Abstract
Background
Despite the improved management of patients with a single ventricle, the long-term outcomes are not optimal. We reported the outcomes of the bidirectional Glenn procedure (BDG) and factors affecting the length of hospital stay, operative mortality, and Nakata index before Fontan completion.
Results
This retrospective study included 259 patients who underwent BDG shunt from 2002 to 2020. The primary study outcomes were operative mortality, duration of hospital stay, and Nakata index before Fontan. Mortality occurred in 10 patients after BDG shunt (3.86%). By univariable logistic regression analysis, postoperative mortality after BDG shunt was associated with high preoperative mean pulmonary artery pressure (OR: 1.06 (95% CI 1.01–1.23); P = 0.02). The median duration of hospital stay after BDG shunt was 12 (9–19) days. Multivariable analysis indicated that Norwood palliation before BDG shunt was significantly associated with prolonged hospital stay (β: 0.53 (95% CI 0.12–0.95), P = 0.01). Fontan completion was performed in 144 patients (50.03%), and the pre-Fontan Nataka index was 173 (130.92–225.34) mm2/m2. Norwood palliation (β: − 0.61 (95% CI 62.63–20.18), P = 0.003) and preoperative saturation (β: − 2.38 (95% CI − 4.49–0.26), P = 0.03) were inversely associated with pre-Fontan Nakata index in patients who had Fontan completion.
Conclusions
BDG had a low mortality rate. Pulmonary artery pressure, Norwood palliation, cardiopulmonary bypass time, and pre-BDG shunt saturation were key factors associated with post-BDG outcomes in our series.
Similar content being viewed by others
Background
Patients with single-ventricle pathology are managed with a series of staged palliative procedures, including modified Blalock-Taussig shunt (MBTS), bidirectional Glenn shunt (BDG), and later Fontan completion [1]. Despite the improved management of patients with a single ventricle, the long-term outcomes are not optimal [2]. BDG shunt is used to unload the systemic ventricle and improve systemic oxygenation in patients with single ventricle physiology [3]; consequently, the outcomes of Fontan completion improved with the staged repair. BDG shunt can be performed as a step before Fontan completion or as part of a one-and-a-half ventricle repair [4, 5].
Several factors could affect mortality and pulmonary artery growth after BDG shunt, including age, diagnosis, and the dominant ventricle [6]. The effect of pulmonary artery growth and the Nakata index on the outcomes of Fontan completion is controversial; however, it was reported to be an independent predictor of the functional status after Fontan [7, 8]. Therefore, we reviewed our experience with patients who underwent BDG shunt and reported the outcomes of this staged palliative procedure and factors affecting the length of hospital stay, operative mortality, and Nakata index before Fontan completion.
Methods
Design and research ethics
We performed a retrospective study on 259 patients who underwent BDG shunt from 2002 to 2020 in our centre. The decision to perform the BDG shunt was based on the multidisciplinary meeting of our paediatrics heart team, including cardiologists, cardiothoracic surgeons, and intensivists.
The study was approved by the local institutional review board, and the need for parents/guardians' consent to participate was waived.
Study data
Data were collected from papers and electronic charts. Preoperative data included age, weight, and height at the time of the procedure, diagnosis, and previous intervention. Echocardiographic data were collected from the most recent echocardiography before the intervention. Data identified from echocardiography included the dominant ventricle and its function and the atrioventricular valve (AVV) regurgitation and its degree (severe, moderate, mild, or absent). The patients who had cardiac catheterization before the BDG shunt were reviewed. Data extracted after reviewing catheterization images included oxygen saturation, mean pulmonary artery (PA) pressure, indexed pulmonary vascular resistance (PVRI), and ventricular end‐diastolic pressure (VEDP). The diameters of the branch pulmonary arteries were measured, and the Nakata index was calculated [6].
BDG shunt was performed on all patients with an end-to-side anastomosis on cardiopulmonary bypass (CPB). In patients with bilateral superior vena cava (SVC), a bilateral BDG shunt was performed. We collected data related to the type of BDG shunt, CPB and cross-clamp times, and concomitant procedures.
Postoperative hospital outcomes included the duration of mechanical ventilation, intensive care unit (ICU) and hospital stay, time of sternal closure, chylothorax, diaphragmatic paralysis, and hospital mortality. Postoperative saturation, the need for inhaled nitric oxide (INO), and sildenafil also were reported.
Patients were followed to Fontan completion, and the interstage mortality, Nakata index before Fontan, and post-Fontan mortality were reported.
Study outcomes were hospital mortality, duration of hospital stay, and Nakata index before Fontan.
Statistical analysis
Descriptive analysis was used to present our data. Continuous data were presented according to the normality distribution using both mean and standard deviation or median and 25th–75th percentiles. Nominal data were presented as numbers and percentages. A comparison of the pre and postoperative oxygen saturation was performed using the paired t-test. Univariable logistic regression analysis was used to evaluate factors associated with hospital mortality. Multivariable negative binomial regression was used to study factors associated with the duration of hospital stay, and quantile regression was used to study factors associated with Nakata index pre-Fontan. Variables with a P-value of 0.15 or less in the univariable analysis were included in the multivariable model. Stata 16 (Stata Corp-College Station-TX-USA) was used for analysis.
Results
Patients' characteristics
The study included 259 patients who underwent BDG shunt. Their median age was 9 months (5.7–15 months), and the most common diagnoses were tricuspid atresia (TA) (n = 49, 18.99%), hypoplastic left heart syndrome (HLHS) (n = 46, 17.83%), and common atrioventricular canal (CAVC) (n = 39, 15.12%). The left ventricle was dominant in 94 patients (36.29%), and the dominant right ventricle was found in 89 patients (34.36%).
BDG shunt was the first stage in 102 patients (39.69%) and was preceded by Norwood in 69 patients (26.85%), patent ductus arteriosus (PDA) stenting in 36 patients (14.01%), and MBTS in 30 patients (11.67%).
Most patients had normal preoperative ventricular function (n = 237, 95.56%). The atrioventricular valve was competent in 102 patients (43.40%), and 6 had severe regurgitation (2.55%). Preoperative saturation was 86% (80–91), and the mean pulmonary artery pressure was 14 (11–18) mmHg. (Table 1).
Operative data
Concomitant pulmonary artery plasty was performed in 67 patients (26.27%), atrial septectomy in 81 patients (31.64%), atrioventricular valve repair in 13 patients (5.06%), and repair of total anomalous pulmonary venous return in 9 patients (3.5%). The median cardiopulmonary bypass time was 55 (40–74) minutes, and the cross-clamp time was 10 (0–31) minutes (Table 2).
Postoperative outcomes
Early postoperative superior vena cava (SVC) pressure was 18 mmHg (15–20). Nitric oxide was used in 29 patients (11.28%), and sildenafil in 54 patients (21.09%). Postoperative oxygen saturation was 89% (85–93), which was significantly higher than the preoperative level (P ˂ 0.001). Sternal closure was delayed in 14 patients (5.45%). Chylothorax occurred in 32 patients (12.65%), phrenic nerve palsy in 26 patients (10.20%), and hospital mortality in 10 (3.86%) patients. The median duration of ICU stay was 5 (3–8) days, and hospital stay was 12 (9–19) days.
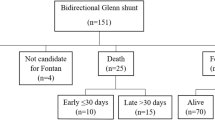
Interstage mortality occurred in 4 (1.54%) patients, and 144 (50.03%) had Fontan completion. Nakata index before Fontan was 173 (130.92–225.34). Mortality after Fontan was reported in 5 (1.93%) patients (Table 3).
Factors associated with BDG shunt outcomes
By univariable logistic regression analysis, postoperative mortality after BDG shunt was associated with high preoperative mean pulmonary artery pressure (P = 0.02) (Table 4).
Multivariable analysis indicated that Norwood palliation before BDG shunt was significantly associated with prolonged hospital stay (P = 0.01) (Table 5).
Norwood palliation and preoperative saturation were inversely associated with the pre-Fontan Nakata index in patients who had Fontan completion (P = 0.003 and 0.03, respectively). (Table 6).
Discussion
The staged approach for single ventricle pathology is associated with improved Fontan outcomes [9, 10]; however, the outcomes of Fontan completion are still not optimal. Improving the outcomes after each stage could impact the overall outcomes after Fontan. In this study, we reported our experience with BDG shunt over twenty years from our tertiary referral centers.
The study included 259 patients who underwent BDG shunt, and the primary outcomes of the study were operative mortality, duration of hospital stay, and the pre-Fontan Nakata index. Secondary outcomes included other postoperative complications, such as delayed sternal closure, chylothorax, diaphragmatic paralysis, Fontan completion, and interstage mortality.
The reported mortality in this series was 3.86%, and it was associated with higher pre-BDG shunt pulmonary artery pressure. The mortality rate reported after BDG shunt varies widely in the literature. Meyer and associates reported a 3.3% mortality rate among 61 children [11], and other series reported a mortality rate between 1 and 20% after BDG shunt [12,13,14,15].
Several factors could contribute to the wide variability of the reported mortality after BDG shunt. One of these factors is the use of cardiopulmonary bypass and the concomitant procedures performed. In our series, all patients had a repair on cardiopulmonary bypass, whether they had associated repair or not. Hussain and colleagues reported no mortality rate in 37 patients who had BDG without cardiopulmonary bypass [16]. Crotti and collaborators evaluated BDG shunt with and without cardiopulmonary bypass and found no difference in the outcomes between both approaches [17].
In our study, cardiopulmonary bypass has an effect on hospital stay but not on mortality. Another factor that could affect the outcomes of staged repair is concomitant atrioventricular valve regurgitation. Sinha and associates found that concomitant atrioventricular valve repair was associated with worse outcomes after the staged repair of single ventricles, but that was not the case in our study [18]. Similar to our series, Sethasathien, and associates found that high preoperative mean pulmonary artery pressure was an independent predictor of mortality after BDG shunt [15]. On the other hand, Silvilairat and colleagues found no effect of pulmonary artery pressure on mortality after BDG shunt [19]. Another study found that patients with accessory pulmonary blood flow had a trend of higher mortality and prolonged hospital stay after BDG shunt [20]. In concomitant to our study Talwar and associates found that younger age at BDG shunt was associated with prolonged hospital stay; however, age and pulmonary artery pressure did not affect mortality [21]. The previous Norwood palliation was another factor associated with a prolonged hospital stay in our series.
The effect of the Nakata index on the outcomes after Fontan is controversial. Adachi and coworkers found that the outcomes after Fontan, including the functional status, were not affected by the pulmonary artery index [22]. However, Ridderbos and colleagues found that the Nakata index was negatively associated with the follow-up duration and correlated with post-Fontan functional status [8]. Kansy and associates found that pre-BDG shunt pulmonary artery diameter was inversely correlated with the growth of the pulmonary artery [23]. Our series found that Norwood palliation and low pre-BDG oxygen saturation negatively correlated with the pre-Fontan Nakata index. Pulmonary artery growth after Norwood palliation is variable and is related to several factors, including the type of conduit [24, 25]. In clinical practice, we are sometimes deceived by high saturation, which could give us false image about pulmonary branch growth [26]. However, from our results here, we highly recommend that saturation alone is not a good indicator. The presence of collaterals to distal pulmonary artery branches could give high saturation and prevent pulmonary trees from growing.
Our study showed that BDG shunt using cardiopulmonary bypass has a low mortality rate. Several factors affecting the outcomes were studied, mainly related to the previous Norwood palliation and pre-BDG shunt pulmonary artery pressure. Patients at high risk of complications could benefit from a personalized approach to improve the outcomes.
Study limitations:
The study is limited by the retrospective design, and several unmeasured variables could have affected the outcomes. Additionally, the study had a wide group of patients, and the outcomes could be variables in those patients. We performed multivariable adjustments to account for these factors, while the number of patients who had mortality was low and multivariable adjustment for this outcome was not feasible. The study was performed over 20 years, and the practice and patient care could have changed during this time.
Conclusions
BDG had a low mortality rate. Pulmonary artery pressure, Norwood palliation, cardiopulmonary bypass time, and pre-BDG shunt saturation were key factors associated with post-BDG outcomes in our series.
Availability of data and materials
Un-identified data are available upon request with the corresponding author.
Abbreviations
- BDG:
-
Bidirectional Glenn procedure
- MBTS:
-
Modified Blalock-Taussig shunt
- AVV:
-
Atrioventricular valve
- PA:
-
Pulmonary artery
- PVRI:
-
Pressure, indexed pulmonary vascular resistance
- VEDP:
-
Ventricular end‐diastolic pressure
- CPB:
-
Cardiopulmonary bypass
- SVC:
-
Superior vena cava
- ICU:
-
Intensive care unit
- INO:
-
Inhaled nitric oxide
- HLHS:
-
Hypoplastic left heart syndrome
- CAVC:
-
Common atrioventricular canal
- PDA:
-
Patent ductus arteriosus
References
Atz AM, Zak V, Mahony L, Uzark K, D’agincourt N, Goldberg DJ et al (2017) Longitudinal outcomes of patients with single ventricle after the fontan procedure. J Am Coll Cardiol 69(22):2735–44
Ismail MF, Elmahrouk AF, Arafat AA, Hamouda TE, Alshaikh BA, Shihata MS et al (2020) Evolution of the Norwood operation outcomes in patients with late presentation. J Thorac Cardiovasc Surg 159(3):1040–1048
Naik RB, Srivastava CP, Arsiwala S, Mathur A, Sharma S (2021) Early outcomes after the on pump bidirectional Glenn procedure: a single center experience. J Card Surg 36(9):3207–3214
Reddy VM, McElhinney DB, Moore P, Haas GS, Hanley FL (1997) Outcomes after bidirectional cavopulmonary shunt in infants less than 6 months old. J Am Coll Cardiol 29(6):1365–1370
Kopf GS, Laks H, Stansel HC, Hellenbrand WE, Kleinman CS, Talner NS (1990) Thirty-year follow-up of superior vena cava-pulmonary artery (Glenn) shunts. J Thorac Cardiovasc Surg 100(5):661–662
Dohain AM, Ismail MF, Elmahrouk AF, Hamouda TE, Arafat AA, Helal A, et al. The outcomes of bidirectional Glenn before and after 4 months of age: A comparative study. J Card Surg. 2020;
Ovroutski S, Alexi-Meskishvili V (2008) Does the Nakata index predict outcome after Fontan operation? Eur J Cardio-Thoracic Surg. 33(5):951
Ridderbos F-JS, Bonenkamp BE, Meyer SL, Eshuis G, Ebels T, van Melle JP, et al. Pulmonary artery size is associated with functional clinical status in the Fontan circulation. Heart 2020; 106(3):233–9
Yamauchi H, Imura H, Maruyama Y, Sakamoto S, Saji Y, Ishii Y et al (2002) Evolution of staged approach for Fontan operation. J Nippon Med Sch 69(2):154–159
Elmahrouk AF, Ismail MF, Arafat AA, Dohain AM, Helal AM, Hamouda TE, Galal M, Edrees AM, Al-Radi OO, Jamjoom AA (2021) Outcomes of biventricular repair for shone’s complex. J Card Surg 36(1):12–20. https://doi.org/10.1111/jocs.15090. (Epub 2020 Oct 8 PMID: 33032391)
Meyer HM, Marange-Chikuni D, Anaesthesia MM, Zühlke L, Roussow B, Human P et al (2022) Outcomes after bidirectional Glenn shunt in a tertiary-care pediatric hospital in South Africa. J Cardiothorac Vasc Anesth. 36(6):1573–81
Samir K, Muftah H, Ammar A (2009) Bidirectional cavopulomnary shunt without cardiopulmonary bypass, the experience of Ain Shams University. J Egypt Soc Cardiothorac Surg. 18:79
Awori MN, Mohamed MNK, Mohamed AA (2019) Utility of the bidirectional Glenn shunt. Ann African Surg. 16(1):30–32
Manuel V, Morais H, Turquetto ALR, Miguel G, Miana LA, Pedro A et al (2019) Single ventricle palliation in a developing Sub-Saharan African country: what should be improved? World J Pediatr Congenit Heart Surg 10(2):164–170
Sethasathien S, Silvilairat S, Lhodamrongrat C, Sittiwangkul R, Makonkawkeyoon K, Pongprot Y et al (2021) Risk factors for morbidity and mortality after a bidirectional Glenn shunt in Northern Thailand. Gen Thorac Cardiovasc Surg 69(3):451–457
Hussain ST, Bhan A, Sapra S, Juneja R, Das S, Sharma S (2007) The bidirectional cavopulmonary (Glenn) shunt without cardiopulmonary bypass: is it a safe option? Interact Cardiovasc Thorac Surg 6(1):77–82
Crotti UA, Braile DM, de Godoy MF, Gonzalez Murillo H, De Marchi CH, Chigutti MY et al (2004) A operação de Glenn bidirecional deve ser realizada com ou sem o auxílio de circulação extracorpórea? Rev Bras Cir Cardiovasc. 19(3):274–9
Sinha R, Altin HF, McCracken C, Well A, Rosenblum J, Kanter K et al (2021) Effect of atrioventricular valve repair on multistage palliation results of single-ventricle defects. Ann Thorac Surg 111(2):662–670
Silvilairat S, Pongprot Y, Sittiwangkul R, Woragidpoonpol S, Chuaratanaphong S, Nawarawong W (2008) Factors influencing survival in patients after bidirectional Glenn shunt. Asian Cardiovasc Thorac Ann 16(5):381–6
Mainwaring RD, Lamberti JJ, Uzark K, Spicer RL, Cocalis MW, Moore JW (1999) Effect of accessory pulmonary blood flow on survival after the bidirectional Glenn procedure. Circulation. 100(suppl_2):II151–II156
Talwar S, Sandup T, Gupta S, Ramakrishnan S, Kothari SS, Saxena A et al (2018) Factors determining early outcomes after the bidirectional superior cavopulmonary anastomosis. Indian J Thorac Cardiovasc Surg 34(4):457–67
Adachi I, Yagihara T, Kagisaki K, Hagino I, Ishizaka T, Kobayashi J et al (2007) Preoperative small pulmonary artery did not affect the midterm results of Fontan operation. Eur J cardio-thoracic Surg Off J Eur Assoc Cardio-thoracic Surg 32(1):156–162
Kansy A, Brzezińska-Rajszys G, Zubrzycka M, Mirkowicz-Małek M, Maruszewski P, Manowska M et al (2013) Pulmonary artery growth in univentricular physiology patients. Kardiol Pol 71(6):581–587
Pruetz JD, Badran S, Dorey F, Starnes VA, Lewis AB (2009) Differential branch pulmonary artery growth after the Norwood procedure with right ventricle-pulmonary artery conduit versus modified Blalock-Taussig shunt in hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 137(6):1342–1348
Ismail MF, Elmahrouk AF, Arafat AA, Hamouda TE, Edrees A, Bogis A, Arfi AM, Dohain AM, Alkhattabi A, Alharbi AW, Shihata MS, Al-Radi OO, Al-Ata JA, Jamjoom AA (2020) Bovine jugular vein valved xenograft for extracardiac total cavo-pulmonary connection: the risk of thrombosis and the potential liver protection effect. J Card Surg 35(4):845–853. https://doi.org/10.1111/jocs.14484. (Epub 2020 Feb 29 PMID: 32112668)
Elmahrouk AF, Ismail MF, Arafat AA, Dohain AM, Edrees AM, Jamjoom AA, Al-Radi OO (2022) Combined Norwood and cavopulmonary shunt as the first palliation in late presenters with hypoplastic left heart syndrome and single-ventricle lesions. J Thorac Cardiovasc Surg. 163(5):1592–1600
Acknowledgements
Not applicable.
Perspectives
Pulmonary artery pressure, Norwood palliation, cardiopulmonary bypass time, and pre-Glenn shunt saturation were the key factors associated with outcome after Bi-directional Glenn.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AAY, AFE, TEH, AMH, and MHM: Conducted the literature search analysis and interpretation of data. OOA, AFE: Conducted the statistical analysis and interpretation of data. AMD, AFE, MSS, OOA, and AAJ: Designed the study, AMA, AMH and MHM: performed data collection, Analysis and interpretation of data, AFE, AAY drafted the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board from King Faisal Specialist Hospital & Research Center-Jeddah (KFSH&RC-J). Reference # (IRB # 2023-03) Date: January 2023. The consent to participate is not applicable due to the retrospective nature of the study.
Consent for publication
Waived for the retrospective nature of the study.
Competing interests
They authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yousef, A.A., Elmahrouk, A.F., Hamouda, T.E. et al. Factors affecting the outcomes after bidirectional Glenn shunt: two decades of experience from a tertiary referral center. Egypt Heart J 75, 53 (2023). https://doi.org/10.1186/s43044-023-00381-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-023-00381-2