycoprotein complex
- GABAA:
-
Gamma-aminobutyric acid type A
- BBB:
-
Blood brain barrier
- MLPA:
-
Multiplex ligation-dependent probe amplification
- MRCE:
-
Medical Research Centre of Excellence
- SPSS 25:
-
Statistical Package for the Social Sciences
- IQR:
-
Interquartile range
- FSIQ:
-
Full Scale IQ
- BMD:
-
Becker muscular dystrophies
References
Okubo M, Minami N, Goto K, Goto Y, Noguchi S, Mitsuhashi S, Nishino I (2016) Genetic diagnosis of Duchenne / Becker muscular dystrophy using next-generation sequencing : validation analysis of DMD mutations. J Hum Genet 61:483–489. https://doi.org/10.1038/jhg.2016
Doorenweerd N (2020) Combining genetics, neuropsychology and neuroimaging to improve understanding of brain involvement in Duchenne muscular dystrophy - a narrative review. Neuromuscul Disord 30:437–442. https://doi.org/10.1016/j.nmd.2020.05.001
Orsini M, Carolina A, de Ferreira AF, de Assis ACD, Magalhães T, Teixeira S, Bastos VH, Marinho V, Oliveira T, Fiorelli R, Oliveira AB, de Freitas MRG (2018) Cognitive impairment in neuromuscular diseases: a systematic review. Neurol Int 10:7473. https://doi.org/10.4081/ni.2018.7473
Preethish-Kumar V, Shah A, Polavarapu K, Kumar M, Safai A, Vengalil S, Nashi S, Deepha S, Govindaraj P, Afsar M, Rajeswaran J, Nalini A, Saini J, Ingalhalikar M (2022) Disrupted structural connectome and neurocognitive functions in Duchenne muscular dystrophy: classifying and subtyping based on Dp140 dystrophin isoform. J Neurol 269:2113–2125. https://doi.org/10.1007/s00415-021-10789-y
Rae MG, O’Malley D (2016) Cognitive dysfunction in Duchenne muscular dystrophy: a possible role for neuromodulatory immune molecules. J Neurophysiol 116:1304–1315. https://doi.org/10.1152/jn.00248.2016
Connolly AM, Florence JM, Cradock MM, Malkus EC, Schierbecker JR, Siener CA, Wulf CO, Anand P, Golumbek PT, Zaidman CM, Philip Miller J, Lowes LP, Alfano LN, Viollet-Callendret L, Flanigan KM, Mendell JR, McDonald CM, Goude E, Johnson L, Nicorici A, Karachunski PI, Day JW, Dalton JC, Farber JM, Buser KK, Darras BT, Kang PB, Riley SO, Shriber E, Parad R, Bushby K, Eagle M (2013) Motor and cognitive assessment of infants and young boys with Duchenne muscular dystrophy: results from the Muscular Dystrophy Association DMD Clinical Research Network. Neuromuscul Disord 23:529–539. https://doi.org/10.1016/j.nmd.2013.04.005
Banihani R, Smile S, Peds DM, Yoon G, Dupuis A, Mosleh M, Snider A, Mcadam L (2015) Cognitive and neurobehavioral profile in boys with Duchenne muscular dystrophy. J Child Neurol 30:1472–1482. https://doi.org/10.1177/0883073815570154
Snow WM, Anderson JE, Jakobson LS (2013) Neuroscience and biobehavioral reviews neuropsychological and neurobehavioral functioning in Duchenne muscular dystrophy: A review. Neurosci Biobehav Rev 37:743–752. https://doi.org/10.1016/j.neubiorev.2013.03.016
Hinton V, Fee R, Goldstein E, De Vivo D (2007) Verbal and memory skills in males with Duchenne muscular dystrophy. Dev Med Child Neurol 49:123–128. https://doi.org/10.1111/j.1469-8749.2007.00123
Poysky J (2007) Behavior patterns in Duchenne muscular dystrophy: report on the Parent Project Muscular Dystrophy behavior workshop 8-9 of December 2006, Philadelphia, USA. Neuromuscul Disord 17:986–994
Cotton SM, Voudouris NJ, Greenwood KM (2005) Association between intellectual functioning and age in children and young adults with Duchenne muscular dystrophy: further results from a meta-analysis. Dev Med Child Neurol 47:257–265. https://doi.org/10.1111/j.1469-8749.2005.tb01131
Gocheva V, Schmidt S, Orsini A-L, Hafner P, Schaedelin S, Weber P, Fischer D (2019) Psychosocial adjustment and parental stress in Duchenne muscular dystrophy. Eur J Paediatr Neurol 23:832–841. https://doi.org/10.1016/j.ejpn.2019.09.008
Taylor PJ, Betts GA, Maroulis S, Gilissen C, Pedersen RL, Mowat DR, Johnston HM, Buckley MF (2010) Dystrophin gene mutation location and the risk of cognitive impairment in Duchenne muscular dystrophy. PLoS One 5:e8803
Wechsler D (2003) Wechsler Intelligence Scale for Children-Fourth Edition: Technical and interpretative manual. The Psychological Corporation, San Antonio
Benton AL (1974) Visual retention test. Psychological Corporation New York, NY
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59:22–33
Ghanem MH, Ibrahim M, El Behairy AA, El Merghany H (1999) Mini International Neuropsychiatric Interview for children/adolescents (MINI Kid); Arabic version. Egypt Dep Neuropsychiatry, Ain Shams University, Cairo
Conners CK (1999) Conners Rating Scales-Revised. Conners, C K (1999) Conners Rat Scales-Revised. In: Maruish ME (ed) use Psychol Test Treat Plan outcomes Assess. Lawrence Erlbaum Assoc Publishers, pp 467–495
El Sheikh MM, Sadek A, Omar AN, El Nahass G (2003) Psychiatric morbidity in first degree relatives of a sample of ADHD children. MD Thesis. Fac Med Ain Shams University
Carey MP, Faulstich ME, Gresham FM, Ruggiero L, Enyart P (1987) Children’s Depression Inventory: construct and discriminant validity across clinical and nonreferred (control) populations. J Consult Clin Psychol 55:755
Ghareeb GA, Beshai JA (1989) Arabic version of the Children’s Depression Inventory: Reliability and validity. J Clin Child Psychol 18:323–326
Schopler E, Reichler RJ, Renner BR (2010) The childhood autism rating scale (CARS). WPS, Los Angeles
Alqahtani M (2017) كارز-2مقيـاس تقييم التوحد للطفولة --ST Arabic adaptations of The Childhood Autism Rating Scale (CARS-2-ST)
Mayzner MS Jr, Sersen E, Tresselt ME (1955) The Taylor Manifest Anxiety Scale and Intelligence. J Consult Psychol 19:401–403
Abdel-Khalek A (1989) The development and validation of an Arabic form of the STAI: Egyptian results. Pers Individ Differ 10:277–285. https://doi.org/10.1016/0191-8869(89)90100-1
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF (1997) Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852
Okasha A, Ragheb K, Attia AH, Seif el Dawla A, Okasha T, Ismail R (2001) Prevalence of obsessive compulsive symptoms (OCS) in a sample of Egyptian adolescents. Encephale 27:8–14
Abbs S, Tuffery-Giraud S, Bakker E, Ferlini A, Sejersen T, Mueller CR (2010) Best Practice Guidelines on molecular diagnostics in Duchenne/Becker muscular dystrophies. Neuromuscul Disord 20:422–427. https://doi.org/10.1016/j.nmd.2010.04.005
Magliano L, D'Angelo MG, Vita G, Pane M, D'Amico A, Balottin U, Angelini C, Battini R, Politano L, Patalano M, Sagliocchi A, Civati F, Brighina E, Vita GL, Messina S, Sframeli M, Lombardo ME, Scalise R, Colia G, Catteruccia M et al (2014) Psychological and practical difficulties among parents and healthy siblings of children with Duchenne vs. Becker muscular dystrophy: an Italian comparative study. Acta Myol 33(3):136–143
Pascual-Morena C, Cavero-Redondo I, Reina-Gutiérrez S, Saz-Lara A, López-Gil JF, Martínez-Vizcaíno V (2022) Prevalence of neuropsychiatric disorders in Duchenne and Becker muscular dystrophies: a systematic review and meta-analysis. Arch Phys Med Rehabil. https://doi.org/10.1016/j.apmr.2022.05.015
López-Hernández LB, Gómez-Díaz B, Escobar-Cedillo RE, Gama-Moreno O, Camacho-Molina A, Soto-Valdés DM, Anaya-Segura MA, Luna-Padrón E, Zúñiga-Guzmán C, Lopez-Hernández JA, Vázquez-Cárdenas NA, Sánchez-Chapul L, Rangel-Villalobos H, Canto P, López-Cardona MG, García S, Méndez-Covarrubias G, Coral-Vázquez RM (2014) Duchenne muscular dystrophy in a developing country: challenges in management and genetic counseling. Genet Couns 25:129–141
Thangarajh M, Hendriksen J, McDermott MP, Martens W, Hart KA, Griggs RC, TREAT-NMD MSG (2019) Relationships between DMD mutations and neurodevelopment in dystrophinopathy. Neurology 93:e1597–e1604. https://doi.org/10.1212/WNL.0000000000008363
Darmahkasih AJ, Rybalsky I, Tian C, Shellenbarger KC, Horn PS, Lambert JT, Wong BL (2020) Neurodevelopmental, behavioral, and emotional symptoms common in Duchenne muscular dystrophy. Muscle Nerve 61:466–474. https://doi.org/10.1002/mus.26803
D’Alessandro R, Ragusa N, Vacchetti M, Rolle E, Rossi F, Brusa C, Davico C, Vitiello B, Mongini T, Ricci FS (2021) Assessing cognitive function in neuromuscular diseases: a pilot study in a sample of children and adolescents. J Clin Med 10:4777
Mahadevappa M, Sekar D, Purushottam M, Thomas PT, Nalini A, Work PS (2020) Duchenne muscular dystrophy and Becker muscular dystrophy confirmed by multiplex ligation-dependent probe amplification: genotype-phenotype correlation in a large cohort. Duchenne Muscular Dystrophy 13:71
Kumar SH, Athimoolam K, Suraj M, Das Christu Das MS, Muralidharan A, Jeyam D, Ashokan J, Karthikeyan P, Krishna R, Khanna-Gupta A, Bremadesam Raman L (2020) Comprehensive genetic analysis of 961 unrelated Duchenne muscular dystrophy patients: focus on diagnosis, prevention and therapeutic possibilities. PLoS One 15:e0232654. https://doi.org/10.1371/journal.pone.0232654
Bladen CL, Salgado D, Monges S, Foncuberta ME, Kekou K, Kosma K, Dawkins H, Lamont L, Roy AJ, Chamova T, Guergueltcheva V, Chan S, Korngut L, Campbell C, Dai Y, Wang J, Barišić N, Brabec P, Lahdetie J, Walter MC, Schreiber-Katz O, Karcagi V, Garami M, Viswanathan V, Bayat F, Buccella F, Kimura E, Koeks Z, van den Bergen JC, Rodrigues M, Roxburgh R, Lusakowska A, Kostera-Pruszczyk A, Zimowski J, Santos R, Neagu E, Artemieva S, Rasic VM, Vojinovic D, Posada M, Bloetzer C, Jeannet P-Y, Joncourt F, Díaz-Manera J, Gallardo E, Karaduman AA, Topaloğlu H, El Sherif R, Stringer A, Shatillo AV, Martin AS, Peay HL, Bellgard MI, Kirschner J, Flanigan KM, Straub V, Bushby K, Verschuuren J, Aartsma-Rus A, Béroud C, Lochmüller H (2015) The TREAT-NMD DMD Global Database: analysis of more than 7,000 Duchenne muscular dystrophy mutations. Hum Mutat 36:395–402. https://doi.org/10.1002/humu.22758
Acknowledgements
The authors want to thank all patients who participated in this study, also the authors are thankful to Dr. Omnia Ahmed for her participation in performing the psychological assessment for the participants.
Funding
The research was totally funded by the researchers.
Author information
Authors and Affiliations
Contributions
The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study conformed to the standards of the Ethical Review Committee, Ain Shams University (FWA 000017585) and the scientific committee of neuropsychiatric department. Before enrollment in the study, after fully describing the objectives and results of the study, participants signed a written informed consent. The anonymity of the subjects was ensured, and all data were stored on a password protected computer in a locked office of the research team and access was strictly limited to study investigators.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sayed, M.M., Fahmy, N.A., El Habiby, M.M.M. et al. Cognitive and neurobehavioral patterns in a sample of Egyptian patients genetically diagnosed with Duchenne muscular dystrophy. Middle East Curr Psychiatry 29, 76 (2022). https://doi.org/10.1186/s43045-022-00242-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-022-00242-9