Abstract
Background
Heart failure (HF) poses a significant public health challenge throughout the world and Morocco. Our objective was to delineate the epidemiological characteristics of Moroccan patients living with chronic heart failure and to identify prognostic factors correlated with CHF mortality.
Results
A total of 1344 patients participated in this study, with survival rates at 3, 6, and 10 years recorded at 75.2%, 60%, and 34%, respectively. During the follow-up, 886 patients succumbed, representing a mortality rate of 65.9%. A Cox regression model, utilizing baseline candidate variables, was developed to predict cardiovascular (CV) mortality. Predictors all of which had a P value less than 0.05 included age, left ventricular ejection fraction (EF) at commencement (< 35%), hypertension, male sex, anemia, creatinine levels, and the number of hospitalizations due to HF decompensation. Notably, the frequency of hospitalizations emerged as the most potent predictor of mortality, with an HR of 2.5 (95% CI [2–2.9]). Almost 90% of patients with three or more readmissions for HF decompensation experienced mortality by the follow-up’s conclusion.
Conclusions
This study offers valuable insights into risk factors and clinical outcomes in HF patients in Morocco. Factors such as male gender, advanced age, a history of hypertension, lower systolic blood pressure, rehospitalizations for HF decompensation, low left ventricular ejection fraction, anemia, and elevated creatinine levels were associated with increased mortality. Medical and health services managers should be aware of the substantial burden and future challenges posed by HF in Morocco, prompting the adoption of multidisciplinary strategies for its management and care.
Similar content being viewed by others
Background
The historical roots of heart failure extend to antiquity, with symptoms purportedly described over 3500 years ago in the remains discovered within a tomb in the Valley of the Queens in Egypt [1]. Since that time, heart failure has posed a substantial and enduring challenge to the field of medicine. Despite advancements in science, technology, and an enhanced understanding of heart failure physiopathology, it remains a substantial challenge to health care professionals.
The American Heart Association defines Heart Failure (HF) as a complex clinical syndrome that results from a functional or structural heart anomaly impairing ventricular filling or ejection of blood to the systemic circulation [2].
Heart failure is a global public health concern affecting millions of people and posing an important social and economic burden more pronounced in developing countries [3]. Morocco is an emerging country experiencing an important transformation in the composition and habits of its society. In fact, like North African countries its population adopted a Western lifestyle in the last decades [4] which has led to an increase in the incidence of Diabetes, Hypertension, obesity, and other Cardiovascular risk factors; Causing an increase in cardiovascular disease and heart failure incidence. Nearly one million Moroccans are living with HF and this number will increase in the future years [5].
The World Heart Federation claims in its annual report of 2023 that cardiovascular diseases (CVDs) are the leading cause of death globally, taking an estimated 20.3 million lives in 2021. Lindstrom et al. [6] the same report predicted that one-third of cardiovascular deaths can be prevented by improving cardiovascular Health, especially in developing countries. Some studies have also reported a great disparity between HF mortality and prognosis between low- and middle-income countries and high-income countries with some authors stating that the lack of adherence to optimal medical-guided therapy may have a key role in these disparities [7, 8].
Prior investigations into heart failure in Morocco have predominantly concentrated on the epidemiological dimensions of the condition, with limited information pertaining to prognosis and predictors of mortality in this geographical context.
The present study endeavors to contribute a more thorough understanding of the burden imposed by heart failure in Morocco, aiming to elucidate the factors that influence its outcomes within population and to facilitate the provision of more efficient and targeted health services tailored to the specific needs of the Moroccan community.
Methods
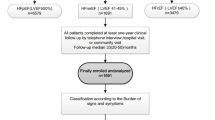
We conducted a retrospective observational investigation that enrolled patients diagnosed with heart failure with reduced ejection fraction (HFrEF) or heart failure with mildly reduced ejection fraction (HFmEF). The study was conducted within the Cardiology department of Ibn Rochd Hospital in Casablanca, spanning from January 2012 to December 2021, with subsequent follow-up until March 2023. Data were systematically gathered from the Heart Failure Registry, and both mortality and incidents of HF decompensation were obtained through direct communication with patients and their families via telephone.
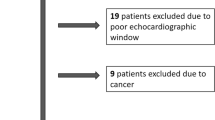
Diagnostic assessments were carried out using Vivid 7 (General Electrics) echocardiography, with left ventricular ejection fraction (LVEF) estimated using Simpson’s method. Inclusion criteria comprised patients exhibiting reduced or mildly reduced ejection fraction, while those with missing data and individuals with LVEF exceeding 49% were excluded.
For statistical analyses, continuous data are expressed using means and standard deviations (SD). Categorical variables were expressed as percentages and subjected to the chi-square test for comparison. Given that the primary endpoint was mortality, survival over time was calculated using the Kaplan–Meier method. Differences in mortality between subgroups were assessed using the log-rank test. Predictors of all-cause mortality were identified through a univariate Cox proportional hazard regression model. All statistical analyses were performed using IBM SPSS Statistics version 23.
Results
Patient characteristics
The study commenced with the inclusion of a total of 1546 patients, from which 202 individuals were subsequently excluded due to insufficient data, resulting in a final cohort of 1344 patients over a ten-year follow-up period. A comprehensive summary of pertinent patient information is presented in Table 1.
Among the included patients, 61.6% were male, and the mean observed age was 61.48 years. Ischemic heart disease was identified as the primary etiology of heart failure in 81.02% of cases. The prevalence of diabetes and hypertension within the entire patient cohort was noted at 40% and 51.4%, respectively. The median value of left ventricular ejection fraction was determined to be 36.2%.
Clinical outcomes
At the conclusion of the follow-up period, the overall mortality rate stood at 65.92%, indicating that 886 patients within the cohort had passed away. Additionally, the survival rates at 3, 6, and 10 years were 75.2%, 60%, and 34%, respectively.
Prognostic predictors
Upon univariate Cox regression analysis, several factors were identified as prognostic predictors associated with a higher mortality rate. These factors include male gender, advanced age, lower systolic blood pressure, a history of hypertension, two or more rehospitalizations for heart failure (HF) decompensation, left ventricular ejection fraction (LVEF) below 35%, and elevated levels of creatinine, as detailed in Table 2.
Time-to-event analysis
The overall survival curve is depicted in Fig. 1, while Figs. 2, 3, and 4 illustrate survival curves across different subgroups. Notably, patients with two or more hospitalizations due to heart decompensation exhibited the most pronounced mortality rate, with nearly all patients experiencing three or more hospitalizations succumbing by the conclusion of the follow-up period (P < 0.001).
Patients with lower LVEF (< 35%) also demonstrated higher mortality, with a distinct separation of survival curves evident after 12 months (P < 0.001). Male patients exhibited a slightly elevated mortality rate compared to their female counterparts (P = 0.04). Finally, creatinine levels exhibited a proportional correlation with the mortality rate.
Discussion
We sought to explore the aspects of chronic heart failure in the Moroccan population; the overall 10-year all-cause mortality was 65.9% with a median follow-up of 58 months. similar findings were found by A recent meta-analysis that included 60 studies mostly conducted in Europe or North America where survival rate of 1, 2, 5, and 10 years was 86.5%, 72.6%, 56.7%and 34.9% respectively [9]. Another study that enrolled participants from low-income countries concluded a significantly higher one-year mortality in Africa (30.6%), and Asia (13.1%), compared to patients from South America (8.6%) and the Middle East (9.1%) P < 0.001 [10]. These results may be underestimated for many reasons: HF is underdiagnosed in these countries, and guideline-directed medical therapy GDMT is not often applicable to treat patients, and poor-quality health services. The absence of Awareness and Prevention programs launched in these countries. Some studies report a twofold increase in the risk of in-hospital mortality and post-discharge events compared to high-income countries [11].
The predominance of the male population (nearly two-thirds) may be explained by tobacco being an important risk factor of ischemic heart disease (more than 80% of HF etiology in our study) predominant in the Moroccan male population. Male gender was also an independent risk factor for all-cause mortality. A study conducted in Saudi Arabia found no significant difference in survival between women and men [12]. Our findings were reported in a recent UK study in which women had a 14% age‐adjusted lower risk of all‐cause mortality [13]. However, a recent Canadian study found that women remain at higher risk than men of dying or developing heart failure in the subsequent 5 years after acute coronary syndrome [14]. These conflicting data may be due to different population characteristics and health care systems.
Age was a strong predictor of mortality, and elderly patients with CHF have a poor prognosis, particularly if their heart failure symptoms are caused by LV systolic dysfunction [15]. As living conditions improve, the elderly population in Morocco will increase significantly by 2030. The High Commission for Planning (HCP) projects a significant demographic shift in Morocco by 2030, with the senior population aged 70 and above exceeding six million, representing a substantial 42% increase from 2021. This transformative surge is anticipated to reshape the societal landscape, as seniors are expected to constitute 15.4% of the total population, as highlighted in the HCP report.
The rehospitalization rate emerged as the foremost risk factor for mortality in this study, revealing a threefold increase in overall heart failure mortality. Although this association is acknowledged in existing literature [16, 17], the resource constraints in Morocco have resulted in the reservation of heart failure hospitalization predominantly for critical cases. As illustrated in Fig. 4, a substantial proportion of patients with three or more hospitalizations experienced mortality over a 10-year follow-up. These observations underscore heart failure decompensation as a pivotal factor indicative of structural and functional cardiac anomalies.
Whether the mortality of patients with acute heart failure onset is higher than those with acute decompensation of chronic heart failure is still subject to debate with conflicting results in recent studies [18, 19] Unfortunately, we could not analyze it due to lack of data. What is sure is that lack of treatment adherence is strongly correlated to mortality and rehospitalization [20]. Our patients had a significant lack of adherence to medical therapy and only a few of them had reached the maximum dose of beta-blockers and ACE making the prevention of cardiovascular morbidity, close follow, and patient education crucial for reducing their mortality in our country.
A reduced left ventricular ejection fraction (LVEF) is indicative of the severity of infarcted zones and fibrosis, and it is consistently linked to an elevated risk of arrhythmia and sudden cardiac death, as corroborated by numerous studies [21, 22]. In our investigation, as depicted in Fig. 3, an LVEF lower than 30% exhibited a statistically significant association with mortality, as indicated by a log-rank value of 0.02. These findings underscore the prognostic relevance of LVEF in our study cohort, aligning with the established understanding of its implications for adverse cardiac outcomes.
In this study, the presence of anemia demonstrated a significant association with higher mortality, a result consistent with findings reported in numerous other studies. The relationship between anemia and mortality was proportional to the severity of the anemia many studies tried to find an explication to this: the difficulty of management of HF patients with anemia, accentuated inflammatory reaction, and nutritional deficiency of iron may all play a role in this higher mortality [23, 24]. Whether the anemia is a consequence of severe HF or a cause of poor outcomes is still an enigma [25]. Hence the benefit of blood transfusion to improve the prognosis of these patients is still a subject of debate as the transfusion therapy can lead to volume overload and ischemic events in HF patients [26]. Some studies in hemodynamically stable cardiac patients suggest reserving blood transfusion to patients with a Hb level below 80 g/L [27].
C-reactive protein is a direct marker of Inflammation which plays an important role in HF pathophysiology[28]. This study found a strong correlation between C-reactive protein and mortality, this result was also found in a Japanese study published in 2019 [29], and the mechanism in which inflammation increases mortality is not fully understood; it is believed that it may result from both a direct myocardial release in consequence of hemodynamic overload and systemic cellular production caused by reduced tissue perfusion and associated hypoxia [30]. Hence, the use of CRP as prognostic marker may be important in the stratification of mortality risk among HF patients.
Our study found that a decrease in renal function was associated with higher overall mortality, and many other studies shared the same finding [31, 32]. This was not surprising for the decrease in renal function which is a direct reflection of deteriorating organ perfusion. The major cause of renal function deterioration is either type 1 CRS (acute cardio-renal syndrome) or type 2 CRS (chronic cardio-renal syndrome). While both hypoperfusion and high glomerular pressure play a role in renal deterioration, type 2 CRS seems to have higher RAAS and SNS activation [33]. Hence, these patients benefice greatly from beta-blockers and ACE\ARBS treatment.
Blood pressure was inversely correlated with mortality; an Italian study that enrolled 6975 patients shared the same finding [34] and lower blood pressure may be a sign of lower cardiac output which is related to impaired ventricular function scaring and hence high risk of death.
Despite the robust identification of hyponatremia and diabetes as significant risk factors in prior studies, [35,36,37], our investigation failed to establish a significant correlation between these factors and mortality within our study cohort. It is noteworthy to acknowledge that this lack of correlation may be attributed to the inherent limitation of our study, specifically the relatively constrained size of the study population. The restricted sample size may have influenced the statistical power and, consequently, the ability to detect significant associations.
A Scottish study published in 2017 has found that HF is as “malignant” as some of the common cancers in both men and women [36, 37]. It is believed that heart failure gravity is underestimated by the general population even in rich countries [38] and that spreading awareness has an important impact on reducing cardiovascular-related morbidity and mortality [39]. This will have a greater effect in developing countries like Morocco.
Linking these insights to the context of Morocco and other developing countries, the adoption of a Mediterranean lifestyle emerges as a potential strategy for cardiovascular health as a recent British study published in 2022 found that promoting Mediterranean and low-fat diets reduced cardiovascular mortality, myocardial infarction, and the incidence of strokes as stated by [40].
The challenges faced in heart failure management in Morocco highlight areas where healthcare infrastructure and practices need serious improvement. Limited resources, access to specialized care, population aging, and gaps in patient education can hinder optimal heart failure management.
Conclusions
This study provides valuable insights into risk factors and clinical outcomes in HF patients in Morocco, male gender, age, low systolic blood pressure, history of hypertension, rehospitalizations for HF decompensation, low LVEF anemia, and high levels of creatinine were associated with increased mortality.
The implications of these findings are substantial for medical and health services managers. The identified risk factors underscore the significant burden and forthcoming challenges posed by HF in Morocco. To address this, a strategic shift toward multidisciplinary approaches in the management and care of this disease is imperative. By understanding these factors, healthcare professionals and administrators can develop nuanced strategies tailored to the specific needs of HF patients in the Moroccan context, potentially optimizing outcomes and resource utilization.
Limitations
This study is subject to several limitations that should be noted. First, 15% of the population had to be excluded due to missing data. Additionally, the analysis of smoking-related data was not feasible due to a lack of information, and certain variables, such as C-reactive protein, had more than 25% missing values. The study’s design also prevented us from differentiating between cardiovascular and all-cause mortality, primarily due to the absence of medical informatization in Morocco.
It is important to highlight that the sample size of 1344 patients may not be representative of the heart failure population, which is estimated to be nearly one million patients. Despite this limitation, the study offers valuable insights into the characteristics of the included cohort.
Due to the design of the study, a comprehensive reexamination of all patients for the evaluation of Guideline-Directed Medical Therapy (GDMT) was not conducted. Instead, our focus was directed solely toward the assessment of heart failure medications.
We acknowledge the need for caution in generalizing these findings, given the current limitations. We hope that a future research on a national and potentially Arabic scale, with a larger and more diverse population, would contribute to confirming our current findings and provide a more comprehensive assessment of the impact of Guideline-Directed Medical Therapy (GDMT) adherence on heart failure patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- CRP:
-
C-reactive protein
- DBP:
-
Diastolic blood pressure
- ESRD:
-
End-stage renal disease
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- HFmEF:
-
Heart failure with mildly reduced ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- GDMT:
-
Guideline-directed medical therapy
- LVEF:
-
Left ventricular ejection fraction
- NHYA:
-
New York Heart Association
- Hb:
-
Hemoglobin
- Hct:
-
Hematocrit
- SBP:
-
Systolic blood pressure
References
Ferrari R, Balla C, Fucili A (2016) Heart failure: an historical perspective. Eur Heart J Suppl 18(suppl_G):G3-10
2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines | Circulation [Internet]. [cited 2023 Aug 9]. Available from: https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001063
Global burden of heart failure: a comprehensive and updated review of epidemiology - PubMed [Internet]. [cited 2023 Aug 9]. Available from: https://pubmed.ncbi.nlm.nih.gov/35150240/
Kopp W (2019) How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab Syndr Obes Targets Ther 24(12):2221–2236
Elyamani R, Soulaymani A, Hami H (2021) Epidemiology of cardiovascular diseases in Morocco: a systematic review. Rev Diabet Stud RDS 17(2):57–67
Lindstrom M, DeCleene N, Dorsey H et al (2022) Global Burden of Cardiovascular Diseases and Risks Collaboration, 1990–2021. J Am Coll Cardiol 80(25):2372–2425
Naik N, Narula J (2020) Heart failure in low-income and middle-income countries: failing REPORT card grades. Lancet Glob Health 8(3):e318
Agbor VN, Ntusi NAB, Noubiap JJ (2020) An overview of heart failure in low- and middle-income countries. Cardiovasc Diagn Ther 10(2):244–251
Jones NR, Roalfe AK, Adoki I et al (2019) Survival of patients with chronic heart failure in the community: a systematic review and meta-analysis. Eur J Heart Fail 21(11):1306–1325
Dokainish H (2016) Mortality in heart failure patients from Africa, Asia, the middle east and south America (inter-chf). J Am Coll Cardiol 67(134_Supplement):1473–1473
Hung CL, Chao TF, Su CH et al (2021) Income level and outcomes in patients with heart failure with universal health coverage. Heart Br Card Soc 107(3):208–216
AlFaleh HF, Thalib L, Kashour T et al (2016) Sex differences in patients with acute decompensated heart failure: insights from the heart function assessment registry trial in Saudi Arabia. Angiology 67(7):647–656
Taylor CJ, Ordóñez-Mena JM, Jones NR et al (2021) National trends in heart failure mortality in men and women, United Kingdom, 2000–2017. Eur J Heart Fail 23(1):3–12
Ezekowitz JA, Savu A, Welsh RC et al (2020) Is there a sex gap in surviving an acute coronary syndrome or subsequent development of heart failure? Circulation 142(23):2231–2239
Gustafsson F, Torp-Pedersen C, Seibæk M, et al, for the DIAMOND study group (2004) Effect of age on short and long-term mortality in patients admitted to hospital with congestive heart failure. Eur Heart J 25(19):1711–1717
Lin AH, Chin JC, Sicignano NM et al (2017) Repeat hospitalizations predict mortality in patients with heart failure. Mil Med 182(9):e1932–e1937
Blumer V, Mentz RJ, Sun JL et al (2021) Prognostic role of prior heart failure hospitalization among patients hospitalized for worsening chronic heart failure. Circ Heart Fail 14(4):e007871
Younis A, Mulla W, Goldkorn R et al (2019) Differences in mortality of new-onset (De-Novo) acute heart failure versus acute decompensated chronic heart failure. Am J Cardiol 124(4):554–559
López-Vilella R, Pastor PJ, Trenado VD et al (2023) mortality after the first hospital admission for acute heart failure, De Novo versus acutely decompensated heart failure with reduced ejection fraction. Am J Cardiol 1(196):59–66
Ruppar TM, Cooper PS, Mehr DR et al (2016) Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. J Am Heart Assoc 5(6):e002606
Angaran P, Dorian P, Ha ACT, Thavendiranathan P, Tsang W, Leong-Poi H et al (2020) Association of left ventricular ejection fraction with mortality and hospitalizations. J Am Soc Echocardiogr 33(7):802-811.e6
Solomon SD, Anavekar N, Skali H et al (2005) Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation 112(24):3738–3744
Anemia and Heart Failure: A Narrative Review—PMC [Internet]. [cited 2023 Aug 10]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393312/
Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, van der Meer P (2008) Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol 52(10):818–827. https://doi.org/10.1016/j.jacc.2008.04.061
Sharma YP, Kaur N, Kasinadhuni G et al (2021) Anemia in heart failure: still an unsolved enigma. Egypt Heart J 73(1):75
Blood transfusion for acute decompensated heart failure--friend or foe? - PubMed [Internet]. [cited 2023 Aug 10]. Available from: https://pubmed.ncbi.nlm.nih.gov/19781427/
Du Pont-Thibodeau G, Harrington K, Lacroix J (2014) Anemia and red blood cell transfusion in critically ill cardiac patients. Ann Intensive Care 2(4):16
Habibi D, Daneshpour MS, Asgarian S et al (2023) Effect of C-reactive protein on the risk of Heart failure: a mendelian randomization study. BMC Cardiovasc Disord 23(1):112
Matsumoto H, Kasai T, Sato A et al (2019) Association between C-reactive protein levels at hospital admission and long-term mortality in patients with acute decompensated heart failure. Heart Vessels 34(12):1961–1968
Anker SD, von Haehling S (2004) Inflammatory mediators in chronic heart failure: an overview. Heart 90(4):464–470
Testani JM, Brisco-Bacik MA (2017) Worsening renal function and mortality in heart failure. Circ Heart Fail 10(2):e003835
Smith GL, Masoudi FA, Shlipak MG et al (2008) Renal impairment predicts long-term mortality risk after acute myocardial infarction. J Am Soc Nephrol JASN 19(1):141–150
Prastaro M, Nardi E, Paolillo S et al (2022) Cardiorenal syndrome: Pathophysiology as a key to the therapeutic approach in an under-diagnosed disease. J Clin Ultrasound 50(8):1110–1124
Barlera S, Tavazzi L, Franzosi MG et al (2013) Predictors of mortality in 6975 patients with chronic heart failure in the Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico-Heart Failure trial: proposal for a nomogram. Circ Heart Fail 6(1):31–39
Rodriguez M, Hernandez M, Cheungpasitporn W, Kashani KB, Riaz I, Rangaswami J, Herzog E, Guglin M, Krittanawong C (2019) Hyponatremia in heart failure: pathogenesis and management. Curr Cardiol Rev 15(4):252–261. https://doi.org/10.2174/1573403X15666190306111812
Lehrke M, Marx N (2017) Diabetes mellitus and heart failure. Am J Med 130(6S):S40–S50. https://doi.org/10.1016/j.amjmed.2017.04.010
Mamas MA, Sperrin M, Watson MC et al (2017) Do patients have worse outcomes in heart failure than in cancer? A primary care-based cohort study with 10-year follow-up in Scotland. Eur J Heart Fail 19(9):1095–1104
Kim MA (2020) Heart failure awareness in the general population: what should we do next? Korean Circ J 50(7):596–598
Dahrouge S, Kaczorowski J, Dolovich L et al (2018) Long term outcomes of cluster randomized trial to improve cardiovascular health at population level: the Cardiovascular Health Awareness Program (CHAP). PLoS ONE 13(9):e0201802
Karam G, Agarwal A, Sadeghirad B et al (2023) Comparison of seven popular structured dietary programmes and risk of mortality and major cardiovascular events in patients at increased cardiovascular risk: systematic review and network meta-analysis. BMJ 29(380):e072003
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
AC TE conceived and designed the study. AC and SH performed the statistical analyses. AC wrote the first draft of the manuscript. MH and RH performed manuscript revision. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective cohort study conducted at IBN ROCHD hospital, Casablanca, Morocco. was approved by the Hospital Ethical Committee, and informed consent was waived due to the retrospective nature of the study and the use of anonymized patient data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Couissi, A., Haboub, M., Hamady, S. et al. Predictors of mortality in heart failure patients with reduced or mildly reduced Ejection Fraction: The CASABLANCA HF Study. Egypt Heart J 76, 5 (2024). https://doi.org/10.1186/s43044-024-00436-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00436-y