Abstract
Background
The left ventricular assist devices (LVADs) are increasingly used for advanced heart failure as a bridge to heart transplantation or as a destination therapy. The aim of this study was to investigate the changes of diastolic pulmonary gradient (DPG), pulmonary vascular resistance (PVR) and transpulmonary gradient (TPG) after LVAD implantation and their impact on survival after LVAD and heart transplantation.
Results
A total of 73 patients who underwent LVAD (HeartMate III) implantation between 2016 and 2022 were retrospectively studied. According to pre-LVAD catheterization, 49 (67.1%) patients had DPG < 7 mmHg and 24 (32.9%) patients had DPG ≥ 7 mmHg. The patients with a pre-VAD DPG ≥ 7 mmHg had higher frequencies of right ventricular (RV) failure (p < 0.001), RVAD insertion (p < 0.001), need for renal replacement therapy (p = 0.002), total mortality (p = 0.036) and on-VAD mortality (p = 0.04) with a longer ICU stay (p = 0.001) compared to the patients with DPG < 7 mmHg. During the follow-up period of 38 (12–60) months, 24 (32.9%) patients died. Pre-LVAD DPG ≥ 7 mmHg (adjusted HR 1.83, 95% CI 1.21–6.341, p = 0.039) and post-LVAD DPG ≥ 7 mmHg (adjusted HR 3.824, 95% CI 1.482–14.648, p = 0.002) were associated with increased risks of mortality. Neither pre-LVAD TPG ≥ 12 (p = 0.505) nor post-LVAD TPG ≥ 12 mmHg (p = 0.122) was associated with an increased risk of death. Pre-LVAD PVR ≥ 3 WU had a statistically insignificant risk of mortality (HR 2.35, 95% CI 0.803–6.848, p = 0.119) while post-LVAD PVR ≥ 3 WU had an increased risk of death (adjusted HR 2.37, 95% CI 1.241–7.254, p = 0.038). For post-transplantation mortality, post-LVAD DPG ≥ 7 mmHg (p = 0.55), post-LVAD TPG ≥ 12 mmHg (p = 0.85) and PVR ≥ 3 WU (p = 0.54) did not have statistically increased risks. The logistic multivariable regression showed that post-LVAD PVR ≥ 3 WU (p = 0.013), post-LVAD DPG ≥ 7 mmHg (p = 0.026) and RVF (p = 0.018) were the predictors of mortality after LVAD implantation. Pre-LVAD DPG ≥ 7 mmHg (p < 0.001) and pre-LVAD PVR ≥ 3 WU (p = 0.036) were the predictors of RVF after LVAD implantation.
Conclusions
Persistently high DPG was associated with right ventricular failure and mortality after LVAD implantation rather than after heart transplantation. DPG is a better predictor of pulmonary vascular remodeling compared to TPG and PVR. Further larger prospective studies are required in this field due to the growing numbers of patients with advanced heart failure, as possible candidates for LVAD implantation, and limitations of heart transplantation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The development of pulmonary hypertension (PH) in patients with left-sided heart disease (PH-LHD) is associated with a worse impact on survival [1,2,3]. It is a complex process that results from persistently high hydrostatic pressures on pulmonary vascular remodeling. The gradually increased pulmonary capillary wedge pressure (PCWP) initially cause a passive elevation of pulmonary venous and arterial pressures. Long-standing PH can cause pulmonary vascular remodeling with endothelial thickening, and fibrosis of the pulmonary vasculature, resulting in post-capillary PH and elevated pulmonary vascular resistance (PVR) [4].
The diastolic pulmonary gradient (DPG), which is the difference between diastolic pulmonary artery pressure (dPAP) and mean PCWP, has been used to differentiate isolated post-capillary PH (IpcPH) with DPG < 7 mmHg from combined post-capillary and pre-capillary PH (CpcPH) with DPG ≥ 7 mmHg [5]. The DPG has been proposed as a better indicator of pulmonary vascular remodeling compared to the PVR (which is mainly affected by compliance of pulmonary vessels) and the transpulmonary gradient (TPG) which is more affected by left atrial pressure and cardiac output [6,7,8].
Recently, the cutoff levels of the pulmonary hemodynamics and the PVR have been changed according to the 6th World Symposium on Pulmonary Hypertension (WSPH) that released 2022 European Society of Cardiology/European Respiratory Society Guidelines. IpcPH is defined as mPAP > 20 mm Hg, PAWP > 15 mm Hg and PVR ≤ 2WU while CpcPH is defined as mPAP > 20 mm Hg, PAWP > 15 mm Hg and PVR > 2 WU [9].
The left ventricular assist devices (LVADs) are increasingly used for advanced heart failure as a bridge to heart transplantation or as a destination therapy. It has been speculated that LVADs may induce reverse remodeling of the pulmonary vasculature [10,11,12]. However, there are still few data about the pulmonary hemodynamic changes with LVAD implantation and their impact on candidacy to heart transplantation. The objective of this study was to evaluate the pulmonary hemodynamics changes with LVAD implantation and their impact on survival after LVAD and heart transplantation.
Methods
Study design and data collection
This was an observational retrospective cohort study that was approved by the Institutional Review Board of King Faisal Specialist Hospital and was given the reference number (2181248). We enrolled only adult patients ≥ 18 years old who underwent LVAD implantation, between April 2016 and May 2022, with waiving of informed consent due to the retrospective analysis and absence of identifiable data or photographs. All patients recruited had right heart catheterization (RHC) and echocardiography before and after LVAD implantation in our tertiary cardiac center. According to our center policy, the patient selection for LVAD and eligibility for heart transplantation is discussed in the multidisciplinary discussion. For the heart failure patients with reduced ejection fraction (HFrEF) who are dependent on inotropic support or temporary mechanical circulatory support (MCS), durable LVAD is considered as a bridge to transplantation or a destination therapy due to its survival benefit and improvement of quality of life [13, 14]. Heart transplantation is offered to patients with advanced HFrEF despite maximal medical therapy without contraindications due to its survival benefit and improved quality of life [14, 15]. The absolute contraindications included age > 70 years, severe neurological or psychiatric disorders, advanced liver or renal diseases and malignancy. The relative contraindications included significant pulmonary hypertension, reduced pulmonary functions and inability to make a commitment to the transplant team [15]. Data collection was done through the hospital’s electronic records, and there was no loss of follow-up. The demographic, clinical, laboratory, echocardiographic and RHC variables were collected. The primary outcome was all and on-VAD mortality. The secondary outcomes included ICU stay, need for dialysis, right ventricular failure (RVF) and need for right ventricular assist device (RVAD).
Echocardiography and RHC variables
The recruited patients underwent detailed echocardiographic assessments before and after LVAD implantation. In case of multiple assessments, the last echocardiography pre-LVAD and the first detailed one after LVAD were used for analysis. The variables studied included: the left ventricular end diastolic volume (LV-EDV), the left ventricular end systolic volume (LV-ESV), the left ventricular ejection fraction (LV-EF), the left atrium (LA) diameter, the pulmonary artery systolic pressure (PASP) and the presence of valvular lesions.
For invasive pulmonary hemodynamics assessment, RHC was done before and after LVAD implantation. The cardiac output (CO) was measured by the Fick method. The hemodynamic parameters included systolic pulmonary artery pressure (sPAP), diastolic PAP (dPAP), mean PAP (mPAP), PCWP, PVR and systemic vascular resistance (SVR). The DPG was the difference between dPAP and PCWP while the TPG was the difference between mPAP and PCWP. To calculate the PVR in Wood units (WU), the TPG was divided by the CO [5]. According to pre-LVAD catheterization, the patients studied were divided into the DPG < 7 mmHg and the DPG ≥ 7 mmHg groups.
Statistical analysis
Data were checked for normality using Shapiro–Wilk and Kolmogorov–Smirnov tests, skewness, kurtosis and plots, and were proved to be deviated from normal distribution so we used the median with interquartile range (IQR) for quantitative data (Additional file 1). Data were summarized using frequency (with percentage) for categorical data using the Statistical Package for the Social Sciences (SPSS) version 28 (IBM Corp., Armonk, NY, USA). Chi-square (x2) test was used for comparing categorical data. Mann–Whitney test was used for comparing quantitative variables. For comparing serial measurements within each patient, Wilcoxon signed-rank test was used. The Kaplan–Meier method was used to get the survival curves, and the log-rank test was used for comparisons. The Cox proportional hazard analysis was used in the regression models to get the hazards ratios with 95% confidence intervals. Two-sided p-values <0.05 were considered statistically significant.
Results
Demographic and clinical characteristics
We enrolled 73 patients who underwent LVAD (HeartMate III) implantation with a median age of 43.2 (30.9–54) years and a body mass index of 25.6 (22.1–29.3) kg/m2, and 60 (82.2%) of them were males. LVAD implantation was done in 56 (76.7%) patients as a possible bridge to heart transplantation, in 15 (20.5%) patients already listed for transplantation and in 2 (2.7%) patients as a destination therapy. According to pre-LVAD catheterization, 49 (67.1%) patients had a DPG < 7 mmHg, and 24 (32.9%) patients had a DPG ≥ 7 mmHg. The 2 groups had statistically insignificant clinical and laboratory variables before LVAD implantation (Table 1).
Echocardiographic and RHC data
Before LVAD implantation, the patients with the DPG < 7 mmHg had lesser LV-EDV (p = 0.04), LV-ESV (p = 0.047) and PASP (p < 0.001) compared to the patients with DPG ≥ 7 without statistically significant differences regarding other echocardiographic variables. After LVAD implantation, the patients with the DPG < 7 mmHg had lesser EDV (p = 0.002), ESV (p = 0.005), PASP (p < 0.041) and LA diameter (p = 0.04) compared to those with DPG ≥ 7. The DPG ≥ 7 group had higher frequencies of moderate/severe mitral valve regurgitation (p = 0.005) and severe tricuspid regurgitation (p = 0.014) (Table 2).
Before LVAD implantation, the patients with DPG < 7 mmHg had lesser sPAP (p < 0.001), dPAP (p < 0.001), mPAP (p < 0.001), TPG (p < 0.001) and PVR (p < 0.001) compared to the patients with DPG ≥ 7 groups. After LVAD implantation, the patients with DPG < 7 mmHg had lesser sPAP (p < 0.001), dPAP (p = 0.012), mPAP (p = 0.002), TPG (p = 0.01) and PVR (p = 0.019) compared to those with DPG ≥ 7 mmHg (Table 3).
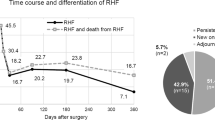
Post-LVAD assessments showed a significant decrease in EDV (p < 0.001), ESV (p < 0.001) and LA diameter (p < 0.001) compared to the pre-LVAD measurements. The LVAD was associated with the decrease in the sPAP (p < 0.001), dPAP (p < 0.001), mPAP (p < 0.001), PCWP (p < 0.001), DPG (p = 0.097), TPG (p < 0.001) and PVR (p < 0.001) (Table 4; Fig. 1).
Outcomes and survival analysis
The patients with a pre-VAD DPG ≥ 7 mmHg had higher frequencies of RVF (p < 0.001), RVAD insertion (p < 0.001), acute kidney injury (p < 0.001), new need for renal replacement therapy (p = 0.002), total mortality (p = 0.036) and on-VAD mortality (p = 0.04) with a longer ICU stay (p = 0.001) compared to the patients with DPG < 7 mmHg (Table 5).
During the follow-up period of 38 (12–60) months, 17 (23.3%) patients had heart transplantation after a median of 10 (6–15) months and 24 (32.9%) patients died. Cox proportional hazard regression revealed that pre-LVAD DPG ≥ 7 mmHg (p = 0.036) and post-LVAD DPG ≥ 7 mmHg (p = 0.005) were associated with increased risks of mortality.
Pre-LVAD TPG ≥ 12 mmHg (p = 0.505) and post-LVAD TPG ≥ 12 mmHg (p = 0.122) did not have significantly increased risks of death. Pre-LVAD PVR ≥ 3 WU had a statistically insignificant risk of mortality (p = 0.119) while post-LVAD PVR ≥ 3 WU had an increased risk of death (HR 2.56, 95% CI 1.117–5.848, p = 0.026) (Table 6).
For post-transplantation mortality, post-LVAD DPG ≥ 7 mmHg (p = 0.55), post-LVAD TPG ≥ 12 mmHg (p = 0.85) and PVR ≥ 3 WU (p = 0.54) did not have statistically increased risks of death in our cohort (Table 6).
The logistic multivariable regression showed that post-LVAD PVR ≥ 3 WU (p = 0.013), post-LVAD DPG ≥ 7 mmHg (p = 0.026) and RVF (p = 0.018) were the predictors of mortality after LVAD. Pre-LVAD DPG ≥ 7 mmHg (p < 0.001) and pre-LVAD PVR ≥ 3 WU (p = 0.036) were the predictors of RVF after LVAD implantation (Table 7).
Survival analyses were graphed by Kaplan–Meier curves with log-rank p values according to pre- and post-LVAD DPG, TPG and PVR (Figs. 2, 3).
Discussion
Our main findings were that the high pre-LVAD DPG was associated with increased occurrence of RV failure and mortality. Persistently high DPG after LVAD carried an increased risk of decreased survival on LVAD, but was not associated with post-transplantation mortality. LVAD insertion was associated with statistically significant improvement of the pulmonary hemodynamic parameters except DPG. Neither pre- nor post-VAD TPG ≥ 12 mmHg was associated with mortality after LVAD or transplantation. Post-LVAD elevated PVR was associated with an increased risk of post-LVAD rather than post-transplantation mortality.
The LVAD implantation for patients with advanced HFrEF produces left ventricular unloading and improves the pulmonary hemodynamic variables resulting in improvement of survival, quality of life, organs perfusion and functional capacity of the patients [16, 17]. In our cohort analysis, the LVAD implantation was associated with decreased left ventricular volumes, decreased severity of mitral regurgitation and improvement of pulmonary hemodynamic variables. Recently, Grupper et al. [18] have studied 85 adult patients with LVAD (HeartMate II and III) and reported the improvement of pulmonary hemodynamics and echocardiographic parameters after LVAD regardless of the pre-LVAD PVR. Despite the LVAD decreases the severity of MR and pulmonary pressures, RVF may occur due to increased preload, loss of the ventricular interdependence and left-sided deviation of septum with possible right ventricular dilatation and worsening of tricuspid regurgitation [19]. RVF occurred in 32.9% of our study patients and almost half of them required the right ventricular assist device (RVAD). The occurrence of RVF and RVAD insertion were more frequent in the group of elevated DPG. Cox proportional and logistic multivariable regressions showed that elevated DPG and PVR were the independent predictors of RVF and mortality after LVAD.
The DPG was proposed as a better indicator of pulmonary vascular remodeling compared to the PVR (which is mainly affected by compliance of pulmonary vessels) and the TPG which is more affected by left atrial pressure and cardiac output [6,7,8]. The cutoff of 7 mmHg was used to differentiate IpcPH with DPG < 7 mmHg from CpcPH with DPG ≥ 7 mmHg [5]. There are still conflicting results about the prognostic value of DPG in the patients with heart failure, post-LVAD insertion and recipients of heart transplantation. Gerges et al. [8] found that elevated DPG > 7 mmHg was associated with a significant pulmonary vascular remodeling and a worse prognosis in patients with TPG > 12 mmHg. Tatsuro Ibe et al. [20] studied 164 patients with PH-LHD and found that the DPG was a more sensitive predictor to worse clinical outcomes compared to the TPG. However, Tampakakis et al. [21] conducted a retrospective analysis of 1236 patients and found that the DPG was not associated with mortality at different cutoff points including 7 mmHg.
Our cohort analysis showed that pre-LVAD high DPG was significantly associated with RVF and mortality. Alnsasra et al. [22] retrospectively reviewed 268 patients with pre-LVAD RHC and found that pre-VAD DPG ≥ 7 mmHg was associated with RVF without a survival difference. Alnsasra et al. [22] did not follow the DPG after LVAD insertion to detect the changes in the pulmonary vascular parameters and any potential impact on survival. In our analysis, the decline of DPG after LVAD insertion was not statistically significant like the decline in TPG and PVR and this may explain the ability of DPG to predict mortality after LVAD. Thenappan et al. [23] investigated the effect of LVAD on DPG in 116 patients and found that 42% of them were non-responders with a persistent DPG > 7 mmHg. Imamura et al. [24] prospectively studied 92 patients with LVAD and found DPG > 5 mmHg was associated with RV deterioration and worse outcomes. We could not find an association between DPG and post-transplantation mortality. Ryan et al. [25] conducted a large retrospective analysis of 5827 recipients of heart transplantation with pulmonary hypertension and concluded that the DPG at different cutoff points was not associated with post-transplantation survival.
We found a statistically significant decrease in the PVR after LVAD insertion and post-LVAD PVR ≥ 3 WU was associated with an increased risk of post-LVAD rather than post-transplantation mortality. LVAD insertion significantly decreased the PVR and TPG compared to medical therapy and increased the candidacy to transplantation but without a survival benefit [26]. LVAD insertion was found to decrease the fixed PH with a high PVR and achieved similar survival rates after heart transplantation compared to those without high PVR [27, 28]. Recently, Selim et al. [29] have retrospectively studied 51 patients with high PVR subjected to LVAD and reported the significant decrease in the PVR after LVAD implantation that persisted after heart transplantation for 1-year follow-up. Tsukashita et al. [30] studied 227 recipients of heart transplantation and found that despite normalization of PVR with LVAD, the patients with an initially high PVR had a greater hospital mortality but a similar 3-year mortality.
According to our study, LVAD significantly decreased the TPG but neither pre- nor post-LVAD was associated with mortality after LVAD or transplantation. Mikus et al. [31] reported that LVAD decreased the TPG and PVR and made 63 patients eligible for transplantation. Alnsasra et al. [22] did not find any association between TPG and RV failure or mortality after LVAD insertion. However, Uriel et al. [32] reported that the elevated TPG rather than PVR negatively affects post-transplantation survival in LVAD patients.
Finally, LVAD implantation improves pulmonary hemodynamics by mechanical unloading. Additionally, Thompson et al. [33] reported the significant decrease in plasma levels of endothlin-1, which is a strong vasoconstrictor after LVAD implantation for patients with advanced heart failure. Saidi et al. [34] retrospectively analyzed 38 patients who receive heart transplantation after LVAD support and reported the improvement of pulmonary hemodynamics with both pulsatile and continuous flow LVADs that were sustained for 3–5 years after transplantation.
Conclusions
Persistently high DPG was associated with right ventricular failure and mortality after LVAD implantation rather than after heart transplantation. DPG is a better predictor of pulmonary vascular remodeling compared to TPG and PVR. Further larger prospective studies are required in this field due to the growing numbers of patients with advanced heart failure, as possible candidates for LVAD implantation, and limitations of heart transplantation.
Limitations of the study
Our study was a single-center work with retrospective analysis of a relatively medium-sized cohort. The results were underpowered due to the sample size. All patients enrolled had continuous flow pump HeartMate III device which limit generalizability to other brands of LVAD.
Availability of data and materials
The data of the study are available with the corresponding author.
Abbreviations
- AKI:
-
Acute kidney injury
- CKD:
-
Chronic kidney disease
- CRRT:
-
Continuous renal replacement therapy
- CpcPH:
-
Combined post-capillary and pre-capillary pulmonary hypertension
- IpcPH:
-
Isolated post-capillary PH
- INTERMACS:
-
Interagency Registry for Mechanically Assisted Circulatory Support
- DPG:
-
Diastolic pulmonary gradient
- HFrEF:
-
Heart failure with reduced ejection fraction
- LVAD:
-
Left ventricular assist device
- LV-EDV:
-
Left ventricular end diastolic volume
- LV-ESV:
-
Left ventricular end systolic volume
- LV-EF:
-
Left ventricular ejection fraction
- LA:
-
Left atrium
- PASP:
-
Pulmonary artery systolic pressure
- sPAP:
-
Systolic pulmonary artery pressure
- dPAP:
-
Diastolic pulmonary artery pressure
- mPAP:
-
Mean pulmonary artery pressure
- RVF:
-
Right ventricular failure
- RVAD:
-
Right ventricular assist device
- PCWP:
-
Pulmonary capillary wedge pressure
- PVR:
-
Pulmonary vascular resistance
- SVR:
-
Systemic vascular resistance
- TPR:
-
Transpulmonary resistance
- TPG:
-
Transpulmonary gradient
- WU:
-
Wood unit
References
Khush KK, Tasissa G, Butler J, McGlothlin D, De Marco T, ESCAPE Investigators (2009) Effect of pulmonary hypertension on clinical outcomes in advanced heart failure: analysis of the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) database. Am Heart J 157:1026–1034
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL (2016) Left ventricular heart failure and pulmonary hypertension. Eur Heart J 37:942–954. https://doi.org/10.1093/eurheartj/ehv512
Kjaergaard J, Akkan D, Iversen KK, Kjoller E, Kober L, Torp-Pedersen C, Hassager C (2007) Prognostic importance of pulmonary hypertension in patients with heart failure. Am J Cardiol 99:1146–1150
Lee F, Mielniczuk LM (2021) Pulmonary hypertension due to left heart disease—a practical approach to diagnosis and management. Can J Cardiol 37(4):572–584. https://doi.org/10.1016/j.cjca.2020.11.003
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M; ESC Scientific Document Group (2016) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37:67–119
Naeije R, Vachiery JL, Yerly P, Vanderpool R (2013) The transpulmonary pressure gradient for the diagnosis of pulmonary vascular disease. Eur Respir J 41:217–223
Vachiery JL, Adir Y, Barbera JA, Champion HC, Coghlan JG, Cottin V, De Marco T, Galie N, Ghio S, Gibbs JS, Martinez FJ, Semigran MJ, Simonneau G, Wells AU, Seeger W (2013) Pulmonary hypertension due to left heart disease. J Am Coll Cardiol 62:D100–D108
Gerges C, Gerges M, Lang MB, Zhang Y, Jakowitsch J, Probst P, Maurer G, Lang IM (2013) Diastolic pulmonary vascular pressure gradient: a predictor of prognosis in “out-of-proportion” pulmonary hypertension. Chest 143:758–766
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS, Escribano-Subias P, Ferrari P, Ferreira DS, Ghofrani HA, Giannakoulas G, Kiely DG, Mayer E, Meszaros G, Nagavci B, Olsson KM, Pepke-Zaba J, Quint JK, Rådegran G, Simonneau G, Sitbon O, Tonia T, Toshner M, Vachiery JL, Vonk Noordegraaf A, Delcroix M, Rosenkranz S, ESC/ERS Scientific Document Group (2022) 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43(38):3618–3731. https://doi.org/10.1093/eurheartj/ehac237. Erratum in: Eur Heart J. 2023;44(15):1312.
Beyersdorf F, Schlensak C, Berchtold-Herz M, Trummer G (2010) Regression of “fixed” pulmonary vascular resistance in heart transplant candidates after unloading with ventricular assist devices. J Thorac Cardiovasc Surg 140:747–749. https://doi.org/10.1016/j.jtcvs.2010.05.042
Mikus E, Stepanenko A, Krabatsch T, Loforte A, Dandel M, Lehmkuhl HB, Hetzer R, Potapov EV (2011) Reversibility of fixed pulmonary hypertension in left ventricular assist device support recipients. Eur J Cardiothorac Surg 40(4):971–977. https://doi.org/10.1016/j.ejcts.2011.01.019
Liden H, Haraldsson A, Ricksten SE, Kjellman U, Wiklund L (2009) Does pretransplant left ventricular assist device therapy improve results after heart transplantation in patients with elevated pulmonary vascular resistance? Eur J Cardiothorac Surg 35(6):1029–1034; discussion 1034–5. https://doi.org/10.1016/j.ejcts.2008.12.024.
Yuzefpolskaya M, Schroeder SE, Houston BA, Robinson MR, Gosev I, Reyentovich A, Koehl D, Cantor R, Jorde UP, Kirklin JK, Pagani FD, D’Alessandro DA (2023) The Society of Thoracic Surgeons Intermacs 2022 annual report: focus on the 2018 Heart Transplant Allocation System. Ann Thorac Surg 115(2):311–327. https://doi.org/10.1016/j.athoracsur.2022.11.023
Al Habeeb W, Tash A, Elasfar A, Almasood A, Bakhsh A, Elshaer F, Al Ayoubi F, AIghalayini KW, AlQaseer MM, Alhussein M, Almogbel O, AlSaif SM, AlHebeshi Y (2023) 2023 National Heart Center/Saudi Heart Association Focused Update of the 2019 Saudi Heart Association Guidelines for the Management of Heart Failure. J Saudi Heart Assoc 35(1):71–134. https://doi.org/10.37616/2212-5043.1334
Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, Mohacsi P, Augustine S, Aaronson K, Barr M (2006) Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates–2006. J Heart Lung Transplant 25(9):1024–1042. https://doi.org/10.1016/j.healun.2006.06.008
Cowger JA, Naka Y, Aaronson KD, Horstmanshof D, Gulati S, Rinde-Hoffman D, Pinney S, Adatya S, Farrar DJ, Jorde UP, MOMENTUM 3 Investigators (2018) Quality of life and functional capacity outcomes in the MOMENTUM 3 trial at 6 months: a call for new metrics for left ventricular assist device patients. J Heart Lung Transplant 37(1):15–24. https://doi.org/10.1016/j.healun.2017.10.019
Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, Long JW, Ascheim DD, Tierney AR, Levitan RG, Watson JT, Meier P, Ronan NS, Shapiro PA, Lazar RM, Miller LW, Gupta L, Frazier OH, Desvigne-Nickens P, Oz MC, Poirier VL, Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) Study Group (2001) Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med 345(20):1435–1443. https://doi.org/10.1056/NEJMoa012175
Grupper A, Mazin I, Faierstein K, Kurnick A, Maor E, Elian D, Barbash IM, Guetta V, Regev E, Morgan A, Segev A, Lavee J, Fefer P (2022) Hemodynamic changes after left ventricular assist device implantation among heart failure patients with and without elevated pulmonary vascular resistance. Front Cardiovasc Med 9:875204. https://doi.org/10.3389/fcvm.2022.875204
Bravo CA, Navarro AG, Dhaliwal KK, Khorsandi M, Keenan JE, Mudigonda P, O’Brien KD, Mahr C (2022) Right heart failure after left ventricular assist device: from mechanisms to treatments. Front Cardiovasc Med 9:1023549. https://doi.org/10.3389/fcvm.2022.1023549
Ibe T, Wada H, Sakakura K, Ikeda N, Yamada Y, Sugawara Y, Mitsuhashi T, Ako J, Fujita H, Momomura SI (2016) Pulmonary hypertension due to left heart disease: the prognostic implications of diastolic pulmonary vascular pressure gradient. J Cardiol 67(6):555–559
Tampakakis E, Leary PJ, Selby VN, De Marco T, Cappola TP, Felker GM, Russell SD, Kasper EK, Tedford RJ (2015) The diastolic pulmonary gradient does not predict survival in patients with pulmonary hypertension due to left heart disease. JACC Heart Fail 3(1):9–16. https://doi.org/10.1016/j.jchf.2014.07.010
Alnsasra H, Asleh R, Schettle SD, Pereira NL, Frantz RP, Edwards BS, Clavell AL, Maltais S, Daly RC, Stulak JM, Rosenbaum AN, Behfar A, Kushwaha SS (2019) Diastolic pulmonary gradient as a predictor of right ventricular failure after left ventricular assist device implantation. J Am Heart Assoc 8(16):e012073. https://doi.org/10.1161/JAHA.119.012073
Thenappan T, Cogswell R, Kamdar F, Holley C, Harvey L, Colvin-Adams M, Eckman P, Adatya S, John R, Liao K, Pritzker MR (2014) Effect of continuous flow left ventricular assist device on diastolic pulmonary artery pressure-to-pulmonary capillary wedge pressure gradient in end stage heart failure patients with pulmonary hypertension. Circulation 130(Suppl_2):A19236
Imamura T, Narang N, Kim G, Raikhelkar J, Chung B, Nguyen A, Holzhauser L, Rodgers D, Kalantari S, Smith B, Ota T, Song T, Juricek C, Burkhoff D, Jeevanandam V, Sayer G, Uriel N (2020) Decoupling between diastolic pulmonary artery and pulmonary capillary wedge pressures is associated with right ventricular dysfunction and hemocompatibility-related adverse events in patients with left ventricular assist devices. J Am Heart Assoc 9(7):e014801. https://doi.org/10.1161/JAHA.119.014801
Tedford RJ, Beaty CA, Mathai SC, Kolb TM, Damico R, Hassoun PM, Leary PJ, Kass DA, Shah AS (2014) Prognostic value of the pre-transplant diastolic pulmonary artery pressure-to-pulmonary capillary wedge pressure gradient in cardiac transplant recipients with pulmonary hypertension. J Heart Lung Transplant 33(3):289–297. https://doi.org/10.1016/j.healun.2013.11.008.Erratum.In:JHeartLungTransplant.2019;38(2):233
Kumarasinghe G, Jain P, Jabbour A, Lai J, Keogh AM, Kotlyar E, Jansz P, Macdonald PS, Hayward CS (2018) Comparison of continuous-flow ventricular assist device therapy with intensive medical therapy in fixed pulmonary hypertension secondary to advanced left heart failure. ESC Heart Fail 5(4):695–702. https://doi.org/10.1002/ehf2.12284
Alba AC, Rao V, Ross HJ, Jensen AS, Sander K, Gustafsson F, Delgado DH (2010) Impact of fixed pulmonary hypertension on post-heart transplant outcomes in bridge-to-transplant patients. J Heart Lung Transplant 29(11):1253–1258. https://doi.org/10.1016/j.healun.2010.06.002
Zimpfer D, Zrunek P, Sandner S, Schima H, Grimm M, Zuckermann A, Wolner E, Wieselthaler G (2007) Post-transplant survival after lowering fixed pulmonary hypertension using left ventricular assist devices. Eur J Cardiothorac Surg 31(4):698–702. https://doi.org/10.1016/j.ejcts.2006.12.036
Selim AM, Wadhwani L, Burdorf A, Raichlin E, Lowes B, Zolty R (2019) Left Ventricular assist devices in pulmonary hypertension group 2 with significantly elevated pulmonary vascular resistance: a bridge to cure. Heart Lung Circ 28(6):946–952. https://doi.org/10.1016/j.hlc.2018.04.299
Tsukashita M, Takayama H, Takeda K, Han J, Colombo PC, Yuzefpolskaya M, Topkara VK, Garan AR, Mancini DM, Kurlansky PA, Naka Y (2015) Effect of pulmonary vascular resistance before left ventricular assist device implantation on short- and long-term post-transplant survival. J Thorac Cardiovasc Surg 150(5):1352–1360, 1361.e1–2. https://doi.org/10.1016/j.jtcvs.2015.07.012
Mikus E, Stepanenko A, Krabatsch T, Dandel M, Lehmkuhl HB, Loforte A, Hetzer R, Potapov EV (2011) Left ventricular assist device or heart transplantation: impact of transpulmonary gradient and pulmonary vascular resistance on decision making. Eur J Cardiothorac Surg 39(3):310–316. https://doi.org/10.1016/j.ejcts.2010.05.031
Uriel N, Imamura T, Sayer G, Agarwal R, Sims DB, Takayama H, John R, Pagani FD, Naka Y, Sundareswaran KS, Farrar DJ, Jorde UP, Heartmate II Clinical Investigators (2019) High transpulmonary artery gradient obtained at the time of left ventricular assist device implantation negatively affects survival after cardiac transplantation. J Card Fail 25(10):777–784. https://doi.org/10.1016/j.cardfail.2019.03.010
Thompson LO, Skrabal CA, Loebe M, Lafuente JA, Roberts RR, Akgul A, Jones V, Bruckner BA, Thohan V, Noon GP, Youker KA (2005) Plasma neurohormone levels correlate with left ventricular functional and morphological improvement in LVAD patients. J Surg Res 123(1):25–32. https://doi.org/10.1016/j.jss.2004.05.013
Saidi A, Selzman CH, Ahmadjee A, Al-Sarie M, Snow GL, Wever-Pinzon O, Alharethi R, Reid B, Stehlik J, Kfoury AG, Bader F (2018) Favorable effects on pulmonary vascular hemodynamics with continuous-flow left ventricular assist devices are sustained 5 years after heart transplantation. ASAIO J 64(1):38–42. https://doi.org/10.1097/MAT.0000000000000614
Acknowledgements
Not applicable.
Funding
The authors did not receive any funds for the study nor publication.
Author information
Authors and Affiliations
Contributions
ML participated in study design, data collection, statistical analysis and manuscript writing. TM participated in data interpretation and manuscript revision. EH and MM participated in data collection and interpretation. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical committee of King Faisal Heart Center, was given a reference number (2181248) and waived from a specific consent as there is no personal identifiable data or photographs.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Normality testing of the data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laimoud, M., Hakami, E., Maghirang, M.J. et al. Impact of diastolic pulmonary gradient and pulmonary vascular remodeling on survival after left ventricular assist device implantation and heart transplantation. Egypt Heart J 75, 102 (2023). https://doi.org/10.1186/s43044-023-00428-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-023-00428-4