Abstract
Background
Left ventricular ejection fraction falls when the myocardium has already lost a significant portion of its functional capacity. There are conflicting data on whether diastolic dysfunction precedes systolic dysfunction after cardiotoxic chemotherapy. We aimed to study systolic and diastolic dysfunction after cardiotoxic chemotherapy and whether diastolic dysfunction can predict subsequent risk of systolic dysfunction. It was an observational prospective cohort study, and patients receiving cardiotoxic chemotherapy were included. Baseline, demographic, and clinical details were recorded. Echocardiographic measurements of left ventricular systolic function, global longitudinal strain, and diastolic function were noted at baseline, three months, and 6 months.
Results
We included eighty patients. The mean age of the patients was 54.92 ± 7.6 years, predominantly females (80%). The mean left ventricular ejection fraction fell from 64.92 ± 1.96 to 60.97 ± 4.94 at 6 months. Low ejection fraction was seen in 8 (10%) patients at 6 months. The mean global longitudinal strain (GLS) at baseline was − 18.81 ± 0.797 and fell to − 17.65 ± 2.057 at 6 months, with 12 (15%) patients having low GLS (< − 18). Grade 1 diastolic dysfunction was seen in 22 (27.5%) patients, and grade 2 diastolic dysfunction was seen in 3 (3.8%) patients at 6 months. There was a significant decrease in E/A ratio (inflow early diastolic velocity/Inflow late diastolic velocity), mitral tissue Doppler velocity, and an increase in isovolumic relaxation time, mitral valve deceleration time, and E/e′ (inflow early diastolic velocity/tissue Doppler mitral annular velocity), at three months and 6 months. Ejection fraction at 6 months was significantly and negatively correlated with diastolic dysfunction at three months (r = − 0.595, p = 0.02).
Conclusions
Cardiotoxic chemotherapy is associated with early diastolic dysfunction. Early diastolic dysfunction predicts subsequent left ventricular systolic dysfunction.
Similar content being viewed by others
Background
Progress in early detection and treatment has improved the outlook for cancer patients [1]. Yet, chemotherapy's cardiotoxic effects significantly contribute to enduring health challenges and even fatalities [2, 3]. Long-term cancer survivors who have received cardio toxic chemotherapy are at increased risk of cardiac events [4]. Anthracyclines induces apoptosis of cardiomyocytes, oxidative stress and, mitochondrial dysfunction leading to left ventricular dysfunction [6, 7]. Cardio toxicity is seen in nine percent of patients receiving anthracyclines [8].
The assessment of cardiac function during chemotherapy primarily relies on measuring the left ventricular ejection fraction (LVEF) by echocardiography. Although commonly accepted, it can only diagnose left ventricular dysfunction only when the myocardium has already lost a significant portion of its functional capacity. As a result, it serves as a relatively late indicator of left ventricular dysfunction [9]. It is paramount to identify dependable, non-invasive techniques for the early detection of myocardial dysfunction before reaching the critical stage of left ventricular dysfunction.
Detecting alterations in cardiac parameters before a reduction in LVEF occurs is pivotal for identifying patients who could benefit from early cardioprotective interventions. This, in turn, significantly decreases the probability of interrupting effective systemic treatment, potentially jeopardizing patients' long-term well-being. Though different methods are utilized to detect early cardiotoxicity, there remains an unmet need regarding the most ideal way to detect early cardiotoxicity.
The pathogenesis of heart failure involves significant diastolic alterations [10, 11]. Diastolic dysfunction and its severity on echocardiography are associated with risk of overt heart failure on follow-up [12].
Prior research has shown that anthracyclines cause diastolic alterations. However, there are conflicting data on whether diastolic dysfunction precedes systolic dysfunction. While some studies [13, 14] have shown that diastolic dysfunction does not predate systolic dysfunction, other studies [15,16,17,18,19,20,21] have shown that abnormal diastology precedes systolic dysfunction. We designed this prospective study to understand how common diastolic dysfunction is after cardiotoxic chemotherapy and whether diastolic dysfunction can predict subsequent risk of systolic dysfunction.
Methods
Study design
Our longitudinal prospective cohort study was conducted over 24 months at our tertiary care hospital in the Department of Cardiology and Medical Oncology. The study was approved by the Institute Ethics Committee (IEC) with reference number of SIMS 131/IEC-SKIMS/2019-356. All patients provided written informed consent.
Study subjects
The inclusion criteria were: patients receiving cardiotoxic chemotherapy, expected survival of more than 6 months, age ≥ 18 years, normal left ventricular (LV) ejection fraction (≥ 52% for men and ≥ 54% for women) [22], with normal ECG, normal LV diastolic function, and those who gave written informed consent. The exclusion criteria were those with left ventricular (LV) systolic dysfunction, LV diastolic dysfunction of ≥ Grade 1 at baseline, suboptimal echocardiographic assessment, who have received chemotherapy in the past, current pregnancy, and breastfeeding. From cardiological point of view, we excluded breastfeeding women due to concerns about lactation-related physiological changes including fluctuations in fluid balance, electrolyte levels, and hormonal fluctuations, which could affect cardiac function and complicate the interpretation of echocardiographic results.
Clinical characteristics
We recruited cases from outpatient and inpatient medical oncology departments. Clinical details that were noted include the type of malignancy, chemotherapy used, clinical stage, hormone receptor status, any comorbidities (hypertension, diabetes, dyslipidemia, tobacco use, obesity), radiation treatment, and surgical details. Hypertension was determined by the 2018 American Heart Association/American College of Cardiology (AHA/ACC) guidelines [23]. Diabetes was characterized by a fasting blood glucose level greater than 126 mg/dl or an HbA1C level of 6.5 or higher or if the patient was already being treated for diabetes mellitus. Dyslipidemia was defined by the presence of any one of the following: LDL > 130 mg/dl, Total cholesterol > 200 mg/dl, and HDL < 40 mg/dl in men and < 50 mg/dl in women.
Echocardiographic assessment
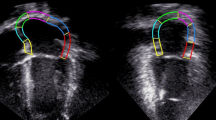
A baseline and follow-up echocardiograms were recorded at three months and 6 months. Transthoracic echocardiograms were performed in the cardiology department on GE Vivid E 95 machines (GE Healthcare, Milwaukee, Wisconsin). Echocardiography included assessment of the following parameters: Left ventricular ejection fraction (LVEF) was measured by modified Simpson’s method. Global longitudinal strain (GLS) was measured in the standard way [22]. The diastolic function parameters included mitral E velocity (mitral inflow early diastolic velocity), mitral A velocity (mitral inflow late diastolic velocity), E/A ratio, e′ (tissue Doppler mitral annular velocity), average E/e,’ mitral valve deceleration time (DT), isovolumic relaxation time (IVRT), peak tricuspid regurgitation (TR) systolic jet velocity. The left atrial (LA) volume index was determined by employing the both the 4-chamber and 2-chamber apical views just before the mitral valve (MV) opened. This calculation utilized the area-length method and was adjusted by dividing it by the individual's body surface area (BSA). Diastolic dysfunction was graded as per ASE guidelines [22]. Cardiac toxicity was diagnosed as a fall of more than ten percent in LVEF without any symptoms or more than a five percent decrease in LVEF along with the presence of heart failure symptoms [24]. Two experienced echocardiographers evaluated the echo cardio graphic parameters. The use of percentages to report the mean value was reported to give the coefficient of variation, which was calculated for intra-observer and inter-observer variability. The intra-observer coefficient of variation (CV) for LVEF was 2.4%. The inter-observer CV for LVEF was 3.4%. The intra-observer CV for GLS was 2.8%. The inter-observer CV for LVEF was 3.2%. The CV (both for intra- and inter-observer) for other diastolic echocardiographic parameters was less than 5%.
Statistical analysis
Sampling was done by purposive sampling technique. The calculation of required sample size was done using Open Epi statistical software version 3 using the following assumptions of a single population proportion formula for the descriptive studies; Prevalence of chemotherapy associated left ventricular dysfunction 6%, with confidence limit of 95% and precision, which was set at 0.05. Thus, the sample came out to be 77. We recruited a total of 80 patients. The data were analyzed by Statistical Package for Social Sciences (SPSS Version 20.0, SPSS Inc., Chicago, Illinois, USA). Continuous variables were expressed as mean ±standard deviation and categorical variables as frequencies and percentages. Pearson’s Chi-square was used for inferential statistics, two-sided p values were reported, and a P value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics
Initially, ninety patients were enrolled. However, five patients were excluded at baseline due to suboptimal echocardiographic assessment of diastolic dysfunction, and another five patients were lost to follow-up. So, a total of eighty patients were included in the final analysis. The mean age of the patients was 54.92 ± 7.6 years, predominantly females (80%). The baseline clinical, demographic, and echocardiographic variables are shown in Table 1. All baseline echocardiographic variables were within normal range. The different type of malignancies included 43 (53.75%) Her 2-positive breast cancer cases, 17 (21.25%), Her 2-negative breast cancer cases, and 20 (25%) Hodgkins lymphoma cases. The cumulative dose of anthracycline was 323.40 ± 101.34 mg/m2 (127.51–430.53 mg/m2).
Changes in diastolic function
At 6 months of follow-up, grade 1 diastolic dysfunction was seen in 22 (27.5%) patients, and grade 2 diastolic dysfunction was seen in 3 (3.8%) patients. The remaining 55 (68.8%) of patients had no diastolic dysfunction. The mean E/A ratio decreased significantly over 6 months (Fig. 1a). There were also a modest significant reduction in lateral and septal e′ (Fig. 1b) and an increase in the E/e′ ratio. LA volume index also increased significantly at 6 months (Table 2). The DT and IVRT (Fig. 2a, b) also increased significantly over time (Table 2). The logistic regression analysis showed radiation therapy, age ≥ 50 years and BMI ≥ 27 kg/m2 to be significantly associated with occurrence of diastolic dysfunction. However, there was no association with diabetes mellites, tobacco use or hypertension with diastolic dysfunction (Table 3).
Changes in left ventricular systolic function and GLS.
Low ejection fraction (systolic dysfunction) was seen in 8 (10%) patients at 6 months. The mean LVEF fell from 64.92 ± 1.96 to 60.97 ± 4.94 at 6 months (Fig. 3a). The mean global longitudinal strain (GLS) at baseline was − 18.81 ± 0.797. At three months, mean GLS reduced to − 18.46 ± 1.793, with 9 (11.25%) patients having low GLS (< − 18). At 6 months, a significant decrease in mean GLS was noted, i.e., 17.65 ± 2.057, with 12 (15%) patients having low GLS (< − 18) (Fig. 3b).
Association between diastolic dysfunction and systolic dysfunction
We analyzed whether diastolic dysfunction at three months had any correlation with the development of systolic dysfunction at 6 months. Pearson’s product moment of correlation analyses was applied. It was found that ejection fraction at 6 months was significantly and negatively correlated with diastolic dysfunction at three months (r = − 0.595, p = 0.02). LVEF at 6 months was inversely related to the diastolic dysfunction grade at three months. We also analyzed the association between LVEF and diastolic dysfunction at 6 months and found a significant correlation between the two at 6 months. (r = − 0.656, p = 0.01). The mean LVEF was significantly lower in those with grade ≥ 1 diastolic dysfunction than those without diastolic dysfunction (58.20 ± 6.819 vs. 62.60 ± 2.096) (p = 0.01). The mean difference of LVEF in patients having diastolic dysfunction Vs no diastolic dysfunction was -4.40 at 6 months.
Relation between GLS and ejection fraction
There was no significant correlation between the GLS at and LVEF at three-month follow-up. (r = 0.195, p = 0.083). However, it was found that GLS at three months and LVEF at 6 months had positive correlation (r = 0.680, p < 0.01). Patients showing a fall in ejection fraction at 6 months had a prior decrease of GLS at three months (Table 4).
Discussion
The present study evaluated the left ventricular diastolic function parameters and their relationship with systolic dysfunction in cancer chemotherapy patients. Our salient findings include: (1) There is early worsening of diastolic dysfunction, and it persists over time. (2) The early diastolic dysfunction is associated with subsequent systolic dysfunction. (3) Ten percent of our patients developed significant fall in LVEF over 6 months.
Around one-third of our patients showed evidence of diastolic dysfunction at 6 months. The E/A ratio decreased over three months and worsened up to 6 months of follow-up. Both DT and IVRT increased as early as three months, with a sustained modest decrease at 6 months. The tissue Doppler velocities also decreased significantly. E/e′ showed a modest increase in follow-up. Our study showed an initial E/A ratio average of 1.36, decreasing to 1.11 after 6 months. This aligns with findings from Upshaw et al. [15], (baseline E/A ratio: 1.2), Boyd et al. [25], (baseline E/A ratio: 1.13), and Cochera et al. [26], (initial E/A ratio: 1.3), all demonstrating a decrease in E/A ratio over time. These consistent trends across studies suggest a pattern of declining E/A ratios in similar patient populations, highlighting a consistent pattern across different studies. Our study noted an increase in DT from 179 initially to 190 ms at the 6-month follow-up, consistent with observations reported by Serrano et al. [17], (186 to 201 ms). However, findings regarding IVRT varied among studies; Stoodley et al. [19], reported a significant increase in IVRT as early as one week, whereas Boyd et al. [25] found no significant change in IVRT during follow-up. The LA volume (ml/BSA) in our study also significantly increased from 21.59 ± 2.29 to 24.56 ± 2.15 at 6 months. However, it did not show any significant change at three months. Although it is a significant method for evaluating remodeling and indirectly assessing LA function, the indexed LA volume exhibits limited sensitivity during the initial phase [27]. Previous studies have shown that LA volume index may not change till 12 months of follow-up [28]. Similar findings were noted by Upshaw et al. [15]. A standard echocardiographic examination is incomplete without assessing diastology. Nevertheless, when monitoring for cardiotoxicity, the emphasis has traditionally been on assessing LV systolic function. Damage to the myocardial membrane and mitochondria has been observed after typical clinical doses of doxorubicin and could lead to impaired left ventricular relaxation and filling [29, 30]. The effects of doxorubicin on systolic and diastolic dysfunction vary between the early and late stages. Initially it can increase the systolic and diastolic function by increasing intramyocardial calcium levels or catecholamines [30,31,32]. However, on long term it decreases the systolic and diastolic dysfunction by direct myocardial injury. However, in children it has shown to acutely deteriorate systolic and diastolic function [20].
Our study population had a higher percentage of hypertensive patients (57.5%) and diabetic patients (47.5%) than other studies. This may be due to the high prevalence of diabetes and hypertension in our local population [33, 34]. Besides, sampling bias may also be contributory. Increasing age, BMI and radiotherapy were positively associated with diastolic dysfunction at 6 months. Age is an established risk factor for cardiotoxic chemotherapy [35, 36]. Increasing BMI has also been associated with worsening cardiac function following anthracycline treatment [37, 38]. Fumoleau et al. [37] found that a BMI of more than 27 kg/m2 significantly correlated with left ventricular dysfunction after epirubicin treatment, with an incidence of 1.8% versus 0.9% in patients with a BMI less than 27 kg/m2. The different mechanisms suggested include higher oxidative stress, high peripheral resistance, and chronic volume overload in obese patients. Radiation therapy is known to cause heart failure with preserved ejection fraction by myocardial fibrosis and left ventricular hypertrophy [39]. One recent study [40] found that radiation therapy is associated with diastolic dysfunction even in those without any systolic dysfunction as determined by GLS. There was no correlation with diabetes mellitus, tobacco use, or hypertension in our study subjects. We suggest the necessary measures to improve risk factors linked to diastolic dysfunction like regular physical activity and maintaining optimal weight. This can potentially lead to a delay in worsening of left ventricular dysfunction.
Association with systolic dysfunction
Our study adds to growing body of knowledge about early impairment of diastolic dysfunction and its relation with subsequent systolic dysfunction. Diastolic dysfunction at three months significantly correlated with depression of ejection fraction at 6 months. LVEF at 6 months was inversely related to the diastolic dysfunction grade at three months. Diastolic impairment before a fall of LVEF is known to occur in coronary artery disease, diabetes, and hypertension [41, 42]. Though some studies [13, 14] have shown simultaneous impairment of left ventricular systolic and diastolic impairment, the most extensive study by Upshaw et al. [15] showed that worsening diastolic dysfunction is associated with increased systolic dysfunction on follow-up. The multicenter study by Calabrese et al. [21], reported LV diastolic dysfunction in 36% of patients as early as one week after starting chemotherapy. According to Stoddard et al. [29], an increase of more than 37% in IVRT demonstrated a sensitivity of 78% and a specificity of 88% for identifying the future development of doxorubicin-induced systolic dysfunction. The mechanism of early diastolic impairment is not yet clear. The probable hypothesis is that the left ventricular endocardium is more sensitive to microvascular abnormalities and interstitial fibrosis, resulting in early impairment of subendocardial function reflected by decreased left ventricular longitudinal strain and abnormal diastolic parameters [43, 44]. With the progression of the disease, the left ventricular ejection fraction also falls due to the involvement of mid-myocardial fibers [45].
Global longitudinal strain and LVEF
Systolic dysfunction was seen in 8 (10%) patients at 6 months. The mean LVEF fell from 64.92 ± 1.96 to 60.97 ± 4.94 at 6 months. The mean global longitudinal strain (GLS) at baseline was − 18.81 ± 0.797 and fell to − 17.65 ± 2.057 at 6 months with 12 (15%) patients having low GLS (< − 18). Our findings are similar to those of Gripp et al. [46], who found that in breast cancer patients undergoing anthracycline and/or trastuzumab treatment, those developing cardiotoxicity showed a significant fall in mean left ventricular GLS compared to baseline at the third month. According to Negishi et al. [47], a reduction of over 11% in GLS indicated a long-term decrease in LVEF and cardiotoxicity in patients who received anthracyclines. Several hypotheses have been proposed to explain anthracycline-induced left ventricular dysfunction. The mechanisms implicated include oxidative stress, lipid peroxidation, protein synthesis inhibition and altered calcium load [4, 5]. Different studies have also shown anthracyclines causing altered gene expression [6]. We also noted that the LV GLS change occurred from the third month onward. In contrast, the ejection fraction changed only in the 6th month. By assessing regional myocardial function, strain serves as a potentially more sensitive indicator of early myocardial dysfunction [48]. Besides, strain is easy to use and reproducible. The various limitations in using LVEF for detecting myocardial damage include measurement errors, relatively late decline when considerable myocardial damage has already occurred, and dependence on preload and afterload. All these factors result in errors that affect the validity of LVEF in assessing early myocardial damage [47]. Besides, anthracyclines initially damage the endocardial layer. As endocardial layer is mainly formed by longitudinal fibers, the early endocardial dysfunction is best picked up by GLS rather than LVEF [49].
Limitation
It is as single-center study with short duration of follow-up. There is uncertainty of long-term impact of early diastolic dysfunction. Besides, we did not use other imaging modalities (3D echo, cardiac MRI) and biomarkers (brain natriuretic peptide and troponin).
Conclusions
Cardiotoxic chemotherapy is associated with significant diastolic and systolic left ventricular dysfunction. Ten percent of our cohort showed evidence of reduced LVEF at 6 months and one-third of patients showed diastolic dysfunction at 6 months. Increasing age and BMI were associated with early diastolic dysfunction. Diastolic dysfunction occurs early and predicts subsequent LV systolic dysfunction. Long-term studies are needed to determine whether early diastolic dysfunction is associated with long-term risk of heart failure.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- LVEF:
-
Left ventricular ejection fraction
- GLS:
-
Global longitudinal strain
- E :
-
Inflow early diastolic velocity
- A :
-
Inflow late diastolic velocity
- e′:
-
Tissue Doppler mitral annular velocity
- DT:
-
Mitral valve deceleration time
- IVRT:
-
Isovolumic relaxation time
- TR:
-
Tricuspid regurgitation
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A (2014) Cancer treatment and survivorship statistics. CA Cancer J Clin 64(4):252–271
Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH (2007) Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol 25(25):3808–3815
Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD (2016) Cardiovascular disease mortality among breast cancer survivors. Epidemiology 27(1):6–13
Carver JR, Shapiro CL, Ng A, Jacobs L, Schwartz C, Virgo KS, Hagerty KL, Somerfield MR, Vaughn DJ (2007) ASCO Cancer Survivorship Expert Panel: American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol 25(25):3991–4008
Demant EJ (1991) Inactivation of cytochrome c oxidase activity in mitochondrial membranes during redox cycling of doxorubicin. Biochem Pharmacol 41(4):543–552
Palmeira CM, Serrano J, Kuehl DW, Wallace KB (1997) Preferential oxidation of cardiac mitochondrial DNA following acute intoxication with doxorubicin. Biochim Biophys Acta 1321:101–106
Mimnaugh EG, Trush MA, Bhatnagar M, Gram TE (1985) Enhancement of reactive oxygen-dependent mitochondrial membrane lipid peroxidation by the anticancer drug adriamycin. Biochem Pharmacol 34:847–856
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F et al (2015) Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 131:1981–1988
Cochet A, Quilichini G, Dygai-Cochet I, Touzery C, Toubeau M, Berriolo-Riedinger A et al (2011) Baseline diastolic dysfunction as a predictive factor of trastuzumab-mediated cardiotoxicity after adjuvant anthracycline therapy in breast cancer. Breast Cancer Res Treat 130:845–854
Faris R, Coats AJ, Henein MY (2002) Echocardiography-derived variables predict outcome in patients with nonischemic dilated cardiomyopathy with or without a restrictive filling pattern. Am Heart J 144:343–350
Shah AM, Claggett B, Sweitzer NK et al (2014) Cardiac structure and function and prognosis in heart failure with preserved ejection fraction: findings from the echocardiographic study of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) Trial. Circ Heart Fail 7:740–751
Kane GC, Karon BL, Mahoney DW et al (2011) Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA 306:856–863
Reuvekamp EJ, Bulten BF, Nieuwenhuis AA, Meekes MR, de Haan AF, Tol J, Maas AH, Elias-Smale SE, de Geus-Oei LF (2016) Does diastolic dysfunction precede systolic dysfunction in trastuzumab-induced cardiotoxicity? Assessment with multigated radionuclide angiography (MUGA). J Nucl Cardiol 23(4):824–832
Lange SA, Ebner B, Wess A, Kögel M, Gajda M, Hitschold T, Jung J (2012) Echocardiography signs of early cardiac impairment in patients with breast cancer and trastuzumab therapy. Clin Res Cardiol 101(6):415–426
Upshaw JN, Finkelman B, Hubbard RA, Smith AM, Narayan HK, Arndt L, Domchek S, DeMichele A, Fox K, Shah P, Clark A, Bradbury A, Matro J, Adusumalli S, Carver JR, Ky B (2020) Comprehensive assessment of changes in left ventricular diastolic function with contemporary breast cancer therapy. JACC Cardiovasc Imaging 13:198–210
Ho E, Brown A, Barrett P, Morgan RB, King G, Kennedy MJ, Murphy RT (2010) Subclinical anthracycline- and trastuzumab-induced cardiotoxicity in the long-term follow-up of asymptomatic breast cancer survivors: a speckle tracking echocardiographic study. Heart 96(9):701–707
Serrano JM, Gonzalez I, Del Castillo S et al (2015) Diastolic dysfunction following anthracycline-based chemotherapy in breast cancer patients: incidence and predictors. Oncologist 20:864–872
Florescu M, Magda LS, Enescu OA, Jinga D, Vinereanu D (2014) Early detection of epirubicin-induced cardiotoxicity in patients with breast cancer. J Am Soc Echocardiogr 27:83–92
Stoodley PW, Richards DA, Boyd A et al (2013) Altered left ventricular longitudinal diastolic function correlates with reduced systolic function immediately after anthracycline chemotherapy. Eur Heart J Cardiovasc Imaging 14:228–234
Ganame J, Claus P, Eyskens B et al (2007) Acute cardiac functional and morphological changes after anthracycline infusions in children. Am J Cardiol 99:974–977
Calabrese V, Menna P, Annibali O et al (2018) Early Diastolic dysfunction after cancer chemotherapy: primary endpoint results of a multicenter cardiooncology study. Chemotherapy 63:55–56
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 29(4):277–314
Whelton PK, Carey RM, Aronow WS et al (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension 71(6):e13–e115
Anqi Y, Yu Z, Mingjun X et al (2019) Use of echocardiography to monitor myocardial damage during anthracycline chemotherapy. Echocardiography 00:1–8
Boyd A, Stoodley P, Richards D et al (2017) Anthracyclines induce early changes in left ventricular systolic and diastolic function: a single centre study. PLoS ONE 12(4):e0175544
Cochera F, Dinca D, Bordejevic DA, Citu I, Mavrea A, Andor M, Tomescu M (2018) Nebivolol effect on doxorubicin-induced cardiotoxicity in breast cancer. Cancer Manag Res 2018(10):2071–2081
Pathan F, D’Elia N, Nolan MT, Marwick TH, Negishi K (2017) Normal ranges of left atrial strain by speckle-tracking echocardiography: a systematic review and meta-analysis. J Am Soc Echocardiogr 30(1):59-70.e8. https://doi.org/10.1016/j.echo.2016.09.007
Timóteo AT, Moura Branco L, Filipe F, Galrinho A, Rio P, Portugal G et al (2019) Cardiotoxicity in breast cancer treatment: What about left ventricular diastolic function and left atrial function? Echocardiography 36(10):1806–1813
Stoddard MF, Seeger J, Liddell NE et al (1992) Prolongation of isovolumetric relaxation time as assessed by Doppler echocardiography predicts doxorubicin-induced systolic dysfunction in humans. J Am Coll Cardiol 2(1):62–69
Marchandise B, Schroeder E, Bosly A et al (1989) Early detection of doxorubicin cardiotoxicity: interest of Doppler echocardiographic analysis of left ventricular filling dynamics. Am Heart 118(1):92–98
Van Boxtel CJ, Olson RD, Boerth RC et al (1978) Doxorubicin: inotropic effects and inhibitory action on ouabain. J Pharmacol Exp Ther 207(2):277–283
Gosálvez M, van Rossum GD, Blanco MF (1979) Inhibition of sodium-potassium-activated adenosine 5′-triphosphatase and ion transport by adriamycin. Cancer Res 39(1):257–261
Zarka AM, Riyaz AM et al (2016) Prevalence and determinants of hypertension in Kashmir: a cross sectional study. IOSR J Dent Med Sci IOSR-JDMS 15(6):57–64
Mathur P, Leburu S, Kulothungan V (2022) Prevalence, awareness, treatment and control of diabetes in India from the countrywide national NCD monitoring survey. Front Public Health 14(10):748157
ShanK LAM, Young JB (1996) Anthracycline induced cardiotoxicity. Ann Intern Med 125:47–58
VonHoff DD, Layard MW, Petal B (1979) Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med 91:710–717
Fumoleau P, Roche H, Kerbrat P et al (2006) Long term cardiac toxicity after adjuvant epirubicin based chemotherapy in early breast cancer: French Adjuvant Study Group results. Ann Oncol 17:85–92
Dranitsaris G, Rayson D, Vincent M et al (2008) The development of a predictive model to estimate cardiotoxic risk for patients with metastatic breast cancer receiving anthracyclines. Breast Cancer Res Treat 107:443–450
Saiki H, Petersen IA, Scott CG (2017) Risk of heart failure with preserved ejection fraction in older women after contemporary radiotherapy for breast cancer. Circulation 135:1388–1396
Tuohinen SS, Skyttä T, Huhtala H, Poutanen T, Virtanen V, Kellokumpu-Lehtinen PL, Raatikainen P (2021) 3-year follow-up of radiation-associated changes in diastolic function by speckle tracking echocardiography. JACC CardioOncol 3(2):277–289
Fouad FM, Slominski JM, Tarazi RC (1984) Left ventricular diastolic function in hypertension: relation to left ventricular mass and systolic function. J Am Coll Cardiol 3:1500–1506
Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ (2003) Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. J Am Med Assoc 289:194–202
Martinez DA, Guhl DJ, Stanley WC, Vailas AC (2003) Extra cellular matrix maturation in the left ventricle of normal and diabetic swine. Diabetes Res Clin Pract 59:1–9
Lumens J, Delhaas T, Arts T, Cowan BR, Young AA (2006) Impaired subendocardial contractile myofiber function in asymptomatic aged humans, as detected using MRI. Am J Physiol Heart Circ Physiol 291:H1573–H1579
Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF (2008) Preserved left ventricular twist and circumferential deformation, but depressed longitudinal and radial deformation in patients with diastolic heart failure. Eur Heart J 29:1283–1289
Gripp EA, Oliveira GE, Feijó LA, Garcia MI, Xavier SS, Sousa AS (2018) Global longitudinal strain accuracy for cardiotoxicity prediction in a cohort of breast cancer patients during anthracycline and/or trastuzumab treatment. Arq Bras Cardiol 110(2):140–150
Negishi T, Negishi K (2017) Echocardiographic evaluation of cardiac function after cancer chemotherapy. J Echocardiogr 642–8:1–8
D’hooge J, Heimdal A, Jamal F et al (2000) Regional strain and strain rate measurements by cardiac ultrasound: principles, implementation and limitations. Eur J Echocardiogr 1:154–170
Mele D, Nardozza M, Spallarossa P, Frassoldati A, Tocchetti CG, Cadeddu C et al (2016) Current views on anthracycline cardiotoxicity. Heart Fail Rev 21:621–634
Acknowledgements
We want to thank Mr Syed Bilal and Mr Syed Mudasir (Echocardiography technicians) for their technical support during the study.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. HR, AR, AM, and FG compiled all data. SM, SK, AL, and KA collected review of literature. AR and HR wrote the manuscript. AR, IH, and HR reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institute Ethics Committee (IEC), Sheri-Kashmir Institute of Medical Sciences, Srinagar, Government of J & K, India. The IEC committee is registered with DCG(I) under registration No. ECR/799/INST/JK/2016/RR-21. The date of approval of the study is 19/03/2019, and the reference number of approval is SIMS 131/IEC-SKIMS/2019-356.All participants provided informed written consent to participate in the study. Informed written consent from parents/legal guardians was taken for patients under 16 years of age.
Consent for publication
The authors affirm that human research participants provided informed consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rashid, H., Rashid, A., Mattoo, A. et al. Left ventricular diastolic function and cardiotoxic chemotherapy. Egypt Heart J 76, 45 (2024). https://doi.org/10.1186/s43044-024-00476-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00476-4