Abstract
Background
Functional health status is increasingly being recognized as a viable endpoint in heart failure (HF) trials. We sought to assess its prognostic impact and relationship with traditional clinical outcomes in patients with HF.
Methods
MEDLINE and Cochrane central were searched up to January 2021 for post hoc analyses of trials or observational studies that assessed independent association between baseline health/functional status, and mortality and hospitalization in patients with HF across the range of left ventricular ejection fractions to evaluate the prognostic ability of NYHA class [II, III, IV], KCCQ, MLHFQ, and 6MWD. Hazard ratios (HR) with 95% confidence intervals were pooled.
Results
Twenty-two studies were included. Relative to NYHA I, NYHA class II (HR 1.54 [1.16–2.04]; p < 0.01), NYHA class III (HR 2.08 [1.57–2.77]; p < 0.01), and NYHA class IV (HR 2.53 [1.25–5.12]; p = 0.01) were independently associated with increased risk of mortality. 6MWD (per 10 m) was associated with decreased mortality (HR 0.98 [0.98–0.99]; p < 0.01). A 5-point increase in KCCQ-OSS (HR 0.94 [0.91–0.96]; p < 0.01) was associated with decreased mortality. A high MLHFQ score (> 45) was significantly associated with increased mortality (HR 1.30 [1.14–1.47]; p < 0.01). NHYA class, 6MWD (per 10 m), KCCQ-OSS, and MLHFQ all significantly associated with all-cause mortality in patients with HF.
Conclusion
Identifying such patients with poor health status using functional health assessment can offer a complementary assessment of disease burden and trajectory which carries a strong prognostic value.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Assessing functional health capacity is an important and recommended component of heart failure (HF) care [1]. Indeed, when acknowledging the potential debilitating effects of HF on physical, social, and psychological health status, many patients may value improved quality of life more than prolonging survival [2, 3]. Cardiovascular societies such as the American Heart Association (AHA) [4] and the European Society of Cardiology (ESC) [5] as well as patient advocate groups and regulatory bodies, such as the Food and Drug Administration (FDA) [6], actively advocate for the inclusion of patient-reported outcomes (PRO) as an endpoint complementary to mortality, cardiovascular events, and hospitalization in HF patients. Functional health assessment, which is often evaluated by the use of health-related quality of life (HRQoL) tools, enables an accurate surveillance of disease burden [4] due to their ability to assess common HF symptoms which are otherwise infrequently reported, such as fatigue and anxiety, thereby assisting clinicians in making informed clinical decisions. However, due to the complex nature of HF care and limited time and resources, the assessment of functional health status in HF patients is often sidelined in routine practice and infrequently included within primary outcomes of HF randomized trials [7]. Clarifying the relationship between traditional clinical outcomes such as mortality and hospitalization and their association with various functional status endpoints may further highlight the importance of these quality-of-life scores. Moreover, the degree to which functional status outcomes yield similar prognostic value in HFrEF and HFpEF is unclear, with prior studies demonstrating inconsistent results [8, 9]. Likewise, based on recent analyses, functional health assessment can vary considerably across racial/ethnic groups [10, 11] and geographic regions [12]. In this context, we aimed to conduct a systematic review and meta-analysis to comprehensively evaluate the prognostic ability of New York Heart Association (NYHA), 6-minute walk distance (6MWD), Kansas City Cardiomyopathy Questionnaire (KCCQ), and Minnesota Living with Heart Failure Questionnaire (MLHFQ) with the clinical endpoints of mortality and hospitalization in patients with HF. In addition, we examined regional differences with respect to tools for health or functional status.
Methods
This meta-analysis follows the Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) and AHA guidelines for systematic reviews and meta-analyses [13, 14]. The MEDLINE and Cochrane central databases were searched up to January 2021. No time or language restrictions were set. Table S1 outlines the search strategy. All articles retrieved were transferred to Endnote Reference Library (Version X8.1; Clarivate Analytics, Philadelphia, Pennsylvania) software, where duplicates were identified and removed. Titles and abstracts of all articles were independently screened by two reviewers (AAS and AA). Full texts of all shortlisted articles were then read to confirm relevance. To ensure no relevant articles were missed, bibliographies of all relevant studies and review articles were also screened. Any discrepancies between the two reviewers were resolved by consulting a third reviewer (IS).
Studies were included if they fulfilled the following eligibility criteria: (a) included patients with any HF; (b) reported all-cause mortality and/or hospitalization in HF patients; (c) reported disease-specific functional assessment tools rather than generic tools when predicting mortality and/or hospitalization; and (d) reported the following cutoff values: (≥ 5 for KCCQ, > 45 for MLHFQ and ≤ 200 m or 10 m increments for 6MWD) and classes [II, III, and IV] for NYHA. (e) Studies that were post hoc analyses of trials or observational studies that assessed independent association between baseline health/functional status and mortality and/or hospitalization.
Two reviewers (AAS and AA) independently extracted data pertaining study characteristics and baseline characteristics such as the number of participants, publication year, HF classification (classified according to reduced or preserved ejection fraction), left ventricular ejection fraction (LVEF), geographic location, length of follow-ups, and mean/median ages. Geographical regions were dependent on the location of where each study was coordinated. This was divided into 4 distinct locations, namely North America (including Canada and US), Europe (including any country in Europe), multi-regional (including countries from North American and Europe), and rest of the world.
The risk of bias was assessed using the Newcastle–Ottawa quality assessment scale for observational studies (Table S2) [15] and the Cochrane risk of bias assessment tool for RCTs (Figure S1) [16]. The Newcastle–Ottawa scale consists of three domains: (a) selection; (b) comparability; and (c) outcome. The quality was appraised using numbers such that the maximum score was 9, and a study with 7–9 had low risk, 4–6 had high risk, and 0–3 had very high risk of bias. The Cochrane tool had seven domains, namely random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other biases [16]. In addition, we used the Gill and Feinstein criteria [17] to review how well quality of life was being measured in the publications by assessing how well they dealt with conceptual issues and methodology, with each criteria having several components as presented in Table S3. Any discrepancies between the 2 reviewers were resolved by consulting a third reviewer (IS). Publication bias assessment could not be conducted as the number of studies within each data set were less than 10.
Outcomes of interest included mortality and hospitalization using the following predictor variables: NYHA functional classes (I, II, III, IV) 6MWD test (≤ 200 m or 10 m increments), KCCQ (≥ 5 point increase in overall summary score [OSS]), and MLHFQ (> 45 score). Behlouli et al. [18] define a MLHFQ score > 45 representing poor QOL with a validation accuracy of 91%. Scores above this threshold indicate a significant burden of heart failure symptoms for KCCQ, an improvement or worsening of ≥ 5 points and indicate a minimal clinically important difference in health status [19, 20]. A 6MWD < 200 m could identify patients with stable HF who are at markedly increased risk of death [21]. This cutoff point, chosen using Akaike’s information criterion, also resulted in the highest Harrell’s concordance index (c‐index) [22]. The threshold of 10 m increments in 6MWD was included based on its availability in the pooled studies.
RevMan (version 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for all statistical analyses. The results were presented as hazard ratios (HR) with 95% confidence intervals (CI), which were pooled using a generic invariance weighted random effects model. Forest plots were created to visually assess the pooled analysis. A geographic regional subgroup analysis was also conducted for each functional health assessment tool where possible. Leave-one-out sensitivity analysis was conducted to see if any one study disproportionately affected the results. Heterogeneity across studies was evaluated using Higgins I2, where a value less than 50% was considered acceptable and a value > 75% was considered significant. A p value < 0.05 was considered significant in all cases.
Results
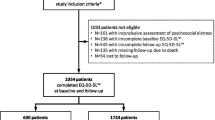
The initial literature search revealed 3050 articles. After exclusions, 22 studies [10 RCTs [21,22,23,24,25,26,27,28,29,30]; 12 observational [31,32,33,34,35,36,37,38,39,40,41,42]] involving 29,064 HF patients were included. Four of these studies assessed more than 1 functional health assessment tool [21, 26, 27, 38]. Majority of health assessment tools analyzed in our study focused on patients with HFrEF [n = 14], while few explored outcomes in patients with HFpEF [n = 4] and some assessed both [n = 4] (Table 1). The PRISMA flowchart (Fig. 1) summarizes that results of our literature search (Table 1) outline the baseline characteristics of all included studies. Quality assessment using the Cochrane risk of bias assessment tool for RCTs demonstrated that majority of the studies included in this meta-analysis were at a low risk of bias (Figure S1). Newcastle–Ottawa scores for observational studies indicated good methodological quality (Table S2).
PRISMA flowchart outlining literature search. [CHF, Coronary Heart Failure; EF, Ejection Fraction; IQR, Interquartile Range; HF, Heart Failure; HFpEF, Heart failure with Preserved Ejection Fraction; HFrEF, Heart failure with Reduced Ejection Fraction; HRQOL, Health-Related Quality Of Life; KCCQ, Kansas City Cardiomyopathy Questionnaire; LVEF, Left Ventricular Ejection Fraction; MLHFQ, Minnesota Living with Heart Failure Questionnaire; NYHA, New York Heart Association; 6MWD, 6-Minute Walk Distance; and SD, Standard Deviation]
The evaluation of methodological and conceptual quality or rigor according to the criteria of Gill and Feinstein et al. [43, 44] (Table S3) revealed that only 1 study (4%) of the 23 provided a definition of the concept QOL (criterion 1). In 15 of the papers (65%), the investigators stated the domains they measured as part of QOL (criterion 2). In 16 of the papers (70%), the investigators gave a specific reason for the choice of instrument to measure QOL (criterion 3). In 10 (44%) of the studies, the investigators had aggregated results from multiple items, domains, or instruments into a single composite score for QOL (criterion 4). In 8 studies (35%) fulfilled criterion 5, concerning whether patients were asked to give their own global rating of QOL by a single item at the end of the questionnaire. However, evaluation of the studies showed that criteria 7–10 were not fulfilled.
We investigated the association between NYHA functional class and all-cause mortality and hospitalization. Of the 9 studies (n = 12,647 HF patients), 2 were exploratory analyses of RCTs [26, 27] and 7 were prospective cohorts [31,32,33, 35, 38, 40, 41] with a median follow-up ranging between 1 and 24 months. Four of these studies recruited patients with HFrEF [27, 33, 35, 38] only, 1 study recruited HFpEF patients [31], and 4 studies recruited patients of all subtypes [26, 32, 40, 41]. The studies typically adjusted for demographics, comorbidities and etiology of HF. Relative to NYHA I, NYHA functional classes II-IV were significant predictors of mortality.
NYHA class II (HR 1.54 [1.16–2.04]; I2 = 0%; p < 0.01), NYHA class III (HR 2.08 [1.57–2.77]; I2 = 2%; p < 0.01), and NYHA class IV (HR 2.53 [1.25–5.12]; I2 = 73%; p = 0.01) were independently associated with increased risk of mortality compared with baseline NYHA functional class I (Fig. 2). Leave-one-out sensitivity analysis showed Ahmed et al. [31] to have a disproportionate effect on the heterogeneity of the results of NYHA IV. Removal of this study from NYHA class IV led to a reduction in heterogeneity while the results remained significant (HR 1.74 [1.16–2.60]; I2 = 0%; p < 0.01).
Subgroup analysis based on geographic regions showed NYHA classes II, III, and IV to be associated with increased mortality in both Europe and North America (Figures s2–s4). NYHA class IV had a stronger association with mortality in European regions (HR 2.70 [1.64–4.45]; I2 = 90%; p < 0.01) than North America (HR 1.93 [1.14–3.28]; I2 = 0%; p = 0.01) (Figure s4).
Studies which did not mention any baseline NYHA functional class were also pooled together to depict a per point increase, which similarly revealed an increased association with mortality (HR 1.70 (1.49–1.95]; I2 = 37%; p < 0.01) (Figure S5).
We also investigated the association between 6MWD-test and all-cause mortality and hospitalization. Of the 7 studies (n = 12,027 HF patients), 4 were exploratory analysis of RCTs [21, 22, 26, 27] and 3 were prospective cohort studies [38,39,40] with a median follow-up duration between 1.5 and 5 years. Out of these, 4 of these studies recruited patients with HFrEF [22, 27, 38, 39], while the remaining three recruited patients of all subtypes. The studies typically adjusted for demographics, comorbidities, and NYHA. Three of these studies investigated mortality and hospitalization with ≤ 200 m distances covered by the participants. Of these, 2 studies were conducted in North America [21, 26], while one was multicenter [22]. The other 4 studies reported distance measured for 10 m increments for mortality in European regions [27, 38,39,40].
Overall, in the 10 m increment studies, a significant association was observed between a lower 6MWD and mortality (HR 0.98 [0.98–0.99]; I2 = 28%; p < 0.01) in European regions (Fig. 3). However, of studies that dichotomized 6MWD, a distance ≤ 200 m was not significantly associated with mortality (HR 1.42 [0.86–2.32]; I2 = 76%; p = 0.17) (Figure S6) or hospitalization (HR 1.38 [0.91–2.07]; I2 = 84%; p = 0.13) (Figure S7). Upon sensitivity analysis, removal of the only study [22] that measured 6MWD using linear splines led to a reduction in heterogeneity and a significant association between ≤ 200 m 6MWD and mortality (HR 1.85 [1.22–2.80]; I2 = 0%; p < 0.01) and hospitalization (HR 1.69 [1.28–2.22]; I2 = 0%; p < 0.01) (Figures s8–s9) [22].
We also studied the association between KCCQ-OSS and all-cause mortality. Among 3 RCTs (n = 6,194 HF patients), 2 recruited patients with HFpEF and HFrEF [28, 42], while 1 recruited only HFrEF patients [23], with a median follow-up duration between 0.25 and 3.3 years. The RCTs typically adjusted for demographics and comorbidities. Overall, a 5-point or higher increase (≥ 5 point) in KCCQ-OSS was associated with decreased mortality (HR 0.94 [0.91–0.96]; I2 = 0%; p < 0.01). Upon subgroup analysis by HF subtypes, increments in KCCQ-OSS revealed a significant association with decreased mortality in both HFpEF (HR 0.95 [0.92 -0.98]; I2 = 0%; p < 0.01) and HFrEF (HR 0.91 [0.87–0.95]; I2 = 0%; p < 0.01) subgroups (Fig. 4). However, no subgroup differences in the predictive ability of KCCQ-OSS were observed when the HF subtypes were compared with each other (p = 0.12). Additionally, no geographical analyses could be conducted due to a lack of data.
Increase of ≥ 5 point in KCCQ-OSS with all-cause mortality in HFpEF and HFrEF patients. [CI, Confidence Interval; HR, Hazard Ratio; HFpEF, Heart Failure with Preserved Ejection Fraction; HFrEF; Heart Failure with Reduced Ejection Fraction; KCCQ-OSS, Kansas City Cardiomyopathy Questionnaire; Overall Summary Score; and SE, Standard Error]
Additionally, we analyzed the association between MLHFQ and all-cause mortality. Of the 7 studies (n = 6,980 HF patients), 4 were exploratory RCTs [24, 25, 29, 30] and 3 were prospective cohort studies [34, 36, 37] with a median follow-up duration between 1 and 5.5 years. Out of these, 4 of these studies recruited patients with HFrEF [24, 25, 29, 36], while the remaining 3 recruited patients of all subtypes [30, 34, 37]. The studies typically adjusted for demographics and disease-related variables such as systolic blood pressure (SBP) and NYHA. Our results revealed that a high MLHFQ score (> 45) was significantly associated with increased mortality (HR 1.30 [1.14–1.47]; I2 = 0%; p < 0.01) (Fig. 5). Furthermore, a subgroup analysis of geographical variation revealed a significantly higher association of MLHFQ with mortality in North America (HR 1.40 [1.03–1.91]; I2 = 0%; p < 0.01) compared with Europe (HR 1.25 [1.07–1.46]; I2 = 0%; p < 0.01) (Figure S10).
Discussion
This meta-analysis involving 29,064 HF patients suggests that clinician-reported outcomes like NYHA and 6MWD for 10 m intervals and PROs such as KCCQ-OSS (≥ 5 points) and > 45 cutoff for MLHFQ are all significant predictors of mortality and/or hospitalization. Majority of health assessment tools analyzed in our study focused on patients with HFrEF [n = 14], while few explored outcomes in patients with HFpEF [n = 4] and some assessed both [n = 4] (Table 1). The models of the underlying studies adjusted for baseline patient characteristics and medical comorbidities.
HF often constitutes an unpredictable disease trajectory, with majority patients having a markedly impaired quality of life. The complex nature of this disease coupled with diverse pathophysiology and subsequent clinical outcomes entails the inclusion of more patient-centered outcomes which incorporates the patient’s perspective and lived experience, thereby including measures and variables which can better assess the trajectory of disease course [45]. Although assessment of mortality and hospitalization endpoints in clinical trials remains critical, the current data suggest that functional status and patient-reported outcomes offer a complementary assessment of disease burden and trajectory that carries strong prognostic value. Inclusion of these tools confers several advantages. Routine serial assessment of patient-reported outcomes and functional assessments may serve as reliable indicators of disease trajectory [46,47,48]. Further, compared to other invasive assessment tools such as biomarkers and implantable devices, the noninvasive nature and potential for remote assessment of health status makes it easier for both patients and clinicians to implement and routinely follow-up.
Our results revealed significant positive association of NYHA classes II, III, and IV with risk of mortality relative to NYHA class I. Only in NYHA IV did Ahmed et al. [31] contribute to significantly increased heterogeneity of the results. This could be because the study primarily focused on patients with HFpEF, while other studies mostly included patients with HFrEF. HFpEF patients tend to have various underlying etiologies as opposed to HFrEF, which is commonly associated with increased neurohormonal activation [49]. A stronger perceived association between mortality and a higher NYHA class in the study may be attributed to lack of therapeutic intervention for HFpEF patients, thereby necessitating further research into this particular populace. Additionally, our results demonstrated that classes III and IV had an increased association with mortality compared with classes I and II. These results are consistent with previous similar studies [31, 50, 51]. Patients with higher NYHA classes are usually older and have more underlying comorbidities such as kidney disease and an increased duration of cardiovascular disease which can lead to a decrease in QOL [52].
The 6MWD test, compared with the more commonly used cardiopulmonary exercise test (CPET), is a relatively affordable and easy way to assess a person’s functional health capacity [53]. Our analysis revealed that when measured on a continuous scale at 10 m intervals, the 6MWD test is especially useful in predicting mortality in patients with HFrEF. The studies pooled for 6MWD in the ≤ 200 m subgroup mainly included participants from North America with decreased LVEF, thus making this iteration more usable for HFrEF patients from the USA and Canada when predicting hospitalization. However, due to the limited number of existing studies on hospitalization from other countries, further research is needed to confirm our findings.
Similar to prior functional health assessment tools, our results demonstrated a significant association between a ≥ 5-point increase in the KCCQ-OSS score, and a decrease in mortality for both HFpEF and HFrEF. One study suggested the inclusion of biomarkers along with KCCQ-OSS to improve its ability in predicting clinical outcomes in patients with HFpEF [42]. Moreover, Huang et al. [54] demonstrated that using only the physical independence and social interaction components of the KCCQ score may also provide significantly better prognosis in HFpEF patients. Therefore, future studies should explore the accuracy of KCCQ score utility in patients with HFpEF.
Furthermore, our results assessing prognostic ability of MLHFQ scores with mortality using the standardized cutoff of > 45 concur with results of a prior meta-analysis, wherein higher MLHFQ scores indicate poor functional status, thereby increasing the risk of death. Majority studies analyzing MLHFQ score included patients with HFrEF, thus making it more suitable to determine prognosis in this cohort.
Conclusion
In our study, majority of the functional health assessment tools were tested in North American cohorts, followed by European regions, while none of the studies reported results in rest of the world. This variation can possibly be due to the fact that most HF RCTs are conducted in North America and Europe [55]. Moreover, PRO data from HF RCTs are not commonly collected overall, but after adjusting for trial factors, are more commonly collected in trials led in Central/South America [56]. Therefore, by using readily available prognostic tools like NYHA, KCCQ, MLHFQ, and 6MWD, healthcare professionals in lower income countries may have decreased dependence on laboratory testing, such as natriuretic peptides or echocardiograms, which may not be widely available or affordable in many underdeveloped regions [12].
This meta-analysis has a few limitations that should be considered while interpreting the results. First, this meta-analysis included observational studies and secondary analyses of RCTs which are prone to residual bias. Second, differences in HF etiologies, study designs, interventions, patient, and trial characteristics present in the patient population may have contributed to clinical heterogeneity. Third, the follow-up ranges for most studies were variable, with some studies reporting longer follow-up periods. Short-term follow-ups are more useful when evaluating disease prognosis. However, long-term prognosis can overestimate progress by showing better recovery or can show worse decline in health. Additionally, when assessing ability of the tools to predict mortality, no specific time frame was mentioned in the studies. We did, however, include the range of median follow-up periods for each tool in their respective section. Lastly, the studies focusing on HF with preserved EF were few. Consequently, we were only able to make limited comparisons of clinical outcomes between HFrEF and HFpEF; hence, our results are exploratory for the HFpEF subtype.
Our findings suggest that NHYA, 6MWD (per 10 m), and MLHFQ provide significant prognostic value in predicting all-cause mortality for HF patients, particularly those with reduced EF. Further research is needed to assess prognostic impact of functional status in patients with HF in regions outside North America and Europe.
Availability of data and materials
All data generated and/or analyzed during this study are included in this published article.
Abbreviations
- AHA:
-
American Heart Association
- CI:
-
Confidence interval
- CPET:
-
Cardiopulmonary exercise test
- EF:
-
Ejection fraction
- ESC:
-
European Society of Cardiology
- FDA:
-
Food and Drug Administration
- HF:
-
Heart failure
- HFpEF:
-
Heart Failure with preserved Ejection Fraction
- HFrEF:
-
Heart Failure with reduced Ejection Fraction
- HR:
-
Hazard ratio
- KCCQ:
-
Kansas City Cardiomyopathy Questionnaire
- KCCQ-OSS:
-
Kansas City Cardiomyopathy Questionnaire Overall Summary Score
- LVEF:
-
Left ventricular ejection fraction
- MLHFQ:
-
Minnesota Living with Heart Failure Questionnaire
- NYHA:
-
New York Heart Association
- PRISMA:
-
Preferred Reporting Items for Systematic review and Meta-Analyses
- PRO:
-
Patient-reported outcome
- QOL:
-
Quality of life
- RCT:
-
Randomized control trial
- SBP:
-
Systolic blood pressure
- SE:
-
Standard error
- 6MWD:
-
6-Minute walk distance
References
Greene SJ, Adusumalli S, Albert NM et al (2021) Building a heart failure clinic: a practical guide from the heart failure society of America. J Card Fail 27:2–19
Rector TS, Tschumperlin LK, Kubo SH et al (1995) Use of the living with heart failure questionnaire to ascertain patients’ perspectives on improvement in quality of life versus risk of drug-induced death. J Card Fail 1:201–206
Lewis EF, Johnson PA, Johnson W et al (2001) Preferences for quality of life or survival expressed by patients with heart failure. J Hear Lung Transplant 20:1016–1024
Rumsfeld JS, Alexander KP, Goff DC et al (2013) Cardiovascular health: The importance of measuring patient-reported health status a scientific statement from the American heart association. Circulation. https://doi.org/10.1161/CIR.0b013e3182949a2e
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200m
Caldwell, B. Value and use of patient-reported outcomes (PROs) in assessing effects of medical devices.
Cavanagh CE (2019) Quality of life in heart failure: screening alone is insufficient. Eur Heart J Qual Care Clin Outcomes 5:191–192
Garin O, Herdman M, Vilagut G et al (2014) Assessing health-related quality of life in patients with heart failure: a systematic, standardized comparison of available measures. Heart Fail Rev 19:359–367
Berry C, McMurray J (1999) A review of quality-of-life evaluations in patients with congestive heart failure. Pharmacoeconomics 16:247–271
Lim E, Davis J, Siriwardhana C et al (2020) Racial/ethnic differences in health-related quality of life among Hawaii adult population. Health Qual Life Outcomes 18:1–16
Hayes DK, Greenlund KJ, Denny CH et al (2007) Racial/ethnic and socioeconomic disparities in health-related quality of life among people with coronary heart disease. Prev Chronic Dis 8:A78
Johansson I, Joseph P, Balasubramanian K et al (2021) Health-related quality of life and mortality in heart failure: the global congestive heart failure study of 23,000 patients from 40 countries. Circulation 143:2129–2142
Hutton B, Salanti G, Caldwell DM et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern Med 162:777–784
Rao G, Lopez-Jimenez F, Boyd J et al (2017) Methodological standards for meta-analyses and qualitative systematic reviews of cardiac prevention and treatment studies a scientific statement from the American Heart Association. Circulation 136:e172–e194
Ottawa Hospital Research Institute.
Higgins JPTT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.d5928
Moons P, Budts W, De Geest S (2006) Critique on the conceptualisation of quality of life: a review and evaluation of different conceptual approaches. Int J Nurs Stud 43:891–901
Behlouli H, Feldman DE, Ducharme A, et al. Identifying relative cut-off scores with neural networks for interpretation of the minnesota living with heart failure questionnaire. In: Proceedings of the 31st annual international conference of the IEEE engineering in medicine and biology society: engineering the future of biomedicine, EMBC 2009. https://doi.org/10.1109/IEMBS.2009.5334659.
Kaplinsky E (2020) DAPA-HF trial: dapagliflozin evolves from a glucose-lowering agent to a therapy for heart failure. Drugs Context. https://doi.org/10.7573/DIC.2019-11-3
Spertus J, Peterson E, Conard MW et al (2005) Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J. https://doi.org/10.1016/j.ahj.2004.12.010
Curtis JP, Rathore SS, Wang Y et al (2004) The association of 6-minute walk performance and outcomes in stable outpatients with heart failure. J Card Fail 10:9–14
Matsumoto K, Xiao Y, Homma S et al (2020) Prognostic impact of 6 min walk test distance in patients with systolic heart failure: insights from the WARCEF trial. ESC Hear Fail. https://doi.org/10.1002/ehf2.13068
Luo N, O’Connor CM, Cooper LB et al (2019) Relationship between changing patient-reported outcomes and subsequent clinical events in patients with chronic heart failure: insights from HF-ACTION. Eur J Heart Fail 21:63–70
Friedmann E, Thomas SA, Liu F et al (2006) Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 152:940.e1-940.e8
Tate CW, Robertson AD, Zolty R et al (2007) Quality of life and prognosis in heart failure: results of the beta-blocker evaluation of survival trial (BEST). J Card Fail 13:732–737
Alahdab MT, Mansour IN, Napan S et al (2009) Six minute walk test predicts long-term all-cause mortality and heart failure rehospitalization in African-American patients hospitalized with acute decompensated heart failure. J Card Fail 15:130–135
Manzano L, Babalis D, Roughton M et al (2011) Predictors of clinical outcomes in elderly patients with heart failure. Eur J Heart Fail 13:528–536
Pokharel Y, Khariton Y, Tang Y et al (2017) Association of serial Kansas city cardiomyopathy questionnaire assessments with death and hospitalization in patients with heart failure with preserved and reduced ejection fraction: a secondary analysis of 2 randomized clinical trials. JAMA Cardiol 2:1315–1321
Bundgaard JS, Thune JJ, Gislason G et al (2020) Quality of life and the associated risk of all-cause mortality in nonischemic heart failure. Int J Cardiol 305:92–98
Hoekstra T, Jaarsma T, Van Veldhuisen DJ et al (2013) Quality of life and survival in patients with heart failure. Eur J Heart Fail 15:94–102
Ahmed A, Aronow WS, Fleg JL (2006) Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J 151:444–450
Ingle L, Rigby AS, Carroll S et al (2007) Prognostic value of the 6 min walk test and self-perceived symptom severity in older patients with chronic heart failure. Eur Heart J 28:560–568
Frankenstein L, Remppis A, Graham J et al (2008) Gender and age related predictive value of walk test in heart failure: do anthropometrics matter in clinical practice? Int J Cardiol 127:331–336
Hole T, Grundtvig M, Gullestad L et al (2010) Improved quality of life in Norwegian heart failure patients after follow-up in outpatient heart failure clinics: results from the Norwegian heart failure registry. Eur J Heart Fail 12:1247–1252
Boxer R, Kleppinger A, Ahmad A et al (2010) The 6-minute walk is associated with frailty and predicts mortality in older adults with heart failure. Congest Hear Fail 16:208–213
Pressler SJ, Kim J, Riley P et al (2010) Memory dysfunction, psychomotor slowing, and decreased executive function predict mortality in patients with heart failure and low ejection fraction. J Card Fail 16:750–760
Zuluaga MC, Guallar-Castillón P, López-García E et al (2010) Generic and disease-specific quality of life as a predictor of long-term mortality in heart failure. Eur J Heart Fail 12:1372–1378
Ingle L, Cleland JG, Clark AL (2014) The long-term prognostic significance of 6-minute walk test distance in patients with chronic heart failure. Biomed Res Int. https://doi.org/10.1155/2014/505969
Ingle L, Cleland JG, Clark AL (2014) The relation between repeated 6-minute walk test performance and outcome in patients with chronic heart failure. Ann Phys Rehabil Med 57:244–253
Grundtvig M, Eriksen-Volnes T, Ørn S et al (2020) 6 min walk test is a strong independent predictor of death in outpatients with heart failure. ESC Hear Fail 7:2904–2911
Cicoira M, Davos CH, Florea V et al (2001) Chronic heart failure in the very elderly: Clinical status, survival, and prognostic factors in 188 patients more than 70 years old. Am Heart J 142:174–180
Sepehrvand N, Savu A, Spertus JA et al (2020) Change of health-related quality of life over time and its association with patient outcomes in patients with heart failure. J Am Heart Assoc 9:e017278
Moons P, Van Deyk K, Budts W et al (2004) Caliber of quality-of-life assessments in congenital heart disease: a plea for more conceptual and methodological rigor. Arch Pediatr Adolesc Med 158:1062–1069
Gill TM, Feinstein AR (1994) A Critical Appraisal of the Quality of Quality-of-Life Measurements. JAMA 272:619–626
Determining Quality of Life - The Cardiology Advisor.
Ferraro KF, Kelley-Moore JA (2001) Self-rated health and mortality among black and white adults: examining the dynamic evaluation thesis. J Gerontol Ser B Psychol Sci Soc Sci. https://doi.org/10.1093/geronb/56.4.S195
Lyyra TM, Leskinen E, Jylhä M et al (2009) Self-rated health and mortality in older men and women: a time-dependent covariate analysis. Arch Gerontol Geriatr 48:14–18
Sadetsky N, Hubbard A, Carroll PR et al (2009) Predictive value of serial measurements of quality of life on all-cause mortality in prostate cancer patients: Data from CaPSURE™ (cancer of the prostate strategic urologic research endeavor) database. Qual Life Res 18:1019–1027
Butler J, Hamo CE, Udelson JE et al (2016) Exploring new endpoints for patients with heart failure with preserved ejection fraction. Circ Hear Fail. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003358
Briongos-Figuero S, Estévez A, Pérez ML et al (2020) Prognostic role of NYHA class in heart failure patients undergoing primary prevention ICD therapy. ESC Hear Fail 7:279–283
New York Heart Association Class - an overview | ScienceDirect Topics.
Ahmed A (2007) A propensity matched study of New York Heart association class and natural history end points in heart failure. Am J Cardiol 99:549–553
Giannitsi S, Bougiakli M, Bechlioulis A et al (2019) 6-minute walking test: a useful tool in the management of heart failure patients. Therapeut Adv Cardiovasc Dis. https://doi.org/10.1177/1753944719870084
Huang W, Teng TK, Tay WT et al (2020) Patient-reported outcomes in heart failure with preserved vs reduced ejection fraction: focus on physical independence. ESC Heart Fail 7:2051–2062
Zhu JW, Le N, Wei S et al (2021) Global representation of heart failure clinical trial leaders, collaborators, and enrolled participants: a bibliometric review 2000–20. Eur Heart J Qual Care Clin Outcomes. https://doi.org/10.1093/EHJQCCO/QCAB058
Eliya Y, Whitelaw S, Thabane L et al (2021) Temporal trends and clinical trial characteristics associated with the inclusion of women in heart failure trial steering committees: a systematic review. Circ Heart Fail. https://doi.org/10.1161/CIRCHEARTFAILURE.120.008064
Acknowledgements
Not applicable.
Funding
The authors declare that they have no source of funding.
Author information
Authors and Affiliations
Contributions
AA and AAS contributed to conceptualization, methodology, investigation, writing—original draft, and data curation. IS and HGCVS were involved in supervision, resources, and writing—reviewing and editing. SJG and MF contributed to writing—reviewing and editing. MSK was involved in writing—reviewing and editing, and project administration.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, A., Siddiqui, A.A., Shahid, I. et al. Prognostic value of quality of life and functional status in patients with heart failure: a systematic review and meta-analysis. Egypt Heart J 76, 97 (2024). https://doi.org/10.1186/s43044-024-00532-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00532-z