Abstract
Background
Stent graft-induced new entry (SINE), defined as the stent graft-induced formation of a new entry point for blood to enter an area, is increasingly being observed after thoracic endovascular aortic repair (TEVAR) for Stanford type B aortic dissection worldwide. We herein describe a case of Stanford type A aortic dissection due to proximal SINE after TEVAR for Stanford type B dissection.
Case presentation
This case involved a 58-year-old man with type A aortic dissection due to SINE. Six years previously, he had developed severe back pain and was diagnosed with type B aortic dissection after computed tomography examination. Because the primary entry was positioned at the descending aorta, we conducted TEVAR for exclusion of the entry with a GORE TAG conformable thoracic aortic graft. He was thereafter followed by our hospital. Six years later, he developed jaw pain and was examined at another hospital. He was transferred to our hospital because of the possibility of type A dissection. Computed tomography revealed type A aortic dissection with proximal site SINE. Emergency partial arch replacement was conducted, and he was discharged on postoperative day 27. Because the entry was at the lesser curve of the arch, we excluded the entry and conducted partial arch replacement.
Conclusions
In this case, proximal SINE occurred 6 years after TEVAR. Because SINE may occur even in the long term after TEVAR, careful follow-up is necessary.
Similar content being viewed by others
Background
Stent graft-induced new entry (SINE), defined as the stent graft-induced formation of a new entry point for blood to enter an area, is being increasingly observed after thoracic endovascular aortic repair (TEVAR) for Stanford type B aortic dissection worldwide. We herein describe a case of Stanford type A dissection due to proximal SINE after TEVAR for Stanford type B dissection. Careful excision of the entry on the lesser curvature side prevented total arch replacement.
Case presentation
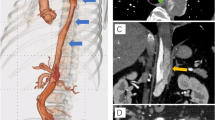
A 58-year-old man presented to our hospital because of chest discomfort and a difference in blood pressure between the right and left arms. He had no family history and did not meet the revised Ghent criteria for Marfan syndrome. The patient had undergone TEVAR with a GORE TAG conformable thoracic aortic graft (CTAG) (diameter 40 mm, length 20 cm and diameter 31 mm, length 20 cm) for Stanford type B dissection at 52 years of age. Noninvasive blood pressure measurement showed that the blood pressure in his right arm was 30 mmHg lower than that in his left arm. We suspected Stanford type A dissection. Enhanced computed tomography showed proximal SINE and therefore type A dissection (Figs. 1A–C, 2A). An emergent operation was performed. The patient was placed in the supine position following induction of general anesthesia. After the right femoral artery and vein were exposed, cardiopulmonary bypass was established via cannulation of these vessels. Median sternotomy was then performed. In our hospital, the routine repair technique for aortic dissection is to perform a median sternotomy after starting femoral bypass. The brachiocephalic and left carotid arteries were exposed during systemic cooling. Hypothermic circulatory arrest was performed at a rectal temperature of 28 °C. Cardioplegic arrest was achieved with intermittent administration of retrograde and antegrade cold blood cardioplegia. After insertion of catheters into the innominate and left common carotid arteries, selective antegrade cerebral perfusion was initiated. The entry tear was found at the lesser aortic arch curve, at which the proximal stent was positioned (Fig. 1D). The entry was excluded, and the transverse arch was transected proximal to the left common carotid artery. After reinforcement of the distal end of the aorta with a felt strip, a four-branched, 28-mm Hemashield prosthesis (Getinge, Gothenburg, Sweden) was anastomosed to the distal end using running 4-0 polypropylene sutures. Systemic perfusion was restarted through the side branch of the graft. The total circulatory arrest time was 66 min. Proximal anastomosis was then performed using continuous 4-0 polypropylene sutures with double-felt-strip reinforcement. With the heart beating, reconstruction of the innominate artery was performed using continuous 5-0 polypropylene sutures. The cardiopulmonary bypass and aortic cross-clamp times were 250 and 139 min, respectively. Postoperative computed tomography showed exclusion of the entry (Fig. 2B). Partial rupture of the tunica media elastic fibers and deposition of mucin were identified, indicating connective tissue disease. Although the patient’s postoperative course was uneventful, weight management and drug adjustment for paroxysmal atrial fibrillation took time; thus, he was discharged on postoperative day 27.
Discussion
SINE is a major complication of TEVAR [1]. New intimal tears after stent graft insertion can be caused by aortic wall fragility or irritation caused by the stent graft [2]. SINE is generally believed to develop in patients with acute or chronic aortic dissection [3]. In the acute phase, because the intimal membrane is thinner and stretches more easily, it can expand and recover its original shape very easily after TEVAR [1]. In the chronic phase, however, the intimal membrane is thicker and more fibrotic than in acute aortic dissection. For this reason, the expansile force of the stent graft persistently injures the rigid true lumen [4]. The intima can then ultimately develop new intimal tears, resulting in aortic dissection.
In this case, SINE had developed in the proximal site 6 years after the first TEVAR. In past reports, SINE had occurred in the acute phase or up to 3 years postoperatively; this is the first report of SINE developing after 6 years postoperatively [5, 6]. Ma et al. [7] reported that a > 15% oversize ratio at the first TEVAR for aortic dissection and a stent graft length of < 145 mm were risk factors for SINE. Our patient did not have these risk factors. Our case is considered rare because Ma et al. [7] reported that a CTAG positioned at Z3 resulted in SINE less frequently than when other TEVAR devices were used.
Hemiarch replacement was considered, and we judged that the margin of the aortic anastomosis in the proximal site from the innominate artery could not be ensured when the entry was removed. We decided to perform partial arch replacement to reconstruct the innominate artery. As a result, we avoided total arch replacement. If we had trimmed the distal anastomosis site at Z3, we might have faced the complicated problem whether we cut the CTAG strad.
Conclusions
In this case, proximal SINE occurred 6 years after TEVAR. Because SINE may occur even in the long run after TEVAR, careful follow-up is necessary.
Availability of data and materials
Not applicable.
Abbreviations
- CTAG:
-
Conformable thoracic aortic graft
- SINE:
-
Stent graft-induced new entry
- TEVAR:
-
Thoracic endovascular aortic repair
References
Jang H, Kim MD, Min Kim G et al (2017) Risk factors for stent graft-induced new entry after thoracic endovascular aortic repair for Stanford type B aortic dissection. J Vasc Surg 65:676–685. https://doi.org/10.1016/j.jvs.2016.09.022
Weng SH, Weng CF, Chen WY et al (2013) Reintervention for distal stent graft-induced new entry after endovascular repair with a stainless steel-based device in aortic dissection. J Vasc Surg 57(1):64–71. https://doi.org/10.1016/J.JVS.2012.07.006
Hughes GC (2019) Stent graft–induced new entry tear (SINE): intentional and NOT. J Thorac Cardiovasc Surg 157(1):101-106.e3. https://doi.org/10.1016/j.jtcvs.2018.10.060
He Y, Tang S, Zhang Y, Liu J, Zhou H (2020) Re-TEVAR in treatment of stent graft-induced new entry between two non-overlapping stent-grafts: a case report. J Cardiothorac Surg. https://doi.org/10.1186/s13019-020-01359-w
Ninomiya M, Takamoto S, Kotsuka Y, Kubota H (2002) Stent-graft-induced intimal injury one year after surgery. J Thorac Cardiovasc Surg 123(2):371–372. https://doi.org/10.1067/mtc.2002.120327
Zhao Y, Yin H, Chen Y et al (2018) Restrictive bare stent prevents distal stent graft-induced new entry in endovascular repair of type B aortic dissection. J Vasc Surg 67(1):93–103. https://doi.org/10.1016/J.JVS.2017.04.066
Ma T, Dong ZH, Fu WG et al (2018) Incidence and risk factors for retrograde type A dissection and stent graft-induced new entry after thoracic endovascular aortic repair. J Vasc Surg 67(4):1026–1033. https://doi.org/10.1016/J.JVS.2017.08.070
Acknowledgements
We thank Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TN wrote this paper. IY helped to write the manuscript. TN performed the operation with IY and NK. KS created volume rendering CT. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
A written informed consent of all details/images relating to the patient for publication was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakajima, T., Iba, Y., Ogura, K. et al. Partial arch replacement of type A aortic dissection after thoracic endovascular aortic repair for type B dissection. Egypt Heart J 75, 81 (2023). https://doi.org/10.1186/s43044-023-00412-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-023-00412-y