Abstract
Background
Cardiac metastases are rare and frequently remain undiagnosed due to the absence of clinical signs in the majority of cases. Malignancies found to most commonly metastasise to the heart include lung carcinoma, breast carcinoma and lymphoma, while urothelial carcinoma is a rare cause of cardiac metastasis. The patient presented with pyrexia, a rare presentation of metastatic cardiac involvement. Single metastatic lesions are mainly reported in the literature, while multiple metastatic deposits such as in this case are less common.
Case presentation
A 74-year-old gentleman presented with frequent febrile spikes, a month after undergoing a nephroureterectomy for poorly differentiated urothelial carcinoma. No febrile source was identified, and a computed tomography identified two cardiac lesions. A transthoracic echocardiogram could not detect the cardiac lesions; therefore, cardiac magnetic resonance (CMR) imaging was performed. Three spherical intramyocardial masses were noted at the basal septum, LV apex and the anteromedial papillary muscle. The lesions demonstrated signal characteristics suggestive of cardiac metastases (high fluid content, absence of fat, presence of a surrounding rim of increased extravascular space, absence of deformation within the masses) from the previously resected urothelial carcinoma. The patient was palliated, and he shortly succumbed to his condition.
Conclusions
Urothelial carcinoma is an exceedingly rare cause of cardiac metastasis. CMR is an important imaging modality for localisation and characterisation of suspicious cardiac lesions, aiding in the diagnosis of cardiac metastasis.
Similar content being viewed by others
Background
The incidence of cardiac metastasis is highly variable in the literature and ranges from 2.3% to 18.3% [1, 2]. Approximately 90% of cardiac metastases are clinically silent and are often diagnosed post-mortem [1, 3, 4]. Urothelial carcinoma is a rare cause of cardiac metastasis, with only 25 reported cases noted in the literature [5,6,7,8,9,10,11,12,13]. The majority of these cases have described single myocardial metastases with varying patient presentations. We report a case of three cardiac metastatic lesions involving the myocardium, presenting with frequent febrile spikes, a month after a nephroureterectomy for urothelial carcinoma.
Case presentation
A 74-year-old gentleman presented to the accident and emergency department complaining of frequent febrile spikes and deterioration in general condition a month after undergoing a nephroureterectomy for urothelial carcinoma. Empirical antibiotics prescribed within the community did not produce any improvement. Examination upon presentation was within normal limits. The patient’s medical and surgical history included hypertension, hypercholesterolaemia, peripheral vascular disease and an uneventful coronary artery bypass surgery five months prior to presentation.
The urothelial malignancy was diagnosed after he initially presented with a few weeks’ history of fever, anorexia and weight loss. Computed tomography (CT) of the thorax, abdomen and pelvis had identified a right upper kidney pole hypodense lesion. Biopsy was performed which reported urothelial carcinoma. Subsequently, the patient underwent a nephroureterectomy which confirmed poorly differentiated, extensively necrotic, Grade 3 (World Health Organisation [WHO] classification) urothelial carcinoma (sarcomatoid variant type) with no lymph node involvement (pathological stage T3N0). The patient had been offered adjuvant chemotherapy due to the high predisposition for distant metastases, but he refused.
During the current admission, no septic focus or causative organism could be identified following multiple blood and urine cultures. Repeat CT of the thorax, abdomen and pelvis was performed, seven weeks following the prior CT, and this identified two new cardiac lesions at the apex of the left ventricle and another in the proximal interventricular wall (Fig. 1). In addition, a peritoneal lesion was noted. Metastatic lesions from the patient’s primary urothelial carcinoma were suspected, particularly since the patient refused post-operative chemotherapy.
Transthoracic echocardiography (TTE) could not identify the cardiac lesions. Cardiac magnetic resonance imaging (CMR) was performed which revealed two spherical intramyocardial masses at the basal septum and the left ventricular apex, and another lesion involving the anteromedial papillary muscle. Tissue characterisation of the lesions revealed a high fluid content, absence of fat, presence of a surrounding rim of increased extravascular space, absence of deformation within the masses, and avascular cores (Figs. 2, 3, 4, 5). These features were highly suggestive of intracardiac malignancy, and in this case, they likely represented metastases from the primary urothelial carcinoma.
Cardiac Magnetic Resonance Imaging: A Early Gadolinium enhancement in short axis view. Late Gadolinium enhancement CMR images in 4-chamber view (B) and short axis views (C, D) revealing two lesions at base of LV apex and base of interventricular septum. Lesions demonstrate no gadolinium enhancement indicating avascular cores
After multidisciplinary discussion, it was decided to proceed with a biopsy of the peritoneal lesion as it was deemed to be safer and more accessible than the cardiac lesions. An ultrasound-guided biopsy of the abdominal lesion confirmed metastases of the primary urothelial carcinoma. Therefore, given the biopsy result, together with the palliative approach at that stage, and the abundant clinical and imaging evidence favouring the diagnosis of cardiac metastases, a biopsy of the cardiac lesions was not justified.
Outcome and follow-up
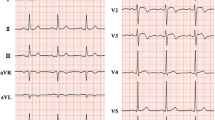
The patient was referred to palliative care in view of his poor medical condition. An electrocardiogram revealed new-onset ST elevations in inferior leads (III and aVF) with Q waves and ST depressions in leads I and aVL (Fig. 6). These changes were attributed to the patient’s cardiac metastases. Shortly following admission for presyncope and general deterioration, he suffered an ischaemic cerebrovascular event, eventually passing away within a few days.
Discussion
Urothelial carcinoma is a rare cause of cardiac metastasis, with only 25 cases reported in the literature. Furthermore, our case is unusual as there were multiple metastases. Fever has also been rarely reported as a presenting complaint.
Cardiac metastases are often clinically silent and are generally discovered during post-mortem examinations, or incidentally on imaging [1, 2]. Bussani et al. [2] conducted a study of 18,751 post-mortem examinations where they identified malignancy in 38.8% of cases, among which 9.1% (662 patients) had cardiac metastasis. From the 662 cases, 98.5% had metastases to other sites other than the heart, indicating that cardiac metastasis is usually a feature of widespread disease. The most common malignancies found to metastasise to the heart included lung, followed by breast and lymphoma or leukaemia. Urothelial carcinoma represented only 1.8% of all primary malignancies with cardiac metastasis, making it an exceptionally rare cause for cardiac metastases [2].
Pericardial involvement is the most frequently cited location of cardiac metastasis, followed by the myocardium; while the least common site is the endocardium [14]. Specific to urothelial metastasis, the majority of the cases reported involved the myocardium (19 cases), while the remaining 5 cases involved the pericardium. One case reported a lesion limited to the endocardial layer [5,6,7,8,9,10,11,12,13]. Similar to our case, only two other cases involved multiple cardiac metastatic lesions from a urothelial primary; Ueda et al. [6] reported a case of right and left myocardial metastases, while Sugimoto et al. [9] reported multiple myocardial metastatic nodules.
Patients with cardiac metastasis are often asymptomatic and are primarily noted on post-mortem examination, as mentioned above. If symptomatic, the symptoms reported by patients are often ambiguous. Symptoms of other organ metastases may be prevalent by the time metastasis to the heart occurs, explaining why cardiac metastases often remain undiagnosed. However, cardiac-specific symptoms may occur depending on the site of the metastatic lesions. Patients with pericardial metastasis may present with a pericarditis-like picture, including the development of a pericardial effusion and possibly tamponade [7, 9, 15]. Myocardial involvement may result in arrhythmic complications including life-threatening ventricular fibrillation or complete atrioventricular block [6, 16, 17]. Myocardial involvement may also compromise cardiac output mimicking congestive heart failure. Metastasis to the endocardium may cause left or right outflow obstruction with cardiogenic shock [17]. Any of the described symptoms in a patient diagnosed with malignancy should raise concerns for possible cardiac metastasis. Among the 25 reported cases of cardiac metastases from urothelial carcinoma, many reported non-specific symptoms such as fatigue, cough, and weight loss, among others. Shortness of breath was also reported which may have been secondary to tamponade, a compromised cardiac output or lung metastasis. Among these 25 patients, only 2 cases reported fever as one of the presenting symptoms, similar to our case [7, 8].
Imaging modalities are the main investigations aiding in the diagnosis of cardiac metastasis, however, an electrocardiogram (ECG) may also contribute by revealing low voltage complexes (due to a pericardial effusion), arrhythmias, or nonspecific ST-T wave abnormalities; the latter being reported in our case [18]. Chest x-ray and echocardiography may reveal a pericardial effusion, while echocardiography may also identify cardiac masses [17]. CT, CMR or positron emission tomography-computed tomography (PET-CT) offer more definite imaging to localise and characterise cardiac masses while excluding differentials such as intracardiac thrombus, vegetations, and benign lesions. Our case offers an insight into the role of CMR in cardiac metastasis diagnosis; an imaging modality that was not frequently used in the literature of similar cases.
CMR protocols vary depending on the institution and involve different sequences which must be tailored towards the suspected cardiac pathology. Commonly used sequences include black-blood T1-weighted sequences (with and without fat saturation and before and after contrast enhancement), black-blood T2-weighted imaging, cine imaging with a steady-state free-precession (SSFP) sequence and early and late gadolinium enhancement (LGE) imaging [19]. All these sequences were included in the reported case as part of the institution’s tumour protocol. Characteristics indicative of cardiac metastasis include smooth and spherical lesions, low or isointense T1-weighted images, hyperintense T2-weighted (owing to the high fluid content of malignant lesions), heterogenous LGE, no signal change on fat suppression sequence (absence of fat), presence of pericardial effusion (likely haemorrhagic), and haemorrhage within the mass [19,20,21]. The tumours in our case demonstrated the above-mentioned characteristics (Figs. 2, 3, 4, 5). Although a clinical diagnosis of cardiac metastasis can often be made on imaging, tissue histology remains the investigation of choice for diagnosis [15]. Cardiac biopsy and treatment of the patient’s condition in the case were deemed ineffectual due to his poor condition.
Conclusions
Urothelial carcinoma is a rare cause of cardiac metastasis, with only two reported cases of multiple metastatic lesions, and another two cases presenting with fever, analogous to our case. The myocardium is a common site for metastasis to the heart from urothelial carcinoma. CMR imaging is an important tool as it offers detailed characterisation and localisation, aiding in the diagnosis of cardiac metastasis.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- CMR:
-
Cardiac magnetic resonance
- CT:
-
Computed tomography
- TTE:
-
Transthoracic echocardiography
- ECG:
-
Electrocardiogram
- PET-CT:
-
Positron emission tomography-computed tomography
- LGE:
-
Late gadolinium enhancement
- SSFP:
-
Steady-state free-precession
References
Al-Mamgani A, Baartman L, Baaijens M, de Pree I, Incrocci L, Levendag PC (2008) Cardiac metastases. Int J Clin Oncol 13:369–372. https://doi.org/10.1007/s10147-007-0749-8
Bussani R, De-Giorgio F, Abbate A, Silvestri F (2007) Cardiac metastases. J Clin Pathol 60:27–34. https://doi.org/10.1136/jcp.2005.035105
Shapiro L (2001) Cardiac tumours: diagnosis and management. Heart 85:218–222. https://doi.org/10.1136/heart.85.2.218
Butany J, Nair V, Naseemuddin A, Nair GM, Catton C, Yau T (2005) Cardiac tumours: diagnosis and management. Lancet Oncol 6:219–228. https://doi.org/10.1016/S1470-2045(05)70093-0
Hattori S, Miyajima A, Maeda T, Takeda T, Morita S, Kosaka T, Kikuchi E, Oya M (2012) Metastatic urothelial carcinoma to pericardia manifested by dyspnea from cardiac tamponade during systemic chemotherapy: case report and literature review. Can Urol Assoc J 6:E184-188. https://doi.org/10.5489/cuaj.11130
Ueda N, Kawamura M, Nakazawa S, Hirai T, Kishikawa H, Nishimura K, Morimoto K (2014) Complete atrioventricular block due to cardiac metastasis from bladder cancer: case report. Hinyokika Kiyo 60:501–506
Khan R, Jehangir W, Tulpule S, Osman M, Singh S, Sen S (2016) Pericardial metastasis induced tamponade from urothelial carcinoma: a rare entity. Case Rep Med 2016:6162732. https://doi.org/10.1155/2016/6162732
Peck JR, Hitchcock CL, Maguire S, Dickerson J, Bush C (2012) Isolated cardiac metastasis from plasmacytoid urothelial carcinoma of the bladder. Exp Hematol Oncol 1:16. https://doi.org/10.1186/2162-3619-1-16
Sugimoto K, Tanaka M, Chiba H (2019) Myocardial rupture due to metastasis of urothelial carcinoma. Circ J 83:839. https://doi.org/10.1253/circj.CJ-18-0669
Arscott WT, Lal P, Mamtani R, O’Quinn R, Deo R, Jones J (2018) Long-term survival after treating cardiac metastasis with radiation and immune therapy: a case report. Cureus 10:2607. https://doi.org/10.7759/cureus.2607
Nakashima Y, Tanioka K, Kubo T, Yamasaki N, Yamasaki I, Syuin T, Kitaoka H (2015) Metastatic cardiac tumor from urothelial carcinoma detected by transthoracic echocardiography: a case report. J Med Case Rep 9:257. https://doi.org/10.1186/s13256-015-0740-3
Palam S, Kapoor R, Kulinski J (2018) A rare presentation of cardiac tamponade from metastatic urothelial carcinoma of the bladder. Case Rep Cardiol 2018:6750264. https://doi.org/10.1155/2018/6750264
Mountzios G, Bamias A, Dalianis A, Danias P, Pantelidaki E, Nanas J, Dimopoulos MA (2010) Endocardial metastases as the only site of relapse in a patient with bladder carcinoma: a case report and review of the literature. Int J Cardiol 140:e4-7. https://doi.org/10.1016/j.ijcard.2008.11.012
Lam KY, Dickens P, Chan AC (1993) Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med 117:1027–1031
Goldberg AD, Blankstein R, Padera RF (2013) Tumors metastatic to the heart. Circulation 128:1790–1794. https://doi.org/10.1161/CIRCULATIONAHA.112.000790
Michela C, Corrado C, Antonio DR, Fabrizio T, Stefano B, Lorenzo M, Ivana M, Francesco G, Claudio T (2011) Radiofrequency catheter ablation of life-threatening ventricular arrhythmias caused by left ventricular metastatic infiltration. Circ Arrhythm Electrophysiol 4:e7–e10. https://doi.org/10.1161/CIRCEP.110.961193
Reynen K, Köckeritz U, Strasser RH (2004) Metastases to the heart. Ann Oncol 15:375–381. https://doi.org/10.1093/annonc/mdh086
Cates CU, Virmani R, Vaughn WK, Robertson RM (1986) Electrocardiographic markers of cardiac metastasis. Am Heart J 112:1297–1303. https://doi.org/10.1016/0002-8703(86)90363-7
Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S (2013) MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology 268:26–43. https://doi.org/10.1148/radiol.13121239
Lichtenberger JP, Reynolds DA, Keung J, Keung E, Carter BW (2016) Metastasis to the heart: a radiologic approach to diagnosis with pathologic correlation. Am J Roentgenol 207:764–772. https://doi.org/10.2214/AJR.16.16148
O’Donnell DH, Abbara S, Chaithiraphan V, Yared K, Killeen RP, Cury RC, Dodd JD (2009) Cardiac tumors: optimal cardiac mr sequences and spectrum of imaging appearances. Am J Roentgenol 193:377–387. https://doi.org/10.2214/AJR.08.1895
Acknowledgements
No acknowledgements to disclose.
Funding
No funding was requested.
Author information
Authors and Affiliations
Contributions
NG: Conception and design, acquisition and interpretation of data, drafting the article, final approval, and agrees to be accountable for all aspects of the work. WC: Acquisition of data, critically revising the article, final approval and agrees to be accountable for all aspects of the work. AB: Acquisition of data, interpretation of data, critically revising the article, final approval and agrees to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient’s next-of-kin for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grech, N., Camilleri, W. & Borg, A. Multiple cardiac metastases from urothelial carcinoma case report. Egypt Heart J 74, 28 (2022). https://doi.org/10.1186/s43044-022-00264-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-022-00264-y