Abstract
Background
A new challenge in coronary artery disease treatment has emerged, where specific populations exhibit ischemic symptoms without any obstruction in the epicardial coronary artery. Instead, they exhibit slow coronary contrast flow, referred to as coronary slow flow (CSF). This study aims to identify several predictors of CSF.
Results
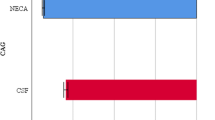
This case–control study was conducted at the Regional General Hospital of West Nusa Tenggara Province in Indonesia from December 2016 to February 2024. The study involved sixty subjects, with 30 in each group of CSF and normal epicardial coronary artery angiogram (NECA). CSF is enforced by the TIMI frame count (TFC) greater than 27 frames. Among all the predictors studied, coronary artery diameter (p < 0.001) and random blood sugar (p = 0.049) were found to affect the CSF significantly. In the multivariate analysis, coronary artery diameter remained a significant predictor (adjusted OR 10.08, 95% CI 2.64–38.50, p < 0.001), with an optimal cut-off point of more than 3.56 mm, a sensitivity of 76.7%, and a specificity of 70.7% (AUC = 0.787, p < 0.001).
Conclusion
The coronary artery diameter strongly predicts CSF in patients undergoing coronary angiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Coronary artery disease (CAD) continues to be a major contributor to mortality and morbidity worldwide, with a high prevalence rate ranging from 5 to 8% [1]. A new challenge has emerged, where specific populations exhibit ischemic symptoms, but their epicardial coronary angiography results show no obstructive signs. Instead, they exhibit slow coronary contrast flow, referred to as coronary slow flow (CSF) [2]. CSF is rare in routine coronary angiography, with an overall incidence rate ranging from 1 to 7% [3].
Tambe et al. first described the CSF phenomenon in 1972 [4,5,6]. CSF is considered an independent clinical entity that needs to be diagnosed by excluding other clinical backgrounds like coronary ectasia, coronary stenosis, coronary spasms, structural abnormalities of the heart, cardiac conduction abnormalities, and other diseases that cause rheological disorders or hemodynamic changes [4]. Despite being non-obstructive, CSF can still lead to severe clinical manifestations such as myocardial ischemia, life-threatening arrhythmias, recurrent acute coronary syndrome (ACS), and even sudden cardiac death [7]. While most patients with CSF have a relatively good prognosis, chronic and recurring angina can cause a significant decrease in their quality of life [6].
There is currently no agreement on the cause of CSF. However, the best approach involves addressing microvascular dysfunction, inflammation, abnormalities in blood cell morphology and function, platelet dysfunction, endothelial dysfunction, increased microvascular tone, and metabolic syndrome. Unfortunately, no specific CSF treatment is available currently [4, 6, 8]. It is essential to identify and manage predictors associated with CSF. However, unmasking these predictors has been challenging as studies have produced inconsistent results.
This study aims to identify several predictors of CSF compared to the normal epicardial coronary artery angiogram (NECA) group. The predictors include coronary artery diameter, red cell distribution width (RDW), platelet distribution width (PDW), mean platelet volume (MPV), neutrophil–lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), body mass index (BMI), random blood sugar (RBS), and serum creatinine levels. There has been limited research on similar lines for the Indonesian population. Therefore, this study is expected to provide a better understanding and guide for handling CSF in the future.
Methods
Study design and participants
This study was conducted at the Regional General Hospital of West Nusa Tenggara Province in Indonesia. The study was designed as a case–control study, where the subjects were divided into two groups: the CSF group and the NECA group. The CSF group was selected by identifying all CSF cases from December 2016 to February 2024. On the other hand, the NECA group was chosen as the control, based on age and sex categories that were similar to the CSF group. The study included all patients who were over 18 years of age and had undergone coronary angiography. The main indication for coronary angiography in the subjects was pectoral angina. However, patients with atrial fibrillation (AF), ejection fraction below 50%, coronary anomalies such as myocardial bridging, coronary fistula, and anomaly of the coronary ostium, those who had prior revascularization therapy such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting, and those who had undergone any previous heart surgery were excluded from the study. Both group's medical records and coronary angiography results were analyzed to collect the necessary secondary data such as essential patient information, laboratory findings, electrocardiogram, echocardiogram, and coronary angiogram.
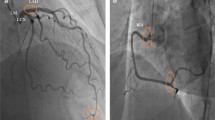
CSF is diagnosed based on the criteria established by Beltrame et al. [9] and Gibson et al. [10]. To be diagnosed with CSF, there must be no obstruction in the epicardial coronary artery and a delayed filling of the contrast agent in a distal coronary artery with a TIMI frame count (TFC) greater than 27 frames. The TFC is calculated by determining the first frame where the contrast agent has filled the entire coronary ostium in an anterograde manner and the last frame where the contrast agent reaches the distal artery. For the left anterior descending artery (LAD), a correction factor is applied by dividing the number of frames among the LAD by 1.7, resulting in the corrected TIMI frame count (cTFC). If the cTFC in LAD or the TFC in other coronary arteries is greater than 27, it is considered CSF. Two experienced interventional cardiologists blinded to the TFC and coronary artery diameter assessment take an average of the measurements.
Statistical analysis
All data collected were analyzed using the SPSS Statistics version 26 program for Mac (IBM Corp., USA). Numerical data that followed a normal distribution were presented as mean ± standard deviation (SD), while numerical data that did not follow a normal distribution were presented as median (Q1–Q3). The distribution of numerical data was tested using the Shapiro–Wilk test. Categorical data were presented as frequency (n) and percentage (%).
Statistical significance was determined using p values < 0.05. An unpaired T-test was used for numerical comparative analytical tests when the data from all groups followed a normal distribution. On the other hand, the Mann–Whitney test was used when any group had an abnormal data distribution. For categorical comparative analytical tests, the Chi-squared test was used. A logistic regression test was used for multivariate statistical analysis. In this test, independent variables were involved in a bivariate test with p-value < 0.100. Further analysis was carried out for multivariate significant predictors using the receiver operating characteristic (ROC) curve. The sensitivity and specificity of the predictor were determined, and the area under the curve (AUC) was defined. The optimal intersection point in predicting CSF events was determined using this analysis.
Results
This study involved 30 CSF participants, and it was found that the prevalence of CSF at our center was 0.8%. Additionally, 30 subjects were chosen from NECA as a control group based on age and sex characteristics (Levene's test, p = 0.954). The study participants had a mean age of 51.52 ± 8.02 years, with most being smokers (81.7%). The median BMI of the participants was 26.97 (24.01–30.89). The participants' coronary arteries had a mean TFC of 22.53 ± 7.76, and the average diameter was 3.70 ± 0.59 mm. The largest diameter was seen in the right coronary artery (RCA) (3.86 ± 0.84 mm), and only 15.0% of the participants showed tortuosity. The laboratory results indicated that the median RBS was 100.5 (95.2–120.5) mg/dL, the mean hemoglobin (Hb) was 13.90 ± 1.42 g/dL, the median platelet count was 255,950 (219,500–294,800) /uL, and the median creatinine level was 0.9 (0.8–1.1) mg/dL. The characteristics of the subjects are listed in Table 1.
In the CSF group, 53.3% of the individuals were men. The left circumflex artery (LCx) was the most commonly affected (83.3%), followed by LAD (50.0%) and RCA (43.3%). This finding corresponds with the mean TFC of LCx, which was the highest (33.08 ± 7.18). Out of the cases, 43.3% involved one vessel, 33.3% involved two vessels, and 23.3% involved three vessels. The characteristics of subjects with CSF are listed in Table 2.
There was a significant difference in the TFC between the CSF and NECA groups, with values of 29.04 ± 4.52 and 16.02 ± 3.79, respectively (p < 0.001). Only two predictors, coronary artery diameter (3.99 ± 0.53 vs. 3.41 ± 0.51, p < 0.001) and RBS (105.5 (97.0–135.0) vs. 97.5 (95.0–115.0), p = 0.049), were found to affect the CSF significantly. Multivariate logistic regression analysis was conducted on predictors with p < 0.100 values, including coronary artery diameter, RBS, and creatinine levels. It was found that only coronary artery diameter had a significant influence on CSF (adjusted OR 10.08, 95% CI 2.64–38.50, p < 0.001). These findings are listed in Table 3. Furthermore, a ROC curve analysis was performed to determine the difference between the CSF and NECA groups. The optimal cut-off point of the mean coronary artery diameter was more than 3.56 mm, with a sensitivity of 76.7% and specificity of 70.7% (AUC = 0.787, p < 0.001), shown in Fig. 1.
Discussion
In this study, the prevalence of CSF was found to be 0.8%, which is lower than the prevalence reported by Nakanishi et al. (1–7%) [3]. However, Sanati et al. also published a similar result (< 1%) [5]. The mean age of the subjects with CSF was 50.63 ± 8.09 years, with males accounting for 53.3% of the cases. Several studies have reported that men are more likely to be affected by CSF, as shown by Huang et al. (61.4%) [6] and Yang et al. (63.4%) [11]. Interestingly, this study found that age did not significantly affect the incidence of CSF (p = 0.398), consistent with several other studies [5, 12] showing that age is not a significant predictor of CSF.
Additionally, most of the subjects in this study were non-smokers (81.7%), and smoking was not found to be a significant predictor of CSF (p = 0.506). This finding is not consistent with some other studies that have shown that smoking has a significant effect, such as those conducted by Altun et al. (p = 0.031) [12], Elsanan et al. (adjusted p = 0.006) [13], and Shui et al. (p < 0.001) [14]. However, these discrepancies could be attributed to the small number of smokers in this study, which may have biased the genuine relationship between smoking and CSF.
According to this study, BMI is not a significant predictor of CSF (p = 0.344), which differs from other publications' findings. Sanati et al. (adjusted p = 0.003) [5], Huang et al. (p = 0.010) [6], and Elsanan et al. (adjusted p < 0.001) [13] have published that BMI is a strong predictor of CSF. Increasing BMI has been shown to elevate the risk of cardiovascular mortality by increasing vasoconstriction mediated by the sympathetic nervous system and systemic inflammatory processes [15, 16]. Obese populations also experience coronary microvascular abnormalities associated with endothelial dysfunction and microvascular remodeling [17]. In this study, most subjects were classified as non-obese, with a median BMI of 26.97 (24.01–30.89), which could explain the difference in findings.
The coronary artery diameter, on the other hand, significantly predicts CSF (3.99 ± 0.53 vs. 3.41 ± 0.51, p < 0.001) in this study. Even after controlling for RBS and creatinine levels, the coronary artery diameter remained a significant predictor (adjusted OR 10.08, 95% CI 2.64–38.50, p < 0.001), with an optimal cut-off point of more than 3.56 mm with a sensitivity of 76.7% and specificity of 70.7% (AUC = 0.787, p < 0.001). This finding challenges the commonly held assumption that larger coronary diameters result in reduced probabilities of myocardial ischemia. It suggests that there exists a critical threshold beyond which coronary arteries, when exceeding a certain diameter, may detrimentally impact myocardial perfusion. Yang et al.'s publication shows that mean coronary artery diameter is also a significant predictor both in bivariate analysis (5.50 ± 0.85 mm vs. 5.18 ± 0.91 mm, p < 0.001) and in multivariate logistic regression analysis (adjusted OR 2.64, 95% CI 1.54–4.51, p < 0.001) [11].
The occurrence of CSF is seen in larger coronary artery diameters, according to the laws of physics, which state that the larger the radius of the blood vessels, the slower the speed of blood flow. This is calculated by the formula Q = πr2v, where Q is constant traffic, π is a constant of 3.14, r is the radius, and v is the flow velocity [11]. However, there are variations in the location of coronary arteries involved. In this study, most CSF cases were in the LCx (83.3%), while most publications report that LAD is the most commonly affected coronary artery [3, 5, 18]. LAD is a much longer vessel than LCx and RCA, which explains why CSF is more common in LAD [10]. This study found that LCx has greater tortuosity than LAD and RCA, affecting coronary blood flow. This explanation is in line with Mihic et al.'s publication, which states that tortuosity is a significant predictor (p < 0.001) in patients with non-obstructive ischemic symptoms, and LCx is the most tortuous vessel [19].
According to this study, RBS was found to be the second most significant predictor of CSF (105.5 (97.0–135.0) vs. 97.5 (95.0–115.0), p = 0.049). However, when multivariate logistic regression analysis was conducted, RBS was no longer significant (p = 0.066). Studies have shown that blood sugar levels, as determined by the HbA1C examination, can potentiate other predictors. Elsanan et al. published that in subjects with an HbA1C > 7, the NLR (r = 0.548, p < 0.001), Hb (r = 0.382, p = 0.018), and hematocrit (r = 0.542, p < 0.001) became significant predictors [13]. Hyperglycemia conditions have been shown to disrupt the physiology of blood flow. Kersten et al. published that hyperglycemia significantly disrupts coronary collateral blood flow through nitric oxide (NO)-mediated mechanisms [20]. The findings were reinforced by Angeli et al., who mentioned that hyperglycemia interferes with NO activation and increases the production of reactive oxygen species, worsening coronary blood flow in ACS cases [21].
Blood viscosity is an essential factor that affects blood flow, with hematocrit and plasma being the primary determinants. The characteristics of red blood cells (RBC) mainly determine microcirculation blood flow, so any deformities in RBC can increase blood viscosity. Therefore, parameters such as RDW are also crucial in determining the occurrence of CSF [22]. Platelet aggregation has been shown to increase significantly in people with CSF, so the platelet size presented by MPV becomes a critical marker describing platelet activity [12]. MPV is a biomarker of platelet activity that is very useful and easy to examine. MPV was also found to be a strong and independent predictor of impaired reperfusion and 6-month mortality in ST-segment elevation myocardial infarction patients undergoing PCI, as well as the incidence of restenosis and acute stent thrombosis [23].
Certain inflammatory predictors, like PLR and NLR, are known to be related to various inflammatory diseases, including cardiovascular disease because inflammation triggers endothelial dysfunction [6, 13]. An increased PLR level can even impact the prothrombotic status, slowing down the coronary blood flow [6]. High PLR levels are associated with a higher risk of recurrence of myocardial infarction, stroke, heart failure, and no-reflow syndrome after PCI [23]. Renal dysfunction also increases the risk of cardiovascular events and worsens prognosis. It is still associated with the mechanism of endothelial dysfunction and worsening of the atherosclerosis process caused by elevated creatinine levels [6]. Endothelial dysfunction affects the decrease in nitric oxide (NO) bioactivity, directly impacting the coronary microvascular [12].
The normal values for creatinine levels, RDW, PDW, and MPV vary depending on the laboratory's examination tools. This study's normal range for creatinine levels was 0.9–1.3 mg/dL, RDW 35.0–47.0 fL, PDW 9.0–13.0 fL, and MPV 7.2–11.1 fL. Several publications have indicated that these parameters significantly impact CSF. For creatinine levels, the results were 0.9 ± 0.2 [12] and 1.17 ± 0.23 [24], RDW 13.21 ± 1.76 [24], and MPV 13.10 ± 1.72 [24] in the CSF group. However, to date, there has been no publication on the effect of PDW on CSF. NLR and PLR are reliable indicators of systemic inflammation and have been extensively studied. However, there has been no consensus on the normal values of NLR and PLR as racial variations significantly influence them. For instance, a study on normal males and females in South China found the reference range for NLR to be 0.43–2.75 and 0.37–2.87, and for PLR to be 36.63–149.13 and 43.36–172.68, respectively [25]. Another publication reports that the normal NLR values in a healthy adult Belgian population are 0.78–3.53 [26]. Meanwhile, in the Iranian population with a mean sample age of 47.9 ± 9.29 years, the mean NLR and PLR were 1.70 ± 0.70 and 117.05 ± 47.73, respectively [27]. Several publications note the significant impact of NLR and PLR on CSF, with an NLR of 1.89 ± 0.58 [11] and a median PLR of 113.11 (91.13–140.11) [6]. Unfortunately, this study found that these parameters had no significant influence on CSF. The differences in results could be due to variations in the characteristics of the population studied in this research and the comparative study. The consistency and sample size, which originated from a single center, may have contributed to the disparity in results compared to the comparative study, which involved multiple centers and a larger number of subjects.
So far, the widely accepted pathophysiological approach for dealing with the CSF has been coronary microvascular dysfunction (CMD) and coronary endothelial dysfunction (CED). However, a surprising publication by Dutta et al. suggests that in patients with angina and non-obstructed coronary arteries, CSF and cTFC are not reliable indicators of CMD or CED. They propose that the guidelines supporting the use of cTFC in diagnosing CMD need to be reassessed. According to their findings, CSF had low diagnostic accuracy for both CMD (43.4%) and CED (31.7%), with poor sensitivity of 26.7% and 21.1%, respectively. Specificity was slightly higher at 65.2% for CMD and 56.0% for CED. Furthermore, cTFC could not predict CMD or CED, as indicated by ROC analyses with an AUC of 0.41 and 0.36, respectively [28]. Therefore, additional invasive or non-invasive tools are necessary to identify this clinical phenomenon when treating patients with CSF.
It is essential to note that although AF was an exclusion criterion in this study, there is a strong connection between AF and CSF. CAD and AF can exacerbate each other because they share similar risk factors and comorbidities [29, 30]. A study by Sharma et al. revealed that CSF was present in 42% of individuals with non-valvular AF. CSF can lead to myocardial ischemia even in the absence of obstructive CAD and may also increase hospitalization rates for AF patients due to fast ventricular response [29]. Furthermore, Gao et al. found that the incidence of CSF (adjusted OR 2.122, 95% CI 1.151–3.910, p = 0.016,) was significantly higher in the intraoperative AF episode group compared to the non-episode group. The proposed mechanism suggests that the duration of AF and the left atrial diameter can impact the TFC in AF patients. Additionally, acute AF leads to an increased demand for oxygen by the atria, potentially exceeding the oxygen supply. Moreover, a significant shortening of the diastolic phase can negatively affect diastolic-dominated coronary perfusion [30].
With the cause of CSF not fully understood, treatment options are limited. Administering anti-anginal medication only provides limited clinical benefits. Extensive studies testing pharmacological approaches to CSF are still lacking and existing evidence comes only from small studies with nonuniform inclusion criteria [7]. Empirical therapies based on several aspects include improving endothelial function by controlling cardiovascular risk factors, using nitrates to dilate coronary arteries, using beta-blockers to prolong coronary perfusion time, using antiplatelets to block platelet cross-linking and aggregation, and using calcium channel blockers to dilate coronary arteries and reduce myocardial contractility [6]. Physicians also widely use nicorandil, which has been proven to improve chest pain symptoms and the impaired function of the left ventricle. This improvement may be due to its potential to increase plasma NO and reduce endothelin-1 in CSF [31]. The effectiveness of nicorandil as a treatment is even better than that of nitroglycerin [32].
However, the study had several limitations. Even though data collection covered a span of seven years, the number of CSF subjects was relatively small. The study did not take into account biomolecular predictors that could have explained the mechanisms underlying CSF. Conducted in a single center with relatively homogeneous subjects, the results may not be easily generalized to the broader population. Furthermore, various echocardiography parameters, such as diastolic function, closely related to left ventricular end-diastolic pressure and CSF, could not be analyzed due to limited secondary data documentation. Lastly, many confounding variables, such as subject comorbidities and prior treatment, could not be controlled for.
Conclusions
To summarize, the coronary artery diameter is a strong predictor of CSF in patients undergoing coronary angiography. Early medical intervention in patients with larger coronary artery diameters is expected to improve CSF outcomes significantly. However, more research is required with more subjects and multiple centers to confirm these findings.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The case report form has been stored in the hospital file.
Abbreviations
- ACS:
-
Acute coronary syndrome
- AF:
-
Atrial fibrillation
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CED:
-
Coronary endothelial dysfunction
- CMD:
-
Coronary microvascular dysfunction
- CSF:
-
Coronary slow flow
- cTFC:
-
Corrected TIMI frame count
- Hb:
-
Hemoglobin
- LAD:
-
Left anterior descending artery
- LCx:
-
Left circumflex artery
- MPV:
-
Mean platelet volume
- NECA:
-
Normal epicardial coronary artery angiogram
- NO:
-
Nitric oxide
- NLR:
-
Neutrophil–lymphocyte ratio
- PCI:
-
Percutaneous coronary intervention
- PDW:
-
Platelet distribution width
- PLR:
-
Platelet-to-lymphocyte ratio
- RBS:
-
Random blood sugar
- RCA:
-
Right coronary artery
- RDW:
-
Red cell distribution width
- TFC:
-
TIMI frame count
References
Bauersachs R, Zeymer U, Brière J-B et al (2019) Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Ther 2019:1–9. https://doi.org/10.1155/2019/8295054
Sadr-Ameli MA, Saedi S, Saedi T et al (2015) Coronary slow flow: benign or ominous? Anatol J Cardiol 15:531–535. https://doi.org/10.5152/akd.2014.5578
Nakanishi K, Daimon M (2019) Coronary slow flow and subclinical left ventricular dysfunction. Int Heart J 60:495–496. https://doi.org/10.1536/ihj.19-152
Zhu Q, Wang S, Huang X et al (2022) Understanding the pathogenesis of coronary slow flow: recent advances. Trends Cardiovasc Med. https://doi.org/10.1016/j.tcm.2022.12.001
Sanati H, Kiani R, Shakerian F et al (2016) Coronary slow flow phenomenon clinical findings and predictors. Res Cardiovasc Med 5:1–5. https://doi.org/10.5812/cardiovascmed.30296
Huang Q, Zhang F, Chen S et al (2021) Clinical characteristics in patients with coronary slow flow phenomenon: a retrospective study. Medicine 100:1–8. https://doi.org/10.1097/MD.0000000000024643
Wang X, Nie S-P (2011) The coronary slow flow phenomenon: characteristics, mechanisms and implications. Cardiovasc Diagn Ther 1:37–43. https://doi.org/10.3978/j.issn.2223-3652.2011.10.01
Afsin A, Kaya H, Suner A et al (2021) Plasma atherogenic indices are independent predictors of slow coronary flow. BMC Cardiovasc Disord 21:1–9. https://doi.org/10.1186/s12872-021-02432-5
Aparicio A, Cuevas J, Morís C, Martín M (2022) Slow coronary blood flow: pathogenesis and clinical implications. Eur Cardiol 17:e08. https://doi.org/10.15420/ecr.2021.46
Gibson CM, Cannon CP, Daley WL et al (1996) TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 93:879–888. https://doi.org/10.1161/01.CIR.93.5.879
Yang Z, Yuan J, Cui J et al (2021) Association of the lymphocyte-to-monocyte ratio, mean diameter of coronary arteries, and uric acid level with coronary slow flow in isolated coronary artery ectasia. BMC Cardiovasc Disord 21:156. https://doi.org/10.1186/s12872-021-01952-4
Altun I, Akin F, Kose N et al (2015) Predictors of slow flow in angiographically normal coronary arteries. IJCEM 8:13762–13768
Elsanan MAHA, Tahoon IHHH, Mohamed GI et al (2023) Relationship between inflammatory markers and coronary slow flow in type 2 diabetic patients. BMC Cardiovasc Disord 23:1–8. https://doi.org/10.1186/s12872-023-03275-y
Shui Z, Wang Y, Sun M et al (2021) The effect of coronary slow flow on left atrial structure and function. Sci Rep 11:7511. https://doi.org/10.1038/s41598-021-87193-z
Limberg JK, Morgan BJ, Schrage WG (2016) Peripheral blood flow regulation in human obesity and metabolic syndrome. Exerc Sport Sci Rev 44:116–122. https://doi.org/10.1249/JES.0000000000000083
Wen J, He L, Du X, Ma C-S (2022) Body mass index enhances the associations between plasma glucose and mortality in patients with acute coronary syndrome. DMSO 15:2675–2682. https://doi.org/10.2147/DMSO.S370118
Powell-Wiley TM, Poirier P, Burke LE et al (2021) Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000000973
Department of Cardiology, Bolu Abant Izzet Baysal University School of Medicine, Bolu, Turkey, Izgi IA (2022) Coronary slow flow. Turk Kardiyol Dern Ars 50:239–241. https://doi.org/10.5543/tkda.2022.22485
Zebic Mihic P, Saric S, Bilic Curcic I et al (2023) The association of severe coronary tortuosity and non-obstructive coronary artery disease. Medicina 59:1619. https://doi.org/10.3390/medicina59091619
Kersten JR, Toller WG, Tessmer JP et al (2001) Hyperglycemia reduces coronary collateral blood flow through a nitric oxide-mediated mechanism. Am J Physiol-Heart Circ Physiol 281:H2097–H2104. https://doi.org/10.1152/ajpheart.2001.281.5.H2097
Angeli F, Reboldi G, Poltronieri C et al (2015) Hyperglycemia in acute coronary syndromes: from mechanisms to prognostic implications. Ther Adv Cardiovasc Dis 9:412–424. https://doi.org/10.1177/1753944715594528
Nader E, Skinner S, Romana M et al (2019) Blood rheology: key parameters, impact on blood flow, role in sickle cell disease and effects of exercise. Front Physiol 10:1329. https://doi.org/10.3389/fphys.2019.01329
Budzianowski J, Pieszko K, Burchardt P et al (2017) The role of hematological indices in patients with acute coronary syndrome. Dis Markers 2017:1–9. https://doi.org/10.1155/2017/3041565
Seyyed Mohammadzad MH, Khademvatani K, Gardeshkhah S, Sedokani A (2021) Echocardiographic and laboratory findings in coronary slow flow phenomenon: cross-sectional study and review. BMC Cardiovasc Disord 21:1–8. https://doi.org/10.1186/s12872-021-02044-z
Ma W, Cui C, Feng S et al (2021) Platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in patients with newly diagnosed moyamoya disease: a cross-sectional Study. Front Neurol 12:631454. https://doi.org/10.3389/fneur.2021.631454
Forget P, Khalifa C, Defour J-P et al (2017) What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes 10:12. https://doi.org/10.1186/s13104-016-2335-5
Moosazadeh M, Maleki I, Alizadeh-Navaei R et al (2019) Normal values of neutrophils/lymphocytes ratio, lymphocytes/monocytes ratio and platelets/lymphocytes ratio among Iranian population: results of Tabari cohort. Caspian J Intern Med. https://doi.org/10.22088/cjim.10.3.320
Dutta U, Sinha A, Demir OM et al (2023) Coronary slow flow is not diagnostic of microvascular dysfunction in patients with angina and unobstructed coronary arteries. JAHA 12:e027664. https://doi.org/10.1161/JAHA.122.027664
Sharma YP, Batta A, Makkar K et al (2022) Angiographic profile and outcomes in persistent non-valvular atrial fibrillation: a study from tertiary care center in North India. Indian Heart J 74:7–12. https://doi.org/10.1016/j.ihj.2021.12.010
Gao Y, Chen Y, Wang C et al (2023) Atrial fibrillation episode status and incidence of coronary slow flow: a propensity score-matched analysis. Front Cardiovasc Med 10:1047748. https://doi.org/10.3389/fcvm.2023.1047748
Chen Z, Chen X, Li S et al (2015) Nicorandil improves myocardial function by regulating plasma nitric oxide and endothelin-1 in coronary slow flow. Coron Artery Dis 26:114–120. https://doi.org/10.1097/MCA.0000000000000179
Sani HD, Eshraghi A, Nezafati MH et al (2015) Nicorandil versus nitroglycerin for symptomatic relief of angina in patients with slow coronary flow phenomenon: a randomized clinical trial. J Cardiovasc Pharmacol Ther 20:401–406. https://doi.org/10.1177/1074248415571457
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors collected research data in case report form and compiled a literature review with equal portions. RE performed all statistical calculations, analyzed and interpreted data, and was a major contributor to writing the manuscript. RE and YP are responsible for proofreading the manuscript. YI conducted ethical clearance in hospitals and universities. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research has received approval from the ethics board of West Nusa Tenggara General Hospital, Indonesia, with reference number 00.9/18/0540/RSUDP/2024. The hospital's research director, Suciati, MD, signed the ethics letter.
Consent for publication
Not applicable.
Competing interests
We, as the authors, have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ermawan, R., Pintaningrum, Y. & Indrayana, Y. The predictors of coronary slow flow in patients undergoing coronary angiography. Egypt Heart J 76, 103 (2024). https://doi.org/10.1186/s43044-024-00536-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00536-9