Abstract
Background
Echocardiographic prognostic indicators of precapillary pulmonary hypertension (PH) mortality has been inconclusive. This study aims to examine the prognostic values of right ventricular echocardiographic functional parameters in predicting precapillary PH mortality.
Methods
Systematic searches were conducted in the ScienceDirect, Medline, and Cochrane databases for longitudinal studies. Assessments included means and hazard ratios (HRs) for Tricuspid Annular Plane Systolic Excursion (TAPSE), Right Ventricular Systolic Pressure (RVSP), Right Ventricular Longitudinal Strain (RVLS), Right Ventricular Fractional Area Change (RVFAC), Right Ventricular Ejection Fraction (RVEF), and Right Ventricular Index of Myocardial Performance (RIMP).
Results
The meta-analysis included 24 cohort studies comprising 2171 participants. Mean values were as follows: TAPSE 17.62 mm, RVSP 77.50 mmHg, RVLS − 16.78%, RVFAC 29.81%, RVEF 37.56%, and RIMP 0.52. TAPSE (HR: 1.28; 95% CI 1.17–1.40; p < 0.001), RVLS (HR: 1.74; 95% CI 1.34–2.26; p < 0.001), RVFAC (HR: 1.40; 95% CI 1.13–1.75; p < 0.001), RVEF (HR: 1.08; 95% CI 1.02–1.15; p = 0.01), and RIMP (HR: 1.51; 95% CI 1.23–1.86; p < 0.001) emerged as significant prognosticators of precapillary PH mortality, with the exception of RVSP (HR: 1.04; 95% CI 0.99–1.09; p = 0.14). TAPSE summary receiver operating characteristics (sROC) analysis yielded an area under the curve (AUC) of 0.85 [95% CI 0.81–0.88] with a sensitivity of 0.81 [95% CI 0.63–0.91] and a specificity of 0.74 [95% CI 0.54–0.87]. RVLS sROC resulted in an AUC of 0.74 [95% CI 0.70–0.78] with a sensitivity of 0.74 [95% CI 0.57–0.86] and a specificity of 0.69 [95% CI 0.64–0.75].
Conclusions
TAPSE, RVLS, RVFAC, RVEF, and RIMP demonstrated promise as valuable prognostic indicators for precapillary PH mortality.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
According to the 2022 guidelines of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) for the diagnosis and treatment of pulmonary hypertension (PH), precapillary PH is defined by a mean pulmonary artery pressure (mPAP) exceeding 20 mmHg, a pulmonary artery wedge pressure (PAWP) of 15 mmHg or less, and a pulmonary vascular resistance (PVR) greater than 2 Wood units (WU) [1]. Precapillary PH encompasses the following clinical groups: Group 1 (comprising pulmonary arterial hypertension (PAH) associated with idiopathic, heritable, drug-induced, connective tissue diseases, and congenital heart diseases), Group 3 (comprising PH associated with lung diseases and/or hypoxia), Group 4 (pulmonary hypertension associated with chronic pulmonary artery obstruction), and Group 5 (comprising those with unclear and multifactorial mechanisms). Postcapillary PH, on the other hand, falls under clinical Group 2, signifying PH stemming from left heart diseases. The incidence of precapillary PH is approximately 6 cases per million adults, with a prevalence ranging from about 49 to 55 cases per million adults [2]. The mean age across studies varied between 43 and 67 years, with a predominant female gender representation ranging from 55 to 81% [3]. In recent times, there is mounting evidence, indicating that PH frequently occurs as a complication of several prevalent diseases. Importantly, the development of pulmonary hypertension in these contexts is consistently linked to the worsening of clinical symptoms and heightened mortality rate. A study demonstrated that the 15-year survival rates were 59.1% for precapillary pulmonary hypertension, 68.5% for PAH, and 44.3% for chronic thromboembolic pulmonary hypertension (CTEPH) [4].
Numerous echocardiographic indices have been suggested as potential prognostic markers in individuals with PH. Nevertheless, the majority of these indices have been derived from various heart chambers, encompassing heterogeneous groups of patients with distinct PH etiologies, insufficient assessment periods, and limited sample sizes [5]. The right ventricle (RV), the cardiac chamber directly impacted by PH, is predominantly absent from most severity classification schemes. This phenomenon may be attributed to the inherent complexity in echocardiographic assessment of the right heart, primarily owing to the intricate morphology of the RV and its physiology, which is influenced by load-dependent factors [6]. There presently exists no universally recognized standard for assessing the RV functional parameters within the realm of prognostic echocardiographic examinations [7]. In the context of PH, the echocardiographic characteristics and behavior of the RV are frequently overlooked by attending physicians, resulting in the omission of valuable and consistent data.
While awareness, diagnosis, and clinical management of precapillary PH have greatly improved over the past few decades, there is still a lack of consensus in the scientific community on which estimates could reflect the prognosis. In essence, this meta-analysis addresses the absence of mortality prediction tools in precapillary PH, offering valuable RV echocardiographic insights that can significantly enhance patient care and outcomes in this clinical context.
Methods
Study design and inclusion criteria
This meta-analysis strictly adhered to the PRISMA guidelines, ensuring a methodical and comprehensive approach. The study protocol was registered and approved in advance in the PROSPERO database (ID: CRD42023461510) before initiating the systematic search. The inclusion criteria were meticulously defined, focusing on both retrospective and prospective cohort studies that specifically examined the prognostic value of RV functional parameters in patients with precapillary PH. The entire process, from conducting the literature search to extracting data and assessing potential biases, was carried out by two authors. Any discrepancies or uncertainties regarding the eligibility of studies were thoughtfully resolved through consensus, involving an additional author in the decision-making process.
The inclusion criteria comprised several key aspects: The studies had to evaluate at least one prognostic parameter, involve patients with mean age at least 40 years, follow up with patients for no less than 6 months, and perform echocardiographic assessments using three-dimensional speckle tracking echocardiography within 1 week of diagnosing precapillary PH. PH participants incorporated into the research were exclusively categorized within groups 1, 3, and 4. Group 5 PH was omitted due to its inclusive nature, encompassing both precapillary and postcapillary forms, typically characterized by multifactorial etiologies. Studies with less than a 6-month follow-up duration, those involving pediatric populations, participants who had undergone chemotherapy, individuals with autoimmune or psychiatric conditions, and studies lacking data on hazard ratios (HRs) were excluded from the analysis. Moreover, studies focusing on patients with group 2 PH were excluded due to its postcapillary nature, ensuring a more homogeneous study population. Furthermore, ethical approval for patient enrollment at all participating sites was obtained from the relevant institutional review boards.
Literature search and selection
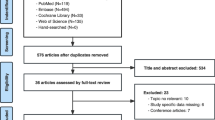
A comprehensive and systematic literature search was carried out, employing the ScienceDirect, Medline, and Cochrane databases, spanning from January 2002 to December 2023. Language restrictions were intentionally omitted during the search process. The search strategy encompassed both Medical Subject Headings (MeSH) terms and pertinent free-text keywords germane to the subject of inquiry. From the initial pool of 1,957 retrieved manuscripts, a total of 213 conformed to the pre-established inclusion criteria, as delineated in the PRISMA flowchart (Fig. 1). Additionally, a meticulous manual examination of the references within the identified studies was conducted to ensure the comprehensiveness of the search and to identify any ancillary literature germane to the subject matter. Ultimately, 24 studies were deemed suitable for incorporation into the quantitative analysis [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
Quality assessment of included studies
A thorough evaluation of potential bias was systematically conducted employing the cohort subscale of the Newcastle–Ottawa Scale (NOS) (Supplementary File 1), encompassing nine critical components. This comprehensive tool evaluates various facets of each study, comprising but not limited to selection bias, comparability bias, and outcome bias. This multifaceted approach took into account pivotal considerations, including the study design, limitations, consistency, directness, and precision of the studies, as well as the potential risk of publication bias.
Data extraction
A thorough and systematic data extraction process was meticulously executed to compile comprehensive demographic, baseline characteristics, and outcome-related data from the included studies. This process entailed a detailed assessment of key parameters, encompassing the country of origin for each study, the total study population, mean age, percentage of female participants, New York Heart Association (NYHA) functional class (FC), World Health Organization (WHO) FC, 6-min walking distance (6MWD), mean pulmonary arterial pressure (mPAP), and the duration of follow-up periods. The research outcomes were predicated on pivotal indicators, specifically, the means and hazard ratios (HRs) of various RV functional parameters, including Tricuspid Annular Plane Systolic Excursion (TAPSE), Right Ventricular Systolic Pressure (RVSP), Right Ventricular Longitudinal Strain (RVLS), Right Ventricular Fractional Area Change (RVFAC), Right Ventricular Ejection Fraction (RVEF), as well as the Right Ventricular Index of Myocardial Performance (RIMP).
A pooled analysis of summary receiver operating characteristics (sROC) curves was conducted, yielding the pooled area under the curve (AUC), sensitivity (%), and specificity (%). Additionally, Kaplan–Meier survival analysis was performed to assess mortality trends over time. Hazard ratio subgroup analyses were carried out based on specific criteria, including NYHA FC (III/IV) ≥ 50%, NYHA FC (III/IV) < 50%, WHO FC (III/IV) ≥ 50%, WHO FC (III/IV) < 50%, Group 1 PH (PH) exclusively, Group 3 and 4 PH, mPAP ≥ 50 mmHg, and mPAP < 50 mmHg subgroups for all six assessed RV functional parameters.
Data synthesis and analysis
A rigorous statistical approach ensured precise analysis. Continuous data were expressed as mean ± SD, categorical variables as absolute numbers or percentages. Data presentation, including 95% CIs, facilitated inter-study comparisons. The REML model amalgamated effect estimates, considering treatment effect variations. The Mantel–Haenszel method assessed heterogeneity, guiding model selection. Visual representation used forest, funnel, and Galbraith plots (Supplementary File 1). Stata software version 18 (StataCorp, College Station, TX, USA) conducted analyses with p < 0.05 significance. Rigorous statistics provided a nuanced exploration, contributing to evidence-based synthesis. Cumulative incidence curves depicted significant echocardiographic measures. Significant measures underwent sROC curve analysis for AUCs, sensitivity, and specificity.
Results
Study selection
The search yielded 1,957 articles, with 982 duplicates. After title and abstract screening, exclusions included medication studies (n = 982), pediatric-focused (n = 221), and those addressing multiple diseases (n = 386). Among the 213 remaining studies, 40 discussed atrial echocardiographic parameters, 102 lacked prognostic assessment, and 69 were irrelevant to precapillary PH. Full-text screening of the remaining 25 studies resulted in the inclusion of 24 studies in the meta-analysis (Fig. 1).
Characteristics and quality assessment of included studies
The twenty-four cohort studies encompassed in this meta-analysis span the period between 2002 and 2023. These studies were conducted across a diverse array of countries, including Australia, Belgium, Brazil, China, France, Germany, Greece, Italy, Japan, the Netherlands, Romania, and the USA. Detailed patient characteristics for each of the cohort studies are presented in Table 1. The cumulative study population consisted of 2,171 patients, exhibiting an average age of 51.18 ± 14.16 years. Among these patients, women constituted 70.64%. The mean 6MWD and mPAP across the various studies were 366.07 ± 119.98 m and 51.90 ± 14.09 mmHg, respectively. Although the duration of follow-up exhibited variation among the studies, ranging from 6 to 50 months, the mean follow-up period approximated 30.42 ± 12.83 months.
Among the selected studies, four of them incorporated patients presenting with NYHA FC III/IV > 50% [11, 17, 19, 29]. In contrast, eight studies encompassed patients with WHO FC III/IV > 50% [10, 13, 16, 18, 22, 24, 26, 30]. Regarding the classification of precapillary hypertension, ten studies exclusively included patients diagnosed with Group I PH [8, 10,11,12,13, 16, 19, 26, 28, 30]. This category encompassed etiologies related to inheritable causes, medication usage, and connective tissue diseases. Furthermore, ten studies featured patients with mPAP ≥ 50 mmHg [10,11,12, 16, 17, 19, 24, 28,29,30] in their cohorts. In Supplementary File 1, we provide a summary of our quality assessment. The individual NOS scores within this cohort ranged from 7 to 8.
Mean and hazard ratios of right ventricular functional parameters
Table 2 displays the mean values and HRs for RV functional parameters concerning mortality in precapillary PH. The pooled mean values were as follows: TAPSE at 17.62 [16.77–18.47] mm, RVSP at 77.50 [69.72–85.27] mmHg, RVLS at − 16.78 [− 17.72 to − 15.84]%, RVFAC at 29.81 [27.58–32.05]%, RVEF at 37.56 [34.03–41.10]%, and RIMP at 0.52 [0.39–0.65] (Fig. 2). Despite the presence of high heterogeneity, all these values were determined to be statistically significant.
Mean values and hazard ratios of right ventricular functional parameters. A TAPSE, B RVSP, C RVLS, D RVFAC, E RVEF, F RIMP. Abbreviations: 95% CI, 95% confidence interval; HR, hazard ratio; RIMP, Right Ventricular Index of Myocardial Performance; RVFAC, Right Ventricular Fractional Area Change; RVEF, Right Ventricular Ejection Fraction; RVLS, Right Ventricular Longitudinal Strain; RVSP, Right Ventricular Systolic Pressure; TAPSE, Tricuspid Annular Plane Systolic Excursion
Concerning prognostic significance, the following parameters were identified as significant prognostic markers for mortality in precapillary PH: TAPSE (HR: 1.28; 95% CI 1.17–1.40; p < 0.001), RVLS (HR: 1.74; 95% CI 1.34–2.26; p < 0.001), RVFAC (HR: 1.40; 95% CI 1.13–1.75; p < 0.001), RVEF (HR: 1.08; 95% CI 1.02–1.15; p = 0.01), and RIMP (HR: 1.51; 95% CI: 1.23–1.86; p < 0.001). In contrast, RVSP (HR: 1.04; 95% CI 0.99–1.09; p = 0.14) was not identified as a prognostic marker of mortality (Fig. 2). Additionally, the HRs for TAPSE, RVFAC, and RVEF were inadvertently inverted during the data analysis process. Consequently, lower values of these parameters are unequivocally linked to a higher mortality risk within the context of precapillary PH. This rectification shows the inverse relationship that exists, providing a clearer understanding of the prognostic implications associated with these critical RV functional parameters.
Subgroup analyses, delineated in accordance with the aforementioned criteria, have unveiled significant insights (Table 3). While the overall prognostic potential of RVSP for mortality remains inconclusive, an intriguing exception has come to light among patients primarily classified under WHO FC III/IV (HR: 1.05; 95% CI 1.03–1.07; p < 0.001), where RVSP emerged as a noteworthy prognostic factor for mortality. Furthermore, RVFAC has exhibited augmented prognostic significance within subgroups characterized by WHO FC III/IV < 50% (HR: 1.40; 95% CI 1.10–1.78; p < 0.01), Group 1 PH (HR: 1.78; 95% CI 1.25–2.55; p < 0.001), and mPAP ≥ 50 mmHg (HR: 1.70; 95% CI 1.25–2.30; p < 0.001). Similarly, both RVEF and RIMP have demonstrated heightened prognostic capacity within the subgroup characterized by WHO FC III/IV < 50% (HR: 1.10; 95% CI 1.06–1.14; p < 0.001 and HR: 1.58; 95% CI 1.36–1.84; p < 0.001, respectively). RIMP exhibited superior predictive capabilities in the context of mortality within Group 3 and 4 PH (HR: 1.58; 95% CI 1.36–1.82; p < 0.001). Notably, the predictive value of RVEF for mortality in groups stratified by etiology and mPAP remains inconclusive due to limited data availability, with only one study analyzed for each group.
Summary receiver operating characteristics curves of TAPSE and RVLS
In pursuit of evaluating the predictive capacity of RV functional parameters concerning mortality in precapillary PH, the utilization of sROC curves was employed, as depicted in Fig. 3. The summarized ROC curve provided an overarching perspective of predictive accuracy, effectively encapsulating the delicate balance between sensitivity and specificity. In this regard, the calculated AUC for TAPSE was found to be 0.85 [0.81–0.88], signifying a commendable level of discriminatory power. TAPSE exhibited a sensitivity of 0.81 [0.63–0.91] coupled with a specificity of 0.74 [0.54–0.87], reinforcing its notable prognostic value. Conversely, for RVLS, the derived AUC amounted to 0.74 [0.70–0.78], implying a moderately robust discriminatory capability. RVLS was associated with a sensitivity of 0.74 [0.57–0.86] and a specificity of 0.69 [0.64–0.75].
Summary receiver operating characteristic curves, pooled sensitivity, specificity, and Kaplan–Meier survival analysis of A TAPSE and B RVLS. Abbreviations: 95% CI, 95% confidence interval; AUC, area under the curve; RVLS, Right Ventricular Longitudinal Strain; SENS, Sensitivity; SPEC, Specificity; sROC, Summary Receiver Operating Characteristic; TAPSE, Tricuspid Annular Plane Systolic Excursion
Kaplan–Meier survival analysis of TAPSE and RVLS
The Kaplan–Meier curves illustrating the estimated composite mortality outcomes are thoughtfully depicted in Fig. 3, stratified by TAPSE and RVLS. The duration of survival analysis for TAPSE was restricted to a maximum of 24 months, whereas studies assessing RVLS extended their data coverage to 48 months. Remarkably, the curves unveiled a compelling trend: Lower TAPSE values and higher RVLS values were conspicuously associated with diminished cumulative survival rates in contrast to their respective counterparts. This underscores the potential prognostic significance of these parameters in gauging the mortality risk for individuals grappling with precapillary PH.
Discussion
To the extent of our knowledge, this is the first systematic review and meta-analysis that reports the significance of various right ventricular echocardiographic parameters as prognostic tools among a relatively large cohort of precapillary PH patients. It is also evident that TAPSE, RVLS, RVFAC, RVEF, and RIMP all emerge as reliable predictors of mortality based on our analysis of pooled HR from the studies. In precapillary PH, survival is contingent on right ventricular dysfunction, a consequence of increased pulmonary vascular resistance. The compensatory mechanisms of the heart, such as hypertrophy or increased contractility, become maladaptive, ultimately failing to counteract the elevated pressure load [32].
TAPSE
TAPSE involves the use of an M-mode ultrasound technique within an apical four-chamber view to assess the longitudinal displacement of the tricuspid ring in the right ventricle. Our analysis has shown that TAPSE is markedly reduced in patients with precapillary PH. This observation aligns with the research conducted by Forfia et al., and a TAPSE lower than 1.8 cm is associated with a lower right ventricular function [15]. This result may be attributed to the increased right ventricular pressure load, which leads to a reduced level of systolic excursion and, consequently, a decrease in ejection fraction [33]. Our analysis demonstrated a robust link between decreased TAPSE and mortality in precapillary PH patients, indicating a 38% higher hazard of mortality in individuals with PH. This includes a comprehensive sROC analysis of TAPSE, emphasizing its prognostic value with 81% sensitivity and 74% specificity. Kaplan–Meier survival analysis over twelve months highlighted TAPSE as the most significant prognostic factor. This finding is consistent with the results of a meta-analysis conducted by Meijerink et al., which similarly demonstrated a correlation between reduced TAPSE and increased mortality [34]. In addition, a recent meta-analysis by Baggen et al. also established decreased TAPSE as a reliable prognostic tool in patients with PH [35]. Interestingly, a study identified a nonsignificant association between TAPSE and all-cause mortality [9]. Despite unclear contributors to this disparity in consolidated findings, subgroup analysis consistently identifies TAPSE as a reliable prognostic tool across subgroups. Emphasizing TAPSE's clinical significance, this echoes its crucial role in predicting adverse outcomes, particularly mortality, in precapillary pulmonary hypertension, while evaluating right ventricular function.
RVSP
RVSP, a crucial echocardiographic parameter for PH screening, estimates PASP by measuring tricuspid regurgitant jet velocity. Our analysis showed a substantial RVSP increase in PH patients (mean value: 77.5 mmHg). Bossone et al. established a key PASP cutoff (36 mmHg), highlighting a significant RVSP disparity between normal individuals and those with PH [36]. Furthermore, a cohort study conducted by Strange et al. found that a RVSP over 30 mmHg was significantly associated with increased 1-year and 5-year mortality [36]. RVSP's potential as a diagnostic tool for pulmonary hypertension is noted. Despite reported high sensitivity and specificity, its inconsistencies imply unreliability as a diagnostic parameter. Surprisingly, our analysis found no statistically significant association between RVSP and mortality, contrary to Corciova et al.'s study, which reported a significant correlation between PASP and mortality [37]. In a recent meta-analysis conducted by Prosperi-Porta et al., it was observed that a 10 mmHg increment in PASP is associated with a 1.5-fold increase in the likelihood of adverse events [38]. Conversely, multiple studies have indicated that the ratio of TAPSE, RVEF, or RVFAC to PASP represents a more dependable prognostic tool for predicting mortality in patients with PH. This is attributed to the capacity of right ventricular–arterial coupling to effectively reflect right ventricular afterload and contractility [6, 39]. These findings suggest that the use of multiple echocardiographic parameters may improve the predictive value for adverse outcomes and mortality in patients with PH. Notably, within our subgroup analysis, we found a strong correlation between RVSP and patients with PH categorized as the WHO FC III/IV. In the advanced stages of PH, patients face an elevated risk of experiencing adverse outcomes as a consequence of their hemodynamic instability [40, 41]. This instability, driven by vascular changes and impaired pulmonary compliance, leads to elevated resistance, straining the right ventricle, causing systemic congestion and inflammation, contributing to higher mortality in advanced PH.
RVLS
The well-established link between reduced RVLS and higher mortality in PH patients establishes RVLS as a valuable mortality prognostic tool. Calculated by averaging strain in six right ventricular segments, RVLS reflects both global and regional systolic function in the context of PH [42]. Through our analysis, it was evident that patients with PH have a higher or less negative RVLS value compared to normal patients with a mean value of − 16.78%. This is attributed to the increased right ventricular mechanical stress and increased contractile required for effective ejection in PH patients [32]. Our analysis has revealed that an elevated RVLS is linked to a 74% increased risk of mortality, with corresponding sensitivity and specificity values of 74% and 69%. These findings suggest that when compared to TAPSE, RVLS may have a comparatively lower significance as a prognostic factor in patients with precapillary PH. Similar to TAPSE, the disparity in survival between patients with higher RVLS and the control group is most pronounced at the twelve-month mark. A meta-analysis by Shukla et al. reported a significantly higher HR of 3.78 in patients with an RVLS of > − 20% [43]. The differences in findings might be attributed to the use of a specific cutoff value, a criterion that we did not utilize in our analysis. In addition, our finding is consistent with a study conducted by Focardi et al., which highlighted that RVLS can predict right ventricular performance, thus playing a crucial role in determining the mortality risk among individuals with PH [44]. Other studies have also reported positive correlation between RVLS and all-cause mortality [45, 46]. Ultimately, this meta-analysis further strengthens the existing body of literature surrounding the utilization of RVLS as a prognostic parameter in individuals with PH.
RVFAC
RVFAC is an index of global systolic performance and contractility, as it measures the percentage of change in the area of right ventricle during systole and diastole [42]. We found that RVFAC is markedly diminished in PH patients with a mean value of 29.81%. Nonetheless, as indicated by a study by Slegg et al., it is important to note that the normal reference values for RVFAC differ by gender, with a threshold of < 30% for males and < 35% for females. Moreover, RVFAC interestingly exhibits a statistically significant reduction in patients diagnosed with precapillary PH [47]. In PH, elevated pulmonary vascular resistance increases the right ventricular afterload, demanding a higher level of contractility to maintain cardiac output. However, this adaptation may become maladaptive over time, leading to a decrease in RVFAC. A reduction in RVFAC indicates the right ventricle's inability to effectively contract, contributing to a poor prognosis. The results of our analysis revealed a strong association between reduced RVFAC and mortality in precapillary PH patients with an increased risk of mortality by 40%. Teramoto et al. conducted a study, reporting a noteworthy correlation between an RVFAC value < 25.5% and all-cause mortality in patients with PH [48]. Nevertheless, further investigations are warranted to establish the precise cutoff value that consistently holds prognostic significance. In patients with WHO FC III/IV < 50%, Group 1 PH, and mPAP ≥ 50 mmHg, RVFAC exhibited heightened prognostic significance.
RVEF
The assessment of RVEF involves calculating the volume of blood expelled from the right ventricle during systole compared to the total end-diastolic volume [42]. In our analysis, we observed the prognostic significance of RVEF in a specific subgroup, specifically those in which less than 50% of the patients were classified under WHO FC III/IV. This result may be due to the advanced disease state in this subgroup, where right ventricular dysfunction plays a more critical role in prognosis. A very recent meta-analysis by Kitano et al. has reported that a pooled HR of 2.54 for RVEF in patients with PH [49]. This result contradicts our analysis, which did not show significant prognostic value for RVEF in the overall cohort. The disparity in findings underscores the complexity of RVEF's role in predicting mortality in PH and may be attributed to variations in patient characteristics, PH etiologies, and methods of RVEF measurement. Therefore, comprehensive research which includes diverse patient populations is necessary to establish a clearer understanding of its prognostic utility in the context of PH.
RIMP
Another significant echocardiographic parameter is the RIMP, also known as the Tei Index or Myocardial Performance Index. These terms are frequently used interchangeably to refer to the same parameter. Through our analysis, it was demonstrated that RIMP holds prognostic significance, particularly among patients with advanced PH in WHO FC III/IV. Interestingly, RIMP also showed superior predictive capacities of mortality within Group 3 and 4 PH, underlining its significance as a prognostic parameter. Similar with previous parameters discussed, this result may also be attributed to the increased hemodynamic instability often experienced by patients in later stages of PH. Studies surrounding the use of RIMP as a standalone parameter in predicting mortality is very limited. Intriguingly, research conducted by Grapsa et al. found that RIMP serve as a valuable prognostic factor in individuals with PH [50].
Study limitations and recommendations
The limitations of our meta-analysis should be considered. Due to the restricted availability of complete data from the included studies, our investigation used a subset of data for sROC and Kaplan–Meier analyses. The data pertaining to PVR values are absent in most studies. Although PVR is crucial in the context of precapillary PH, the lack of data precludes analysis. PVR serves as a critical measurement in differentiating between precapillary, postcapillary, and combined capillary PH. Additionally, the majority of the studies in our analysis were single-center observational retrospective in nature, which can introduce potential biases related to data collection and patient selection. Future research involving randomized controlled trials would provide a more reliable foundation for analysis. Furthermore, the lack of detailed patient-level data regarding NYHA and WHO functional class led us to determine 50% as an approximation for the majority, which might not precisely represent the entire spectrum of functional class distribution. Hence, conducting further research to address these limitations would not only enhance the precision of the results but also increase their clinical relevance and applicability in patients with PH.
Conclusions
In conclusion, right ventricular echocardiographic functional parameters, such as TAPSE, RVLS, RVFAC, RVEF, and RIMP, are substantial prognostic markers for precapillary PH mortality. The predictive value is influenced by disease severity, etiology, and mPAP. While these findings offer valuable insights, further research, including RCTs and patient-level data, is needed to enhance accuracy and clinical applicability in PH patients.
Availability of data and materials
Data available within the article. The authors confirm that the data supporting the findings of this study are available within the article.
Abbreviations
- 6MWD:
-
6-Minute walking distance
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- FC:
-
Functional class
- mPAP:
-
Mean pulmonary arterial pressure
- NYHA:
-
New York Heart Association
- PH:
-
Pulmonary hypertension
- PWP:
-
Pulmonary wedge pressure
- RHC:
-
Right heart catheterization
- RIMP:
-
Right Ventricular Index of Myocardial Performance
- RVFAC:
-
Right Ventricular Fractional Area Change
- RVEF:
-
Right Ventricular Ejection Fraction
- RVLS:
-
Right Ventricular Longitudinal Strain
- RVSP:
-
Right Ventricular Systolic Pressure
- TAPSE:
-
Tricuspid Annular Plane Systolic Excursion
References
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M et al (2022) ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2022:2200879. https://doi.org/10.1183/13993003.00879-2022
Oldroyd SH, Manek G, Sankari A, Bhardwaj A (2023) Pulmonary hypertension. StatPearls, Treasure Island
Leber L, Beaudet A, Muller A (2020) Epidemiology of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: identification of the most accurate estimates from a systematic literature review. Pulm Circ 11:2045894020977300. https://doi.org/10.1177/2045894020977300
Sugiyama Y, Tahara N, Bekki M, Tahara A, Honda A, Maeda-Ogata S et al (2020) Long-term survival outcome for pre-capillary pulmonary hypertension at a Japanese single center. Can J Physiol Pharmacol 98:644–652. https://doi.org/10.1139/cjpp-2019-0663
Grapsa J, Pereira Nunes MC, Tan TC, Cabrita IZ, Coulter T, Smith BCF et al (2015) Echocardiographic and hemodynamic predictors of survival in precapillary pulmonary hypertension. Circ Cardiovasc Imaging 8:e002107. https://doi.org/10.1161/CIRCIMAGING.114.002107
Gheorghe GS, Gheorghe ACD, Ciobanu A, Hodorogea AS (2022) Echocardiographic prognostic factors in pulmonary hypertension. In: Gaze DC (ed) Novel pathogenesis and treatments for cardiovascular disease. IntechOpen, Rijeka, p 265. https://doi.org/10.5772/intechopen.107420
de Barros JA, Sant’Ana G, Martins G, Madlum L, Scremim C, Petterle R et al (2021) Severity of precapillary pulmonary hypertension: predictive factor. Pulmonology. https://doi.org/10.1016/j.pulmoe.2021.11.007
Badagliacca R, Papa S, Valli G, Pezzuto B, Poscia R, Manzi G et al (2016) Echocardiography combined with cardiopulmonary exercise testing for the prediction of outcome in idiopathic pulmonary arterial hypertension. Chest 150:1313–1322. https://doi.org/10.1016/j.chest.2016.07.036
Butcher SC, Feloukidis C, Kamperidis V, Yedidya I, Stassen J, Fortuni F et al (2022) Right ventricular myocardial work characterization in patients with pulmonary hypertension and relation to invasive hemodynamic parameters and outcomes. Am J Cardiol 177:151–161. https://doi.org/10.1016/j.amjcard.2022.04.058
Chen S-L, Zhang J, Zhang H, Xie D-J, Zhou L, Zhang F-F et al (2017) Assessment and prognostic impact of right ventricular function in patients with pulmonary arterial hypertension undergoing pulmonary artery denervation: central role of global right ventricular longitudinal peak systolic strain*. Struct Heart 1:81–90. https://doi.org/10.1080/24748706.2017.1315204
Ciarka A, Doan V, Velez-Roa S, Naeije R, van de Borne P (2010) Prognostic significance of sympathetic nervous system activation in pulmonary arterial hypertension. Am J Respir Crit Care Med 181:1269–1275. https://doi.org/10.1164/rccm.200912-1856OC
da Costa Junior AA, Ota-Arakaki JS, Ramos RP, Uellendahl M, Mancuso FJN, Gil MA et al (2017) Diagnostic and prognostic value of right ventricular strain in patients with pulmonary arterial hypertension and relatively preserved functional capacity studied with echocardiography and magnetic resonance. Int J Cardiovasc Imaging 33:39–46. https://doi.org/10.1007/s10554-016-0966-1
Dandel M, Knosalla C, Kemper D, Stein J, Hetzer R (2015) Assessment of right ventricular adaptability to loading conditions can improve the timing of listing to transplantation in patients with pulmonary arterial hypertension. J Heart Lung Transplant Off Publ Int Soc Heart Transplant 34:319–328. https://doi.org/10.1016/j.healun.2014.11.012
Fine NM, Chen L, Bastiansen PM, Frantz RP, Pellikka PA, Oh JK et al (2013) Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging 6:711–721. https://doi.org/10.1161/CIRCIMAGING.113.000640
Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA et al (2006) Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med 174:1034–1041. https://doi.org/10.1164/rccm.200604-547OC
Ghio S, Klersy C, Magrini G, D’Armini AM, Scelsi L, Raineri C et al (2010) Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol 140:272–278. https://doi.org/10.1016/j.ijcard.2008.11.051
Giusca S, Jurcut R, Coman IM, Ghiorghiu I, Catrina D, Popescu BA et al (2013) Right ventricular function predicts clinical response to specific vasodilator therapy in patients with pulmonary hypertension. Echocardiography 30:17–26. https://doi.org/10.1111/j.1540-8175.2012.01809.x
Greiner S, Goppelt F, Aurich M, Katus HA, Mereles D (2018) Prognostic relevance of the right ventricular myo-mechanical index (RV-MMI) in patients with precapillary pulmonary hypertension. Open Heart 5:e000903. https://doi.org/10.1136/openhrt-2018-000903
Haddad F, Spruijt OA, Denault AY, Mercier O, Brunner N, Furman D et al (2015) Right heart score for predicting outcome in idiopathic, familial, or drug- and toxin-associated pulmonary arterial hypertension. JACC Cardiovasc Imaging 8:627–638. https://doi.org/10.1016/j.jcmg.2014.12.029
Haeck MLA, Scherptong RWC, Marsan NA, Holman ER, Schalij MJ, Bax JJ et al (2012) Prognostic value of right ventricular longitudinal peak systolic strain in patients with pulmonary hypertension. Circ Cardiovasc Imaging 5:628–636. https://doi.org/10.1161/CIRCIMAGING.111.971465
Hulshof HG, van Dijk AP, Hopman MTE, Heesakkers H, George KP, Oxborough DL et al (2021) 5-Year prognostic value of the right ventricular strain-area loop in patients with pulmonary hypertension. Eur Heart J Cardiovasc Imaging 22:188–195. https://doi.org/10.1093/ehjci/jeaa143
Ishii S, Minatsuki S, Hatano M, Saito A, Yagi H, Shimbo M et al (2023) The ratio of TAPSE to PASP predicts prognosis in lung transplant candidates with pulmonary arterial hypertension. Sci Rep 13:3758. https://doi.org/10.1038/s41598-023-30924-1
Li Y, Guo D, Gong J, Wang J, Huang Q, Yang S et al (2021) Right ventricular function and its coupling with pulmonary circulation in precapillary pulmonary hypertension: a three-dimensional echocardiographic study. Front Cardiovasc Med 8:690606
Mahapatra S, Nishimura RA, Oh JK, McGoon MD (2006) The prognostic value of pulmonary vascular capacitance determined by Doppler echocardiography in patients with pulmonary arterial hypertension. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 19:1045–1050. https://doi.org/10.1016/j.echo.2006.03.008
Mathai SC, Sibley CT, Forfia PR, Mudd JO, Fisher MR, Tedford RJ et al (2011) Tricuspid annular plane systolic excursion is a robust outcome measure in systemic sclerosis-associated pulmonary arterial hypertension. J Rheumatol 38:2410–2418. https://doi.org/10.3899/jrheum.110512
Moceri P, Duchateau N, Baudouy D, Schouver E-D, Leroy S, Squara F et al (2018) Three-dimensional right-ventricular regional deformation and survival in pulmonary hypertension. Eur Heart J Cardiovasc Imaging 19:450–458. https://doi.org/10.1093/ehjci/jex163
Murata M, Tsugu T, Kawakami T, Kataoka M, Minakata Y, Endo J et al (2016) Prognostic value of three-dimensional echocardiographic right ventricular ejection fraction in patients with pulmonary arterial hypertension. Oncotarget 7:86781–68790. https://doi.org/10.18632/oncotarget.13505
Park J-H, Park MM, Farha S, Sharp J, Lundgrin E, Comhair S et al (2015) Impaired global right ventricular longitudinal strain predicts long-term adverse outcomes in patients with pulmonary arterial hypertension. J Cardiovasc Ultrasound 23:91–99. https://doi.org/10.4250/jcu.2015.23.2.91
Raymond RJ, Hinderliter AL, Willis PW, Ralph D, Caldwell EJ, Williams W et al (2002) Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol 39:1214–1219. https://doi.org/10.1016/s0735-1097(02)01744-8
Sachdev A, Villarraga HR, Frantz RP, McGoon MD, Hsiao J-F, Maalouf JF et al (2011) Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest 139:1299–1309. https://doi.org/10.1378/chest.10-2015
van Kessel M, Seaton D, Chan J, Yamada A, Kermeen F, Hamilton-Craig C et al (2016) Prognostic value of right ventricular free wall strain in pulmonary hypertension patients with pseudo-normalized tricuspid annular plane systolic excursion values. Int J Cardiovasc Imaging 32:905–912. https://doi.org/10.1007/s10554-016-0862-8
Bernardo RJ, Haddad F, Couture EJ, Hansmann G, de Jesus Perez VA, Denault AY et al (2020) Mechanics of right ventricular dysfunction in pulmonary arterial hypertension and heart failure with preserved ejection fraction. Cardiovasc Diagn Ther 10:1580–1603. https://doi.org/10.21037/cdt-20-479
Spiro JR, Steeds RP (2012) Chapter 14-Echocardiography in respiratory medicine. In: Spiro SG, Silvestri GA, Agustí ABT-CRM (Fourth E) (eds). W.B. Saunders, Philadelphia, pp 193–201. https://doi.org/10.1016/B978-1-4557-0792-8.00014-3
Meijerink F, de Witte SM, Limpens J, de Winter RJ, Bouma BJ, Baan J (2022) Prognostic value of pulmonary hypertension, right ventricular function and tricuspid regurgitation on mortality after transcatheter mitral valve repair: a systematic review and meta-analysis. Heart Lung Circ 31:696–704. https://doi.org/10.1016/j.hlc.2021.11.017
Baggen VJM, Driessen MMP, Post MC, van Dijk AP, Roos-Hesselink JW, van den Bosch AE et al (2016) Echocardiographic findings associated with mortality or transplant in patients withpulmonary arterial hypertension: a systematic review and meta-analysis. Neth Heart J 24:374–389. https://doi.org/10.1007/s12471-016-0845-3
Strange G, Stewart S, Celermajer DS, Prior D, Scalia GM, Marwick TH et al (2019) Threshold of pulmonary hypertension associated with increased mortality. J Am Coll Cardiol 73:2660–2672. https://doi.org/10.1016/j.jacc.2019.03.482
Corciova FC, Arsenescu-Georgescu C (2012) Prognostic factors in pulmonary hypertension. Maedica (Buchar) 7:30–37
Prosperi-Porta G, Ronksley P, Kiamanesh O, Solverson K, Motazedian P, Weatherald J (2022) Prognostic value of echocardiography-derived right ventricular dysfunction in haemodynamically stable pulmonary embolism: a systematic review and meta-analysis. Eur Respir Rev 31:220120. https://doi.org/10.1183/16000617.0120-2022
He Q, Lin Y, Zhu Y, Gao L, Ji M, Zhang L et al (2023) Clinical usefulness of right ventricle-pulmonary artery coupling in cardiovascular disease. J Clin Med. https://doi.org/10.3390/jcm12072526
Chemla D, Castelain V, Hervé P, Lecarpentier Y, Brimioulle S (2002) Haemodynamic evaluation of pulmonary hypertension. Eur Respir J 20:1314 LP – 1331. https://doi.org/10.1183/09031936.02.00068002
Maron BA (2023) Revised definition of pulmonary hypertension and approach to management: a clinical primer. J Am Heart Assoc 12:e029024. https://doi.org/10.1161/JAHA.122.029024
Smolarek D, Gruchała M, Sobiczewski W (2017) Echocardiographic evaluation of right ventricular systolic function: the traditional and innovative approach. Cardiol J 24:563–572. https://doi.org/10.5603/CJ.a2017.0051
Shukla M, Park J-H, Thomas JD, Delgado V, Bax JJ, Kane GC et al (2018) Prognostic value of right ventricular strain using speckle-tracking echocardiography in pulmonary hypertension: a systematic review and meta-analysis. Can J Cardiol 34:1069–1078. https://doi.org/10.1016/j.cjca.2018.04.016
Focardi M, Cameli M, Carbone SF, Massoni A, De Vito R, Lisi M et al (2015) Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging 16:47–52. https://doi.org/10.1093/ehjci/jeu156
Wu VC-C, Takeuchi M (2018) Echocardiographic assessment of right ventricular systolic function. Cardiovasc Diagn Ther 8:70–79. https://doi.org/10.21037/cdt.2017.06.05
Siddiqui I, Rajagopal S, Brucker A, Chiswell K, Christopher B, Alenezi F et al (2018) Clinical and echocardiographic predictors of outcomes in patients with pulmonary hypertension. Am J Cardiol 122:872–878. https://doi.org/10.1016/j.amjcard.2018.05.019
Slegg OG, Willis JA, Wilkinson F, Sparey J, Wild CB, Rossdale J et al (2022) IMproving PULmonary hypertension screening by echocardiography: IMPULSE. Echo Res Pract 9:9. https://doi.org/10.1186/s44156-022-00010-9
Teramoto K, Sengelov M, West E, Santos M, Nadruz W, Skali H et al (2020) Association of pulmonary hypertension and right ventricular function with exercise capacity in heart failure. ESC Heart Fail 7:1635–1644. https://doi.org/10.1002/ehf2.12717
Kitano T, Nabeshima Y, Nagata Y, Takeuchi M (2023) Prognostic value of the right ventricular ejection fraction using three-dimensional echocardiography: systematic review and meta-analysis. PLoS ONE 18:e0287924. https://doi.org/10.1371/journal.pone.0287924
Grapsa I, Pavlopoulos H, Dawson D, Gibbs JSR, Nihoyannopoulos P (2007) Retrospective study of pulmonary hypertensive patients: is right ventricular myocardial performance index a vital prognostic factor? Hellenic J Cardiol 48:152–160
Acknowledgements
The authors would like to thank the Department of Cardiology and Vascular Medicine, Udayana University/Prof. Dr. I.G.N.G Ngoerah General Hospital for their support.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
BGdL was involved in investigation, validation, project administration, writing-original draft, writing-reviewing and editing, and visualization. LOSS took part in conceptualization and supervision. JCS was responsible for investigation, data curation, writing-original draft, and writing-reviewing and editing. GNPJ and AHA participated in validation and visualization. AMK contributed to conceptualization, project administration, and supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All of the authors have reviewed the final version of the manuscript and agreed to publish this manuscript.
Competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Liyis, B.G., Suastika, L.O.S., Sutedja, J.C. et al. Prognostic values of right ventricular echocardiography functional parameters for mortality prediction in precapillary pulmonary hypertension: a systematic review and meta-analysis. Egypt Heart J 76, 105 (2024). https://doi.org/10.1186/s43044-024-00539-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00539-6