Abstract
Background
Angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs) are two of the most commonly used antihypertensive drugs acting on the renin–angiotensin–aldosterone system (RAAS). Previous research has shown that RAAS inhibitors increase the expression of angiotensin-converting enzyme, a cellular receptor for the severe acute respiratory syndrome coronavirus 2, raising concerns that the use of ACEi and ARBs in hypertensive patients may increase COVID-19 patient mortality. Therefore, the main aim of the current study was to find out the role of drugs acting on RAAS, particularly ACEi/ARBs in the deaths of COVID-19 patients.
Results
In total, 68 studies were found to be appropriate, reporting a total of 128,078 subjects. The odds ratio was found to be 1.14 [0.95, 1.36], which indicates the non-significant association of ACEi/ARBs with mortality of COVID-19 patients. Further, the association of individual ACEi/ARBs with mortality of COVID-19 patients was also found non-significant. The sensitivity analysis results have shown no significant effect of outliers on the outcome.
Conclusions
Based on available evidence, ACEi/ARB were not significantly associated with deaths of COVID-19 patients.
Similar content being viewed by others
Key points
-
The role of drugs that are used in the management of hypertension and cardiovascular diseases in the deaths of COVID-19 patients is unclear so far
-
The results of the current analysis have found the non-significant role of these drugs in the deaths of COVID-19 patients
-
Based on current evidence, we suggest to continue the use of drugs particularly ACEi/ARB in the management of hypertension and cardiovascular diseases in COVID-19 patients
Background
Recent, highly contagious novel coronavirus (2019-nCoV) caused by SARS-CoV-2 emerged from Wuhan, China, and rapidly spread over more than 100 countries has caused unprecedented health concerns all over the globe. The first case was recorded in November 2019, and the World Health Organization (WHO) declared a pandemic and a global public health emergency on March 11, 2020 [1]. The virus spread continuously despite many drastic containment measures (complete lockdown, curfews, etc.). On March 13, 2022, more than 456,797,217 cases of COVID-19 were reported across the globe, resulting in approximately 6,043,094 deaths [2]. Health authorities all over the world are struggling to develop possible prevention and therapeutic measures [2, 3]. Fortunately, vaccines are developed and used as a preventive measure across the globe. However, still there is no specific drug available for the treatment of infected patients with SARS-CoV-2. There are a number of research questions that are unanswered so far related to this infection. It has been observed that COVID-19 patients with co-morbid conditions such as diabetes (DM), hypertension (HT), or cardiovascular disease (CVD) are more prone to death [3, 4]. There are a number of explanations for this. It has also been hypothesized that the use of medicines in the management of co-morbid conditions also could be one of the reasons. Hypertension and cardiovascular diseases are the most common co-morbid conditions, and the most commonly used drugs in the management of these conditions are acting on the renin–angiotensin–aldosterone system (RAAS) such as ACEi/ARBs. SARS-CoV-2 enters the cell through the host's angiotensin-converting enzyme (ACE) [4], and drugs acting on the RAAS (ACEi and ARB) may boost ACE2 expression, resulting in greater SARS-CoV-2 binding [5]. The enhanced binding of SARS-CoV-2 to the host could result in severe symptoms or even deaths of COVID-19 patients. The pieces of evidence have been primarily contentious up to this point. Some studies have also shown the protective effect of these medicines in COVID-19 patients [4, 6], whereas some studies have concluded a higher mortality rate [7,8,9,10,11].
To the best of our knowledge, few meta-analyses have also been conducted to find out the association of ACEi/ARBs in the deaths of COVID-19 patients. However, a number of included studies are too less to draw any valid conclusion. Further, some meta-analyses have also included different designs of studies. Therefore, we have performed a systematic review and meta-analysis of observational studies to find out the exact association of ACEi/ARB in the deaths of COVID-19 patients.
Methods
Search strategy
PubMed, Google Scholar, and MedRxiv preprint server were used to identify relevant studies from December 2019 to January 2022 with proper MeSH terms. The MeSH phrases or keywords with Boolean operators were used as followings “(COVID19)” OR “(COVID-19)” OR “(COVID-19 VIRUS INFECTION)” OR “(COVID19 INFECTION)” OR “(SARS COVID 19 INFECTION)” OR “(2019 NOVEL CORONAVIRUS INFECTION)” OR “(SARS COVID DISEASE)” OR “(COVID-19 DISEASE)” AND “(ACE)” OR “(ARB)” OR “(ANGIOTENSIN CONVERTING ENZYME)” OR “(ANGIOTENSIN RECEPTOR BLOCKERS)” which were used are presented in Additional file 1: Table S1. This study was carried out according to the PRISMA [12] and STROBE guidelines [13].
Eligibility criteria
The studies were included or excluded as per the defined inclusion and exclusion criteria. The inclusion criteria include COVID-19 patients, age above 18 years, use of ACEi/ARB classes of drugs alone or in combinations, one of the outcomes was death. The studies were excluded if published other than in the English language, review articles, meta-analyses, case reports, letters, comments or opinions, animal studies, death was not reported as one of the outcomes and editorials.
Screening
The screening of relevant studies as per inclusion and exclusion criteria was done independently by two authors (RS and AK). The PRISMA guideline was followed, and a selection of studies based on titles, abstracts, and full texts was presented in the PRISMA flow chart. The conflict among the authors was resolved after discussion with third (JM), fourth (AKT), and fifth authors (GA).
Quality assessment
The Newcastle–Ottawa (Questionnaire) Scale (NOS) was used to determine the quality of the studies and measuring the risk of bias in cohort and case–control studies [14]. Three reviewers (RS, AK, and JM) have conducted quality assessments of included studies, and disagreements were resolved after discussion with the fourth (AKT) and fifth (GA) authors. The following are the major components used for the quality assessment: comparability, selection of non-exposed cohort, representativeness of the exposed cohort, ascertainment of exposure, outcome assessment, demonstration that the outcome of interest was not present at the start of the study, adequacy of cohort follow-up and follow-up time. The quality rating scale runs from 0 to 10, with a score of > 7 stars indicating high-quality content.
Data extraction
The data were extracted from 68 studies and cross-checked by both authors (RS and AK). The data were extracted in an M.S Excel sheet which contains the columns like authors’ first names, type of study, location of study, total sample size, number of males/females, age groups, the total number of patients in the ACEi/ARBs and Non-ACEi/ARB’s groups, number of subjects died in the ACEi/ARBs and non-ACEi/ARB’s groups.
Data analysis
The overall estimate was calculated in terms of odds ratios with a 95% confidence interval. The random-effect model was preferred over the fixed-effect model due to variations among included studies. The Chi-square statistic and the I2 z test were used to measure heterogeneity. The funnel plot was used to determine whether there was any publishing bias. The sensitivity analysis was performed to check the effects of outliers on the outcome. For the data analysis, RevMan 5 was employed.
Results
Search results and study characteristics
The initial search identified 94,184 studies. A total of 224 duplicates were found and the remaining 93,940 studies were further screened based on the titles. A total of 2907 studies were found relevant which were further screened based on abstracts. Further, a full text of 200 studies was downloaded, and finally, 68 studies were found relevant for quantitative analysis as per the aim and objective of the current study. Out of these 68 studies, 61 studies were published in peer-reviewed journals, whereas the remaining 7 studies were preprints. The step-by-step screening and selection of studies are presented in Fig. 1 as per the PRISMA flow chart. Out of 68 selected studies [7,8,9,10,11, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77], 56 were cohort and the remaining 12 were case–control studies. A total of 128,078 patients were found. The study characteristics of included studies are compiled in Table 1.
Quality evaluation
The Newcastle–Ottawa Scale was used to determine the quality of the studies. The study's cohort and case–control classes were assessed on a scale of 0 to 10, with low risk of bias (8–10), moderate risk (5–7), and high risk (0–4) assigned to each. A total of 52 studies were found to be of excellent quality, and 16 studies were of fair quality as compiled in Table 2. In the case of cohort studies, 49 studies were found to be excellent and 7 were of fair quality, whereas in the case of case–control studies, out of 12 studies, 3 studies were found to be excellent and the remaining 9 were of fair quality.
ACEi/ARB and deaths of COVID-19 patients
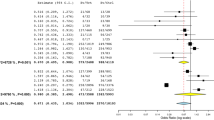
A total of 68 studies were included, with a total of 128,078 COVID-19 cases. A total of 31,625 patients were on ACEi/ARB, whereas the remaining 96,453 were in non-ACEi/ARB group. The pooled odds ratio was found to be 1.14 [0.95, 1.36] which indicates a non-signification association of ACEi/ARB in deaths of COVID-19 patients as compared to the non-ACEi/ARB group (Fig. 2). However, the heterogeneity among studies was found to be 92% which is quite high as indicated by I2 statistics and the Chi-square test (p < 0.00001). Therefore, further, sub-group analysis was also done to find out the reasons for heterogeneity.
Publication bias
The funnel plot was used to analyze publication bias qualitatively. The shape of the plot revealed some degree of asymmetry (Fig. 3) which indicates the involvement of publication bias.
Sub-group analysis
The subgroup analysis was done to check the effect of ACEi/ARB individually on the outcome.
ACEi
Out of 68 studies, only 10 studies mentioned specifically about ACEi and contain relevant data (Additional file 1: Table S2). The pooled odds ratio was found to be 1.43 [0.83, 2.47] which indicates the non-signification association of ACEi in deaths of COVID-19 patients as compared to the non-ACEi group (Fig. 4a).
Further, we have also tried to check the effect of individual ACEi (captopril, enalapril, lisinopril, perindopril, ramipril, and zofenopril) on the outcome, however, we have got relevant information related to ramipril only (Additional file 1: Table S3). The pooled odds ratio was found to be 1.02 [0.44, 2.36] which indicates the non-significant association of ramipril in deaths of COVID-19 patients as compared to the non-ramipril group (Fig. 4b). The funnel plot also indicated the involvement of publication bias as shown in Fig. 5.
ARB
A total of 10 studies mentioned specifically ARB and contain relevant data (Additional file 1: Table S4). The pooled odds ratio was found to be 1.37 [0.68, 2.77] which indicates the non-significant association of ARB in deaths of COVID-19 patients as compared to the non-ARB group (Fig. 6a). However, the heterogeneity among studies was found to be 92% which is quite high as indicated by I2 statistics and the Chi-square test (p < 0.00001).
Further, the effects of individual ARB (candesartan, irbesartan, valsartan, losartan, telmisartan, eprosartan, fimasartan, azilsartan, and olmesartan) on the outcome have also been tried. However, we have found relevant data on losartan (Additional file 1: Table S5) and valsartan only (Additional file 1: Table S6). The pooled odds ratio was found to be 1.20 [0.11, 13.39] and 2.78 [0.45, 17.12] for losartan and valsartan, respectively, which also indicates the non-signification association of losartan and valsartan in the deaths of COVID-19 patients as compared to non-losartan and valsartan group (Fig. 6b, c). The funnel plot indicated involvement of publication bias as shown in Fig. 7.
Sensitivity analysis
The sensitivity analysis was performed to check the effects of outliers on the outcome.
ACEi/ARB
We have identified 4 studies with a high sample size [48, 60, 62, 63] and one study with a low sample size [20]. The analysis was done again after the exclusion of these studies and pooled odds ratios were found to be 1.08 [0.91, 1.29] which also shows non-significant reductions in deaths of COVID-19 patients in the ACEi/ARB group as compared to non-ACEi/ARB group (Fig. 8a).
Sensitivity analysis a forest plot of ACEi/ARB after exclusion of high sample size studies (Rosenthal 2020 [63], Rodilla 2020 [62], Rezel-Potts 2021 [60], Lee 2020 [48]) and low sample size study (Banerjee 2020 [20]). b Forest plot of ACEi after exclusion of high sample size studies (Fosbol 2020, Lee 2020) [8, 48] and low sample size study (Banerjee 2020) [20]. c Forest plot of ramipril after exclusion of high sample sizes (Braude 2020) [23] and low sample size (Banerjee 2020) [20]. d Forest plot of ARBs after exclusion of high sample size (Fosbol 2020, Lee 2020) [8, 48]
ACEi
The analysis was also done after the exclusion of Fosbol and Lee [8, 48] (high sample size) and Banerjee [20] (low sample size) studies. The pooled odds ratio was found to be 0.92 [0.45, 1.88] which also indicates non-significant reductions in deaths of COVID-19 patients in the ACEi group as compared to the non-ACEi group (Fig. 8b). The overall effect of ramipril was also calculated after the exclusion of Braude [23] (high sample size) and Banerjee [20] (low sample size) studies. The overall odds ratio after exclusion was found to be 0.59 [0.30, 1.14] which also indicates a non-significant reduction in deaths of COVID-19 patients in the ramipril group as compared to the non-rampiril group (Fig. 8c).
ARB
The ARB has also shown a non-significant effect after the exclusion of high sample size studies (Fosbol 2020, Lee 2020) [8, 48] (Fig. 8d).
Discussion
It has been observed that COVID-19 patients with co-morbid conditions such as diabetes (DM), hypertension (HT), or cardiovascular disease (CVD) are more prone to death. There is a number of reported explanations in the literature. The use of medicines could also be one of the reasons. ACEi and ARB are commonly used in hypertensive or cardiovascular disease patients. Both groups of medicines work by inhibiting the RAAS. Angiotensin-converting enzyme inhibitors prevent angiotensin-I from converting to angiotensin-II, whereas angiotensin receptor blockers prevent angiotensin II from acting, resulting in vasodilation and decreased aldosterone output. Angiotensin-converting enzyme-2 (ACE2) is found in a variety of organs, including the alveoli of the lungs, and is related to angiotensin-converting enzyme 1 (ACE1), which plays a role in RAAS [21, 55]. The SARS-CoV-2 uses the angiotensin-converting enzyme (ACE) of the host to enter inside the cell, and some of the classes of drugs (ACEI and ARB) could increase ACE2 expression which can result in increased binding of the SARS-CoV-2. The increased binding of SARS-CoV-2 with the host might result in severe conditions for the patients. Ferrario et al. (2005) have reported safety concerns regarding the use of RAAS inhibitors in COVID-19 patients due to increased ACE2 expression [78]. The COVID-19 hypertensive patients using ACEi/ARB have more tendencies to develop severe pneumonia compared to those not using ACEi/ARB [64]. The literature has shown conflicting findings regarding the use of ACEIs and ARB in COVID-19 patients.
To the best of our knowledge, very few meta-analyses have also been conducted to find out the association of ACEi/ARB in the deaths of COVID-19 patients. Recently, the meta-analysis results of Dai et al. (2021) have reported a non-significant association of ACEIs/ARBs in the deaths of COVID-19 patients. However, data included in this analysis was up to June 20, 2020 [79]. The meta-analysis conducted by Singh et al. (2022) has also shown similar results, however, studies were included up to January 18th, 2021 [80]. Hasan et al. (2020) have conducted a meta-analysis of 24 studies and also reported a non-significant association of ACEIs/ARBs in the deaths of COVID-19 patients [81]. The meta-analysis results of Wang et al. (2021) have concluded that ACEi/ARB treatment was significantly associated with a lower risk of mortality in hypertensive COVID-19 patients. The studies were included up to October 12, 2020 [82]. Recently, the meta-analysis conducted by Azad and Kumar (2022) has shown no significant association of ACEi/ARB in the deaths of COVID-19 patients [83]. We have included 68 observational studies, and the results of our meta-analysis have also shown a non-significant association of ACEi/ARBs in the mortality of COVID-19 patients. We have also tried to find out the effect of individual ACEi/ARBs and also found a non-significant association. Further, the sensitivity analysis results have also shown the non-significant impact of outliers on the outcome.
The failure to publish the results of specific studies due to the direction, nature, or strength of the study findings is known as publication bias. Outcome-reporting bias, time-lag bias, gray-literature bias, full-publication bias, language bias, citation bias, and media-attention bias are all examples of publishing bias in academic articles [84, 85]. The funnel plots of the current investigation have indicated the involvement of publication bias.
Heterogeneity refers to the differences in research outcomes between studies. Heterogeneity is not something to be terrified of; it simply implies that your data are variable. When multiple research projects are brought together for a meta-analysis, it is apparent that differences will be discovered [86]. The current analysis results have also shown heterogeneity among included studies as indicated by I2 statistics.
Limitations
We have included seven studies from the medRxiv.org databases that had not yet been peer-reviewed. We saw this as a drawback because peer-reviewers would be able to see more flaws in reporting techniques and other details. The majority of this research, however, was expected to be peer-reviewed. We didn’t find sufficient data to check the effect of all individual ACEi/ARBs on the outcome. The studies published in the English language are only considered. The search is limited to selected databases only. The funnel plots have also indicated the involvement of publication bias.
Conclusions
In conclusion, to date, the use of ACEi and ARB classes of drugs for the management of co-morbid conditions of COVID-19 patients has not been linked with increased deaths. However, more evidence is required.
Availability of data and materials
All data are included in Additional file 1.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitors
- ACE2:
-
Angiotensin-converting enzyme
- ARBs:
-
Angiotensin receptor blockers
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- HT:
-
Hypertension
- MeSH:
-
Medical Subject Headings
- NOS:
-
Newcastle–Ottawa Scale
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- RAAS:
-
Renin–angiotensin–aldosterone system
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- 2019-nCoV:
-
Novel coronavirus
- WHO:
-
World Health Organization
References
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323(13):1239–1242. https://doi.org/10.1001/jama.2020.2648
World Health Organization (WHO) Weekly epidemiological update on COVID-19 - 15 March 2022. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---15-march-2022. Accessed 17 Mar 2022
Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, Hosein Z, Padda I, Mangat J, Altaf M (2020) Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med 2(8):1069–1076. https://doi.org/10.1007/s42399-020-00363-4
Hoffmann M, Kleine-Weber H, Schroeder S et al (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2):271-280.e8. https://doi.org/10.1016/j.cell.2020.02.052
Albini A, Noonan DM, Pelosi G, Di Guardo G, Lombardo M (2020) The SARS-CoV-2 receptor, ACE-2, is expressed on many different cell types: implications for ACE-inhibitor- and angiotensin II receptor blocker-based antihypertensive therapies-reply. Intern Emerg Med 15(8):1583–1584. https://doi.org/10.1007/s11739-020-02436-7
Zhang P, Zhu L, Cai J et al (2020) Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 126(12):1671–1681. https://doi.org/10.1161/CIRCRESAHA.120.317134
Felice C, Nardin C, Di Tanna GL, Grossi U, Bernardi E, Scaldaferri L, Romagnoli M, Tonon L, Cavasin P, Novello S, Scarpa R, Farnia A, De Menis E, Rigoli R, Cinetto F, Pauletto P, Agostini C, Rattazzi M (2020) Use of RAAS inhibitors and risk of clinical deterioration in COVID-19: results from an Italian Cohort of 133 hypertensives. Am J Hypertens 33(10):944–948. https://doi.org/10.1093/ajh/hpaa096
Fosbøl EL, Butt JH, Østergaard L, Andersson C, Selmer C, Kragholm K, Schou M, Phelps M, Gislason GH, Gerds TA, Torp-Pedersen C, Køber L (2020) Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. JAMA 324(2):168–177. https://doi.org/10.1001/jama.2020.11301
Hu J, Zhang X, Zhang X, Zhao H, Lian J, Hao S, Jia H, Yang M, Lu Y, Xiang D, Cai H, Zhang S, Gu J, Ye C, Yu G, Jin C, Zheng L, Yang Y, Sheng J (2020) COVID-19 is more severe in patients with hypertension; ACEI/ARB treatment does not influence clinical severity and outcome. J Infect 81(6):979–997. https://doi.org/10.1016/j.jinf.2020.05.056
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 5(7):811–818. https://doi.org/10.1001/jamacardio.2020.1017
Lafaurie M, Martin-Blondel G, Delobel P, Charpentier S, Sommet A, Moulis G (2021) Outcome of patients hospitalized for COVID-19 and exposure to angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers in France: results of the ACE-CoV study. Fundam Clin Pharmacol 35(1):194–203. https://doi.org/10.1111/fcp.12613
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines. Available at https://www.strobe-statement.org/
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P: The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Derington CG, Cohen JB, Mohanty AF, Greene TH, Cook J, Ying J, Wei G, Herrick JS, Stevens VW, Jones BE, Wang L, Zheutlin AR, South AM, Hanff TC, Smith SM, Cooper-DeHoff RM, King JB, Alexander GC, Berlowitz DR, Ahmad FS, Penrod MJ, Hess R, Conroy MB, Fang JC, Rubin MA, Beddhu S, Cheung AK, Xian W, Weintraub WS, Bress AP (2021) Angiotensin II receptor blocker or angiotensin-converting enzyme inhibitor use and COVID-19-related outcomes among US Veterans. PLoS ONE 16(4):e0248080. https://doi.org/10.1371/journal.pone.0248080
Ayed M, Borahmah AA, Yazdani A, Sultan A, Mossad A, Rawdhan H (2021) Assessment of clinical characteristics and mortality-associated factors in COVID-19 critical cases in Kuwait. Med Princ Pract 30(2):185–192. https://doi.org/10.1159/000513047
Senkal N, Meral R, Medetalibeyoğlu A, Konyaoğlu H, Kose M, Tukek T (2020) Association between chronic ACE inhibitor exposure and decreased odds of severe disease in patients with COVID-19. Anatol J Cardiol 24(1):21–29. https://doi.org/10.14744/AnatolJCardiol.2020.57431
Bae DJ, Tehrani DM, Rabadia SV, Frost M, Parikh RV, Calfon-Press M, Aksoy O, Umar S, Ardehali R, Rabbani A, Bokhoor P, Nsair A, Currier J, Tobis J, Fonarow GC, Dave R, Rafique AM (2020) Angiotensin converting enzyme inhibitor and angiotensin II receptor blocker use among outpatients diagnosed with COVID-19. Am J Cardiol 132:150–157. https://doi.org/10.1016/j.amjcard.2020.07.007
Baker KF, Hanrath AT, van der Loeff IS, Tee SA, Capstick R, Marchitelli G, Li A, Barr A, Eid A, Ahmed S, Bajwa D, Mohammed O, Alderson N, Lendrem C, Lendrem DW, Covid-Control Group, Covid-Clinical Group, Pareja-Cebrian L, Welch A, Field J, Payne BAI, Taha Y, Price DA, Gibbins C, Schmid ML, Hunter E, Duncan CJA (2021) COVID-19 management in a UK NHS foundation trust with a high consequence infectious diseases centre: a retrospective analysis. Med Sci (Basel) 9(1):6. https://doi.org/10.3390/medsci9010006
Banerjee D, Popoola J, Shah S, Ster IC, Quan V, Phanish M (2020) COVID-19 infection in kidney transplant recipients. Kidney Int 97(6):1076–1082. https://doi.org/10.1016/j.kint.2020.03.018
Bauer AZ, Gore R, Sama SR, Rosiello R, Garber L, Sundaresan D, McDonald A, Arruda P, Kriebel D (2021) Hypertension, medications, and risk of severe COVID-19: a Massachusetts community-based observational study. J Clin Hypertens (Greenwich) 23(1):21–27. https://doi.org/10.1111/jch.14101
Bean DM, Kraljevic Z, Searle T, Bendayan R, Kevin O, Pickles A, Folarin A, Roguski L, Noor K, Shek A, Zakeri R, Shah AM, Teo JTH, Dobson RJB (2020) Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are not associated with severe COVID-19 infection in a multi-site UK acute hospital trust. Eur J Heart Fail 22(6):967–974. https://doi.org/10.1002/ejhf.1924
Braude P, Carter B, Short R, Vilches-Moraga A, Verduri A, Pearce L, Price A, Quinn TJ, Stechman M, Collins J, Bruce E, Einarsson A, Rickard F, Mitchell E, Holloway M, Hesford J, Barlow-Pay F, Clini E, Myint PK, Moug S, McCarthy K, Hewitt J (2020) The influence of ACE inhibitors and ARBs on hospital length of stay and survival in people with COVID-19. Int J Cardiol Heart Vasc 31:100660. https://doi.org/10.1016/j.ijcha.2020.100660
Cannata F, Chiarito M, Reimers B, Azzolini E, Ferrante G, My I, Viggiani G, Panico C, Regazzoli D, Ciccarelli M, Voza A, Aghemo A, Li H, Wang Y, Condorelli G, Stefanini GG (2020) Continuation versus discontinuation of ACE inhibitors or angiotensin II receptor blockers in COVID-19: effects on blood pressure control and mortality. Eur Heart J Cardiovasc Pharmacother 6(6):412–414. https://doi.org/10.1093/ehjcvp/pvaa056
Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, Amadou C, Arnault G, Baudoux F, Bauduceau B, Borot S, Bourgeon-Ghittori M, Bourron O, Boutoille D, Cazenave-Roblot F, Chaumeil C, Cosson E, Coudol S, Darmon P, Disse E, Ducet-Boiffard A, Gaborit B, Joubert M, Kerlan V, Laviolle B, Marchand L, Meyer L, Potier L, Prevost G, Riveline JP, Robert R, Saulnier PJ, Sultan A, Thébaut JF, Thivolet C, Tramunt B, Vatier C, Roussel R, Gautier JF, Gourdy P; CORONADO investigators (2020) Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia 63(8):1500–1515. https://doi.org/10.1007/s00125-020-05180-x
Cetinkal G, Kocas BB, Ser OS, Kilci H, Yildiz SS, Ozcan SN, Verdi Y, Altinay M, Kilickesmez K (2020) The association between chronic use of renin–angiotensin–aldosterone system blockers and in-hospital adverse events among COVID-19 patients with hypertension. Sisli Etfal Hastan Tip Bul 54(4):399–404. https://doi.org/10.14744/SEMB.2020.15689
Chaudhri I, Koraishy FM, Bolotova O, Yoo J, Marcos LA, Taub E, Sahib H, Bloom M, Ahmad S, Skopicki H, Mallipattu SK (2020) Outcomes associated with the use of renin–angiotensin–aldosterone system blockade in hospitalized patients with SARS-CoV-2 Infection. Kidney360 1(8):801–809. https://doi.org/10.34067/kid.0003792020
Chen C, Wang F, Chen P, Jiang J, Cui G, Zhou N, Moroni F, Moslehi JJ, Ammirati E, Wang DW (2020) Mortality and pre-hospitalization use of renin-angiotensin system inhibitors in hypertensive COVID-19 patients. J Am Heart Assoc 9(21):e017736. https://doi.org/10.1161/JAHA.120.017736
Chen M, Fan Y, Wu X, Zhang, L, Guo T, Keqiong D, Cao J, Luo H, He T, Gong Y, Wang H, Wan J, Wang X, Lu Z (2020) Clinical characteristics and risk factors for fatal outcome in patients with 2019-coronavirus infected disease (COVID-19) in Wuhan, China (2/27/2020). https://doi.org/10.2139/ssrn.3546069
Chen Y, Yang D, Cheng B, Chen J, Peng A, Yang C, Liu C, Xiong M, Deng A, Zhang Y, Zheng L, Huang K (2020) Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 43(7):1399–1407. https://doi.org/10.2337/dc20-0660
Choi HK, Koo HJ, Seok H, Jeon JH, Choi WS, Kim DJ, Park DW, Han E (2020) ARB/ACEI use and severe COVID-19: a nationwide case–control study. medRxiv 2020.06.12.20129916; https://doi.org/10.1101/2020.06.12.20129916
Christiansen CF, Pottegård A, Heide-Jørgensen U, Bodilsen J, Søgaard OS, Maeng M, Vistisen ST, Schmidt M, Lund LC, Reilev M, Hallas J, Voldstedlund M, Husby A, Thomsen MK, Johansen NB, Brun NC, Thomsen RW, Bøtker HE, Sørensen HT (2021) SARS-CoV-2 infection and adverse outcomes in users of ACE inhibitors and angiotensin-receptor blockers: a nationwide case–control and cohort analysis. Thorax 76(4):370–379. https://doi.org/10.1136/thoraxjnl-2020-215768
Conversano A, Melillo F, Napolano A, Fominskiy E, Spessot M, Ciceri F, Agricola E (2020) Renin–angiotensin–aldosterone system inhibitors and outcome in patients with SARS-CoV-2 pneumonia: a case series study. Hypertension 76(2):e10–e12. https://doi.org/10.1161/HYPERTENSIONAHA.120.15312
Covino M, De Matteis G, Burzo ML, Santoro M, Fuorlo M, Sabia L, Sandroni C, Gasbarrini A, Franceschi F, Gambassi G; Gemelli Against COVID-19 Group (2020) Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and prognosis of hypertensive patients hospitalised with COVID-19. Intern Med J 50(12):1483–1491. https://doi.org/10.1111/imj.15078
Desai A, Voza G, Paiardi S, Teofilo FI, Caltagirone G, Pons MR, Aloise M, Kogan M, Tommasini T, Savevski V, Stefanini G, Angelini C, Ciccarelli M, Badalamenti S, De Nalda AL, Aghemo A, Cecconi M, Martinelli Boneschi F, Voza A; Humanitas COVID-19 task force (2021) The role of anti-hypertensive treatment, comorbidities and early introduction of LMWH in the setting of COVID-19: a retrospective, observational study in Northern Italy. Int J Cardiol 324:249–254. https://doi.org/10.1016/j.ijcard.2020.09.062
Genet B, Vidal JS, Cohen A, Boully C, Beunardeau M, Marine Harlé L, Gonçalves A, Boudali Y, Hernandorena I, Bailly H, Lenoir H, Piccoli M, Chahwakilian A, Kermanach L, de Jong L, Duron E, Girerd X, Hanon O (2020) COVID-19 In-hospital mortality and use of renin–angiotensin system blockers in geriatrics patients. J Am Med Dir Assoc 21(11):1539–1545. https://doi.org/10.1016/j.jamda.2020.09.004
Giacomelli A, Ridolfo AL, Milazzo L, Oreni L, Bernacchia D, Siano M, Bonazzetti C, Covizzi A, Schiuma M, Passerini M, Piscaglia M, Coen M, Gubertini G, Rizzardini G, Cogliati C, Brambilla AM, Colombo R, Castelli A, Rech R, Riva A, Torre A, Meroni L, Rusconi S, Antinori S, Galli M (2020) 30-Day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res 158:104931. https://doi.org/10.1016/j.phrs.2020.104931
Giorgi Rossi P, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R; Reggio Emilia COVID-19 Working Group (2020) Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLoS ONE 15(8):e0238281. https://doi.org/10.1371/journal.pone.0238281
Hakeam HA, Alsemari M, Duhailib ZA, Ghonem L, Alharbi SA, Almutairy E, Sheraim NMB, Alsalhi M, Alhijji A, AlQahtani S, Khalid M, Barry M (2021) Association of angiotensin-converting enzyme inhibitors and angiotensin II blockers with severity of COVID-19: a multicentre, prospective study. J Cardiovasc Pharmacol Ther 26(3):244–252. https://doi.org/10.1177/1074248420976279
Huang Z, Cao J, Yao Y, Jin X, Luo Z, Xue Y, Zhu C, Song Y, Wang Y, Zou Y, Qian J, Yu K, Gong H, Ge J (2020) The effect of RAS blockers on the clinical characteristics of COVID-19 patients with hypertension. Ann Transl Med 8(7):430. https://doi.org/10.21037/atm.2020.03.229
Ip A, Parikh K, Parrillo JE, Mathura S, Hansen E, Sawczuk IS, Goldberg SL (2020) Hypertension and renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. medRxiv 2020.04.24.20077388. https://doi.org/10.1101/2020.04.24.20077388
Jung C, Bruno RR, Wernly B, Joannidis M, Oeyen S, Zafeiridis T, Marsh B, Andersen FH, Moreno R, Fernandes AM, Artigas A, Pinto BB, Schefold J, Wolff G, Kelm M, De Lange DW, Guidet B, Flaatten H, Fjølner J; COVIP study group (2021) Inhibitors of the renin–angiotensin–aldosterone system and COVID-19 in critically ill elderly patients. Eur Heart J Cardiovasc Pharmacother 7(1):76–77. https://doi.org/10.1093/ehjcvp/pvaa083
Jung SY, Choi JC, You SH, Kim WY (2020) Association of renin-angiotensin-aldosterone system inhibitors with coronavirus disease 2019 (COVID-19)-related outcomes in Korea: a nationwide population-based cohort study. Clin Infect Dis 71(16):2121–2128. https://doi.org/10.1093/cid/ciaa624
Khan KS, Reed-Embleton H, Lewis J, Bain P, Mahmud S (2020) Angiotensin converting enzyme inhibitors do not increase the risk of poor outcomes in COVID-19 disease. A multi-centre observational study. Scott Med J 65(4):149–153. https://doi.org/10.1177/0036933020951926
Khera R, Clark C, Lu Y, Guo Y, Ren S, Truax B, Spatz ES, Murugiah K, Lin Z, Omer SB, Vojta D, Krumholz HM (2020) Association of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers with the risk of hospitalization and death in hypertensive patients with coronavirus disease-19. medRxiv. 19:2020.05.17.20104943. https://doi.org/10.1101/2020.05.17.20104943
Kim JH, Baek YH, Lee H, Choe YJ, Shin HJ, Shin JY (2021) Clinical outcomes of COVID-19 following the use of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers among patients with hypertension in Korea: a nationwide study. Epidemiol Health 43:e2021004. https://doi.org/10.4178/epih.e2021004
Lam KW, Chow KW, Vo J, Hou W, Li H, Richman PS, Mallipattu SK, Skopicki HA, Singer AJ, Duong TQ (2020) Continued in-hospital angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker use in hypertensive COVID-19 patients is associated with positive clinical outcome. J Infect Dis 222(8):1256–1264. https://doi.org/10.1093/infdis/jiaa447
Lee HY, Ahn J, Kang CK, Won SH, Park JH, Kang CH, Chung KH, Joh JS, Bang J, Yoo, H, Park O, Oh M (2020) Association of angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors on COVID-19-related outcome (4/1/2020). https://doi.org/10.2139/ssrn.3569837
Li J, Wang X, Chen J, Zhang H, Deng A (2020) Association of renin-angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan. China JAMA Cardiol 5(7):825–830. https://doi.org/10.1001/jamacardio.2020.1624
Liabeuf S, Moragny J, Bennis Y, Batteux B, Brochot E, Schmit JL, Lanoix JP, Andrejak C, Ganry O, Slama M, Maizel J, Mahjoub Y, Masmoudi K, Gras-Champel V (2021) Association between renin–angiotensin system inhibitors and COVID-19 complications. Eur Heart J Cardiovasc Pharmacother 7(5):426–434. https://doi.org/10.1093/ehjcvp/pvaa062
Lim JH, Cho JH, Jeon Y, Kim JH, Lee GY, Jeon S, Noh HW, Lee YH, Lee J, Chang HH, Jung HY, Choi JY, Park SH, Kim CD, Kim YL, Kim SW (2020) Adverse impact of renin-angiotensin system blockade on the clinical course in hospitalized patients with severe COVID-19: a retrospective cohort study. Sci Rep 10(1):20250. https://doi.org/10.1038/s41598-020-76915-4
López-Otero D, López-Pais J, Cacho-Antonio CE, Antúnez-Muiños PJ, González-Ferrero T, Pérez-Poza M, Otero-García Ó, Díaz-Fernández B, Bastos-Fernández M, Bouzas-Cruz N, Sanmartín-Pena XC, Varela-Román A, Portela-Romero M, Valdés-Cuadrado L, Pose-Reino A, González-Juanatey JR (2021) Impacto de los inhibidores de la enzima de conversión de la angiotensina y los antagonistas del receptor de la angiotensina II en la COVID-19 en una población occidental. Registro CARDIOVID [Impact of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers on COVID-19 in a western population. CARDIOVID registry]. Rev Esp Cardiol 74(2):175–182. https://doi.org/10.1016/j.recesp.2020.05.030
Matsuzawa Y, Ogawa H, Kimura K, Konishi M, Kirigaya J, Fukui K, Tsukahara K, Shimizu H, Iwabuchi K, Yamada Y, Saka K, Takeuchi I, Hirano T, Tamura K (2020) Renin-angiotensin system inhibitors and the severity of coronavirus disease 2019 in Kanagawa, Japan: a retrospective cohort study. Hypertens Res 43(11):1257–1266. https://doi.org/10.1038/s41440-020-00535-8
Mehta N, Kalra A, Nowacki AS, Anjewierden S, Han Z, Bhat P, Carmona-Rubio AE, Jacob M, Procop GW, Harrington S, Milinovich A, Svensson LG, Jehi L, Young JB, Chung MK (2020) Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol 5(9):1020–1026. https://doi.org/10.1001/jamacardio.2020.1855
Meng J, Xiao G, Zhang J, He X, Ou M, Bi J, Yang R, Di W, Wang Z, Li Z, Gao H, Liu L, Zhang G (2020) Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect 9(1):757–760. https://doi.org/10.1080/22221751.2020.1746200
Negreira-Caamaño M, Piqueras-Flores J, Martínez-DelRio J, Nieto-Sandoval-Martin-DeLaSierra P, Aguila-Gordo D, Mateo-Gomez C, Salas-Bravo D, Rodriguez-Martinez M, Negreira-Caamaño M (2020) Impact of treatment with renin-angiotensin system inhibitors on clinical outcomes in hypertensive patients hospitalized with COVID-19. High Blood Press Cardiovasc Prev 27(6):561–568. https://doi.org/10.1007/s40292-020-00409-7
Oussalah A, Gleye S, Clerc Urmes I, Laugel E, Callet J, Barbé F, Orlowski S, Malaplate C, Aimone-Gastin I, Caillierez BM, Merten M, Jeannesson E, Kormann R, Olivier JL, Rodriguez-Guéant RM, Namour F, Bevilacqua S, Losser MR, Levy B, Kimmoun A, Gibot S, Thilly N, Frimat L, Schvoerer E, Guéant JL (2020) Long-term ACE inhibitor/ARB use is associated with severe renal dysfunction and acute kidney injury in patients with severe COVID-19: results from a referral center cohort in the Northeast of France. Clin Infect Dis 71(9):2447–2456. https://doi.org/10.1093/cid/ciaa677
Pan W, Zhang J, Wang M, Ye J, Xu Y, Shen B, He H, Wang Z, Ye D, Zhao M, Luo Z, Liu M, Zhang P, Gu J, Liu M, Li D, Liu J, Wan J (2020) Clinical features of COVID-19 in patients with essential hypertension and the impacts of renin-angiotensin-aldosterone system inhibitors on the prognosis of COVID-19 patients. Hypertension 76(3):732–741. https://doi.org/10.1161/HYPERTENSIONAHA.120.15289
Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT, Skanderson M, Hauser RG, Schultze A, Jarvis CI, Holodniy M, Lo Re V, Akgun KM, Crothers K, Taddei TH, Freiberg MS, Justice AC (2020) Covid-19 testing, hospital admission, and intensive care among 2,026,227 United States veterans aged 54–75 years. medRxiv. 14:2020.04.09.20059964. https://doi.org/10.1101/2020.04.09.20059964
Rezel-Potts E, Douiri A, Chowienczyk PJ, Gulliford MC (2021) Antihypertensive medications and COVID-19 diagnosis and mortality: population-based case-control analysis in the United Kingdom. Br J Clin Pharmacol 87(12):4598–4607. https://doi.org/10.1111/bcp.14873
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; the Northwell COVID-19 Research Consortium, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP (2020) Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 323(20):2052–2059. https://doi.org/10.1001/jama.2020.6775
Rodilla E, Saura A, Jiménez I, Mendizábal A, Pineda-Cantero A, Lorenzo-Hernández E, Fidalgo-Montero MDP, López-Cuervo JF, Gil-Sánchez R, Rabadán-Pejenaute E, Abella-Vázquez L, Giner-Galvañ V, Solís-Marquínez MN, Boixeda R, Peña-Fernández A, Carrasco-Sánchez FJ, González-Moraleja J, Torres-Peña JD, Guisado-Espartero ME, Escobar-Sevilla J, Guzmán-García M, Martín-Escalante MD, Martínez-González ÁL, Casas-Rojo JM, Gómez-Huelgas R (2020) Association of hypertension with all-cause mortality among hospitalized patients with COVID-19. J Clin Med 9(10):3136. https://doi.org/10.3390/jcm9103136
Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S (2020) Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open 3(12):e2029058. https://doi.org/10.1001/jamanetworkopen.2020.29058
Sardu C, Maggi P, Messina V, Iuliano P, Sardu A, Iovinella V, Paolisso G, Marfella R (2020) Could anti-hypertensive drug therapy affect the clinical prognosis of hypertensive patients with COVID-19 infection? Data from centers of Southern Italy. J Am Heart Assoc 9(17):e016948. https://doi.org/10.1161/JAHA.120.016948
Selçuk M, Çınar T, Keskin M, Çiçek V, Kılıç Ş, Kenan B, Doğan S, Asal S, Günay N, Yıldırım E, Keskin Ü, Orhan AL (2020) Is the use of ACE inb/ARBs associated with higher in-hospital mortality in Covid-19 pneumonia patients? Clin Exp Hypertens 42(8):738–742. https://doi.org/10.1080/10641963.2020.1783549
Shah P, Owens J, Franklin J, Jani Y, Kumar A, Doshi R (2020) Baseline use of angiotensin-converting enzyme inhibitor/AT1 blocker and outcomes in hospitalized coronavirus disease 2019 African-American patients. J Hypertens 38(12):2537–2541. https://doi.org/10.1097/HJH.0000000000002584
Soleimani A, Kazemian S, Karbalai Saleh S, Aminorroaya A, Shajari Z, Hadadi A, Talebpour M, Sadeghian H, Payandemehr P, Sotoodehnia M, Bahreini M, Najmeddin F, Heidarzadeh A, Zivari E, Ashraf H (2020) Effects of angiotensin receptor blockers (ARBs) on in-hospital outcomes of patients with hypertension and confirmed or clinically suspected COVID-19. Am J Hypertens 33(12):1102–1111. https://doi.org/10.1093/ajh/hpaa149
Son M, Seo J, Yang S (2020) Association between renin-angiotensin-aldosterone system inhibitors and COVID-19 infection in South Korea. Hypertension 76(3):742–749. https://doi.org/10.1161/HYPERTENSIONAHA.120.15464
Tan ND, Qiu Y, Xing XB, Ghosh S, Chen MH, Mao R (2020) Associations between angiotensin-converting enzyme inhibitors and angiotensin II receptor blocker use, gastrointestinal symptoms, and mortality among patients with COVID-19. Gastroenterology 159(3):1170-1172.e1. https://doi.org/10.1053/j.gastro.2020.05.034
Wang Z, Zhang D, Wang S, Jin Y, Huan J, Wu Y, Xia C, Li Z, Qi X, Zhang D, Han X, Zhu X, Qu Y, Wang Q (2020) A retrospective study from 2 centers in china on the effects of continued use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers in patients with hypertension and COVID-19. Med Sci Monit 26:e926651. https://doi.org/10.12659/MSM.926651
Xu J, Huang C, Fan G, Liu Z, Shang L, Zhou F, Wang Y, Yu J, Yang L, Xie K, Huang Z, Huang L, Gu X, Li H, Zhang Y, Wang Y, Hayden FG, Horby PW, Cao B, Wang C (2020) Use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers in context of COVID-19 outbreak: a retrospective analysis. Front Med 14(5):601–612. https://doi.org/10.1007/s11684-020-0800-y
Yang G, Tan Z, Zhou L, Yang M, Peng L, Liu J, Cai J, Yang R, Han J, Huang Y, He S (2020) Effects of angiotensin II receptor blockers and ACE (angiotensin-converting enzyme) inhibitors on virus infection, inflammatory status, and clinical outcomes in patients with COVID-19 and hypertension: a single-center retrospective study. Hypertension 76(1):51–58. https://doi.org/10.1161/HYPERTENSIONAHA.120.15143
Yuan Y, Liu D, Zeng S, Wang S, Xu S, Wang Y, Yu R, Gao Y, Li H, Feng X, Zhou N, Zhao C, Gao Q (2020) In-hospital use of ACEI/ARB is associated with lower risk of mortality and critic illness in COVID-19 patients with hypertension. J Infect 81(5):816–846. https://doi.org/10.1016/j.jinf.2020.08.014
Zeng Z, Sha T, Zhang Y, Wu F, Hu H, Li H (2020) Hypertension in patients hospitalized with COVID-19 in Wuhan, China: a single-center retrospective observational study. MedRxiv. https://doi.org/10.1101/2020.04.06.20054825
Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, Liu YM, Zhao YC, Huang X, Lin L, Xia M, Chen MM, Cheng X, Zhang X, Guo D, Peng Y, Ji YX, Chen J, She ZG, Wang Y, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang XJ, Wang X, Touyz RM, Xia J, Zhang BH, Huang X, Yuan Y, Loomba R, Liu PP, Li H (2020) Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 126(12):1671–1681. https://doi.org/10.1161/CIRCRESAHA.120.317134
Zhong Y, Zhao L, Wu G, Hu C, Wu C, Xu M, Dong H, Zhang Q, Wang G, Yu B, Lv J, Wu C, Zhang S, Cao C, Shu L, Pan Y, Liu X, Wu F (2020) Impact of renin-angiotensin system inhibitors use on mortality in severe COVID-19 patients with hypertension: a retrospective observational study. J Int Med Res 48(12):300060520979151. https://doi.org/10.1177/0300060520979151
Zhou F, Liu YM, Xie J, Li H, Lei F, Yang H, Qin JJ, Cai J, Zhang XJ, Wu B, Xia M, Xiang D, Yang C, Ma X, Xu Q, Lu Z, Lu H, Xia X, Wang D, Liao X, Peng G, Yang J, Huang X, Zhang BH, Yuan Y, Wei X, Liu PP, Wang Y, Zhang P, She ZG, Xia J, Li H (2020) Comparative impacts of ACE (angiotensin-converting enzyme) inhibitors versus angiotensin II receptor blockers on the risk of COVID-19 mortality. Hypertension 76(2):e15–e17. https://doi.org/10.1161/HYPERTENSIONAHA.120.15622
Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE (2005) Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 111(20):2605–2610. https://doi.org/10.1161/CIRCULATIONAHA.104.510461
Dai XC, An ZY, Wang ZY, Wang ZZ, Wang YR. (2021) Associations Between the Use of Renin-Angiotensin System Inhibitors and the Risks of Severe COVID-19 and Mortality in COVID-19 Patients With Hypertension: A Meta-Analysis of Observational Studies. Front Cardiovasc Med 8:609857. https://doi.org/10.3389/fcvm.2021.609857
Singh R, Rathore SS, Khan H, Bhurwal A, Sheraton M, Ghosh P, Anand S, Makadia J, Ayesha F, Mahapure KS, Mehra I, Tekin A, Kashyap R, Bansal V (2022) Mortality and severity in COVID-19 patients on ACEIs and ARBs—a systematic review, meta-analysis, and meta-regression analysis. Front Med (Lausanne) 10(8):703661. https://doi.org/10.3389/fmed.2021.703661
Hasan SS, Kow CS, Hadi MA, Zaidi STR, Merchant HA (2020) Mortality and disease severity among COVID-19 patients receiving renin–angiotensin system inhibitors: a systematic review and meta-analysis. Am J Cardiovasc Drugs 20(6):571–590. https://doi.org/10.1007/s40256-020-00439-5
Wang Y, Chen B, Li Y, Zhang L, Wang Y, Yang S, Xiao X, Qin Q (2021) The use of renin–angiotensin–aldosterone system (RAAS) inhibitors is associated with a lower risk of mortality in hypertensive COVID-19 patients: a systematic review and meta-analysis. J Med Virol 93(3):1370–1377. https://doi.org/10.1002/jmv.26625
Azad GN, Kumar A (2022) ACEi/ARB and deaths of COVID-19 patients. Curr Hypertens Rev. https://doi.org/10.2174/1573402118666220407093332
Srivastava R, Kumar A (2021) Use of aspirin in reduction of mortality of COVID-19 patients: a meta-analysis. Int J Clin Pract 75:e14515. https://doi.org/10.1111/ijcp.14515
Vitalakumar D, Sharma A, Kumar A, Flora SJS (2021) Neurological Manifestations in COVID-19 Patients: a meta-analysis. ACS Chem Neurosci 12:2776–2797. https://doi.org/10.1021/acschemneuro.1c00353
Thakur M, Datusalia AK, Kumar A (2022) Use of steroids in COVID-19 patients: a meta-analysis. Eur J Pharmacol 914:174579. https://doi.org/10.1016/j.ejphar.2021.174579
Acknowledgements
The authors acknowledge the Vice-Chancellor Prof. (Dr.) Ramesh K. Goyal, Delhi Pharmaceutical Sciences and Research University, New Delhi, India, for providing an excellent research facility. The authors also acknowledge the Delhi knowledge Development Foundation for providing funding for the establishment of DPSRU, the Centre for Precision Medicine and Pharmacy.
Funding
We have not received any funding for this particular work.
Author information
Authors and Affiliations
Contributions
RS, and AK contributed to the study conception and design. The data collection was done by RS, cross-checked by JM, and analyzed by AK. GA, JM, and AKT give their valuable suggestions throughout the study and contributed to revision. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Table S1:
Search Strategy. Table S2: Details of the ACEi therapy (Molecules type). Table S3: Details of the ACEi therapy (Molecules type ramipril). Table S4 Details of the ARB therapy (Molecules type). Table S5: Details of the ARB therapy (Molecules type losartan). Table S6 Details of the ARB therapy (Molecules type valsartan).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharma, R., Kumar, A., Majeed, J. et al. Drugs acting on the renin–angiotensin–aldosterone system (RAAS) and deaths of COVID-19 patients: a systematic review and meta-analysis of observational studies. Egypt Heart J 74, 64 (2022). https://doi.org/10.1186/s43044-022-00303-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-022-00303-8