Abstract
Background
This meta-analysis aimed to assess the value of the C2HEST score to facilitate population screening and detection of AF risk in millions of populations and validate risk scores and their composition and discriminatory power for identifying people at high or low risk of AF. We searched major indexing databases, including Pubmed/Medline, ISI web of science, Scopus, Embase, and Cochrane central, using (“C2HEST” OR “risk scoring system” OR “risk score”) AND (“atrial fibrillation (AF)” OR “atrial flutter” OR “tachycardia, supraventricular” OR “heart atrium flutter”) without any language, study region or study type restrictions between 1990 and 2021 years. Analyses were done using Meta-DiSc. The title and abstract screening were conducted by two independent investigators.
Results
Totally 679 records were found through the initial search, of which ultimately, nine articles were included in the qualitative and quantitative analyses. The risk of AF accompanied every one-point increase of C2HEST score (OR 1.03, 95% CI 1.01–1.05, p < 0.00001), with a high heterogeneity across studies (I2 = 100%). The SROC for C2HEST score in the prediction of AF showed that the overall area under the curve (AUC) was 0.91 (95% CI 0.85–0.96), AUC in Asian population was 0.87 (95% CI: 0.78–0.95) versus non-Asian 0.95 (95% CI 0.91–0.99), and in general population was 0.92 (95% CI 0.85–0.99) versus those with chronic conditions 0.83 (95% CI 0.71–0.95), respectively.
Conclusions
The results of this research support the idea that this quick score has the opportunity for use as a risk assessment in patients' AF screening strategies.
Highlights
-
Use of C2HEST score to predict Atrial Fibrillation.
-
For identifying people at high or low risk of Atrial Fibrillation.
-
Assessment the value of the C2HEST score.
Similar content being viewed by others
Background
Atrial fibrillation (AF) is a common type of arrhythmia or irregular heartbeat, which is defined as a supraventricular tachyarrhythmia characterized by uncoordinated atrial activity and subsequent mechanical atrial failure [1]. AF by disrupting heart function and increasing stroke risk accounts a significant source of mortality [2]. It was demonstrated AF affects about 1% of people under 60 years and 8% of people over 80-year [3], and approximately 2.3 million people in North America and 4.5 million in the EU Member States suffer from this disease [4,5,6]. Surveys such as conducted by Kannel et al. have shown that about a third of hospitalizations for rhythm disorders are due to this disorder, which has grown by 66% in the last 20 years [7].
Main text
Several factors contribute to this increasing, including population aging, increased prevalence of chronic heart disease (CHD), and improving diagnostic ability due to the advancing of technologies and equipment [8]. Therapeutic strategies in managing AF are based on interventions that control heart rate or rhythm [9]. Thromboembolism is one of the life-threatening adverse events in AF that, for preventing it, anticoagulant therapy is essential. However, treatment and management of patients with AF should be based on the disease’s type [10].
To predict incident AF, numerous risk scores considering instrumental and laboratory factors have been established so far [11,12,13]. By predicting AF risk in a timely manner, especially using various risk scoring systems, it is possible to control the disease and prevent its complications by using preventive treatment methods [14]. The C2HEST score (C2, coronary artery disease or chronic obstructive pulmonary disease [1 point each]; H, hypertension [1 point]; E, elderly [age ≥ 75 years, 2 points]; S, systolic heart failure [2 points]; T, thyroid disease [hyperthyroidism, 1 point]), the latest, easy-to-use and most straightforward risk scoring system was initially introduced and validated through large population-based cohorts of healthy individuals and patients with chronic diseases [15,16,17].
Therefore, this systematic review and meta-analysis aimed to assess the value of the C2HEST score to facilitate population screening and detection of AF risk in over millions of general populations and those with chronic diseases, and the validation of risk scores and their composition and discriminatory power for identifying people at high or low risk of AF.
Methods
This systematic review and meta-analysis were conducted according to the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) [18] and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [19] and SEDATE (Synthesizing Evidence from Diagnostic Accuracy Tests) guidelines [20].
Search strategy
We searched major indexing databases, including Pubmed/Medline, ISI web of science (WOS), Scopus, Embase, and Cochrane central, using (“C2HEST” OR “riskscoring system” OR “risk score”) AND (“atrial fibrillation (AF)” OR “atrial flutter” OR “tachycardia, supraventricular” OR “heart atrium flutter”) without any language, study region, or study type restrictions between 1990 and 2021 years.
Inclusion criteria
Criteria for selecting studies were as follows, considering individuals from either the general population or those with chronic diseases susceptible to AF occurrence, and larger prospective, national, population-based studies using C2HEST score for predicting the risk of AF. Studies that evaluated the C2HEST score in other heart disorders or investigated other scoring systems in AF were excluded.
Study selections
After removing duplicated studies, two authors (HH and FR) independently screened titles and abstracts of potential papers considering pre-defined inclusion and exclusion criteria. Any disagreements were resolved by either re-evaluating the source article or consulting a third author (ME). Two independent investigators conducted the title and abstract screening.
Data extraction
Information, including author’s name, publication year, country, age, sample size, and study design.
Methodological quality assessment
Two reviewers (HH and FR) performed the quality assessment of included studies using the Newcastle–Ottawa Scale (NOS) and the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tools. Disagreements were resolved by either discussing or re-evaluating the original article with a third reviewer (ME).
Ethical consideration
Ethical committee approval and informed consent were not essential due to working on previously published studies.
Statistical analysis
We retrieved the odds ratio (OR) with 95% confidence interval (CI) from the eligible studies and calculated summary OR (SOR) with the random-effects or fixed-effect models depending on the level of heterogeneity to evaluate the association of C2HEST score with the risk of AF [21]. Afterward, we measured heterogeneity across studies using Cochran’s Q statistics and I2 test. When I2 values (more than 50%) showed a high heterogeneity sensitivity and subgroup analyses were performed to discover the heterogeneity source. A hierarchical receiver-operating characteristic summary (HSROC) curve and a summary receiver operating characteristic (SROC) curve have been mounted. All experiments were viewed with the HSROC curve as a circle and plotted. The area under the curve (AUC) was computed to determine the diagnostic precision. Approaches 1.0 to the AUC would mean outstanding results, and impaired performance would be suggested if it approaches 0.5. Among numerous subgroups, the 95% CI of the AUC was compared. When the sensitivity and specificity were directly unavailable, they were calculated according to the following formulas: sensitivity = TP/(TP + FN) and specificity = TN/(FP + TN). Publication bias was measured using Deeks’ regression test [22]. Subgroup analysis was done according to the NOS assessment, C2HEST score for AF prediction, Ethnicity, General population, and Chronic conditions. The analysis was conducted using version 1.4 of the Meta-DiSc software (https://meta-disc.software.informer.com/1.4/) [23] and Revman 5.3.
Results
Search results
Totally 679 records were found through the initial search. Of 679 articles, 120 duplicated studies were found, and 109 were omitted due to irrelevant titles and abstracts. The rest 450 were entered the full-text screening, of which 441 were excluded due to pre-defined inclusion criteria. Ultimately, nine articles were included in the qualitative and quantitative analyses (Fig. 1).
Study characteristics
There were 6,293,676 general population and 2,741,896 patients in the nine eligible studies, of which 310,649 cases developed AF. Five studies sampled individuals from the general population [14, 15, 24,25,26], while the rest four included patients with chronic conditions [16, 27,28,29] (Table 1). In general population, the average age of the included participants was from 34.0 to 62.5 years (females took up 10.8–58%); whereas, in the chronic condition population, the average age of the included participants was from 52.6 to 70.8 years (females took up 47–54.7%). The average C2HEST score of the included participants was from 0.32 to 4.7. The majority of the included participants had hypertension among various comorbidities, ranging from 15.28 to 91.99%.
Meta-analysis
Five of nine included studies were rated as high-quality according to the NOS assessment, and the rest four were rated as medium quality studies (Additional file 1: Table S1). Our data have shown that the risk of AF is accompanied 3% by every one-point increase of C2HEST score (OR 1.03, 95% CI 1.01–1.05, p < 0.00001), with a high heterogeneity across studies (I2 = 100%) (Fig. 2). Six of the nine included studies observed the performance of C2HEST score for AF prediction [15, 16, 24, 27, 28, 30], of which four of them rated as medium quality studies using the QUADAS-2 framework (Additional file 2: Table S2). We retrieved the sensitivity, specificity, and accuracy test result in the nine included studies. The sensitivity of C2HEST score in predicting AF was from 66.9 to 94.8%, specificity from 51.58 to 98.18%, and accuracy from 59.21 to 78.95% (Additional file 3: Table S3).
Our pooled analysis consequently revealed that the C2HEST score had reasonably higher sensitivity in predicting the AF, especially in the Asian comparison to non-Asian population (Table 2).
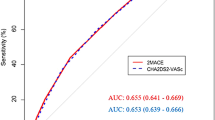
The SROC for C2HEST score in the prediction of AF showed that the overall area under the curve (AUC) was 0.91 (95% CI 0.85–0.96) (Fig. 3A), AUC in Asian population was 0.87 (95% CI 0.78–0.95) versus non-Asian 0.95 (95% CI 0.91–0.99) (Fig. 3B, C), and in general population was 0.92 (95% CI 0.85–0.99) versus those with chronic conditions 0.83 (95% CI 0.71–0.95) (Fig. 3D, E), respectively.
Summary receiver operating characteristic curve (SROC) analysis. The red circle symbol represents the summary estimate of sensitivity and specificity of the C2HEST score using a bivariate random-effects regression model. A dotted line surrounds the circle represents the 95% confidence interval. AUC area under the curve. A The overall AUC, B Asian, C non-Asian, D general population, and E chronic conditions
Discussion
The result of this study indicates a positive association between the C2HEST score and the AF. The most prominent finding to emerge from the analysis is that each one-point increase in C2HEST score was associated with risk of AF, on the other hand, our analysis showed that none of the subgroups were significantly different in any of the measured variables except for the specificity between general population and chronic condition.
Therefore, the AUC and pooled specificity of C2HEST score in the general population versus those with chronic conditions were higher. Moreover, this study's pooled specificity and sensitivity are in line with those of previous studies in the 86.5–89.8 range and 75.01–78.6 range, respectively [15, 27, 28, 30]. The highest OR was observed in the studies conducted by Guo et al. (OR 1.6, 95% CI 0.96–1.17) and Liang et al. (OR 1.6, 95% CI 1.05–1.07) [29, 30], and the lowest was observed in Lip et al., (OR 1, 95% CI 1–1) and Li et al., reports (OR 1, 95% CI 1–1.03) [15, 16]. Also, Guo et al., Liag et al., and Hu and Lin included high-risk population with hypertension (HTN), heart failure (HF), diabetes mellitus (DM), coronary artery disease (CAD), and Chronic obstructive pulmonary disease (COPD) [27, 29, 30].
A recent study that set out to determine the usability of C2HEST and HATCH scores in AF prediction demonstrated that the C2HEST score appeared to be more predictive of AF versus HATCH score [24]. This agree with Li et al. findings that the C2HEST score can be used as a simple clinical tool to determine an individual’s probability of developing AF in Asians who do not have structural heart disease (SHD) [15]. However, the AUROC values for CHA2DS2-VASc and C2HEST are almost equal, meaning that there is a little difference in predictive ability [27]. In that case, white European population hospitalized with prior ischemic stroke, the C2HEST score performed well in predicting the risk of experiencing event AF [28].
Furthermore, a higher risk C2HEST score was linked to an increased risk of new onset AF. More extensive efforts for screening and diagnosing event AF may be considered for these patients [16]. In addition, the C2HEST score, particularly when paired with symptoms, can make a population-based screening and prevention approach for AF more feasible [30].
Detailed examination of Identifying At-Risk Patients C2HEST score by Li et al. has shown that in patients without AF who had a cardiac implantable electronic unit; the C2HEST score estimated the occurrence of sustained atrial high-rate episodes (SAHREs); consequently, patients with a C2HEST score of four having the greatest chance [31]. Also, in patients with heart failure and retained ejection fraction, the C2HEST score could forecast the likelihood of event AF, death, and hospitalization for heart failure with preserved ejection fraction (HFpEF). Its flexibility can make fast risk evaluations possible in busy clinical settings [29].
Limitations
This study has some limitations; a patient with hypertension for 20 years is more likely to encounter AF than another with only a two-year history of hypertension. Also, the degree of compliance to treatment and the degree of control of CHEST components were not mentioned, so the drugs given can affect AF.
Conclusions
This investigation aimed to achieve a reliable, accurate, and easy-to-performance method for predicting AF development. This study has identified that the C2HEST score has good performance in predicting AF and could help identify the individuals at high risk of AF in the Asian and non-Asian populations. The results of this research support the idea that this quick score can be used as a risk assessment in patients' AF screening strategies.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the [Pubmed, Web of Science, Scopus, EM Base] repository.
Abbreviations
- WOS:
-
Web of science
- AF:
-
Atrial fibrillation
- CHD:
-
Chronic heart disease
- C2HEST score:
-
C2, coronary artery disease or chronic obstructive pulmonary disease; H, hypertension; E, elderly (age ≥ 75 years); S, systolic heart failure; T, thyroid disease (hyperthyroidism)
- MOOSE:
-
Meta-analyses Of Observational Studies in Epidemiology
- PRISMA:
-
Systematic reviews and Meta-Analyses
- SEDATE:
-
Synthesizing Evidence from Diagnostic Accuracy Tests
- NOS:
-
Newcastle–Ottawa Scale
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SOR:
-
Summary OR
- HSROC:
-
Hierarchical receiver-operating characteristic summary
- SROC:
-
Summary receiver operating characteristic
- AUC:
-
Area under the curve
- HTN:
-
Hypertension
- HF:
-
Heart failure
- DM:
-
Diabetes mellitus
- CAD:
-
Coronary artery disease
- COPD:
-
Chronic obstructive pulmonary disease
- SHD:
-
Structural heart disease
- SAHREs:
-
Sustained atrial high-rate episodes
- HFpEF:
-
Heart failure with preserved ejection fraction
References
Lip GYH, Tello-Montoliu A (2006) Management of atrial fibrillation. Heart 92(8):1177–1182
Pellman J, Sheikh F (2015) Atrial fibrillation: mechanisms, therapeutics, and future directions. Compr Physiol 5(2):649–665
Zathar Z, Karunatilleke A, Fawzy AM, Lip GYH (2019) Atrial fibrillation in older people: concepts and controversies. Front Med (Lausanne) 6:175–175
Savarese G, Lund LH (2017) Global public health burden of heart failure. Card Fail Rev 3(1):7–11
Haywood LJ (2011) Racial/ethnic differences in the prevalence of atrial fibrillation among older adults–a cross-sectional study. J Natl Med Assoc 103(2):180–181
Shen AY, Contreras R, Sobnosky S, Shah AI, Ichiuji AM, Jorgensen MB, Brar SS, Chen W (2010) Racial/ethnic differences in the prevalence of atrial fibrillation among older adults–a cross-sectional study. J Natl Med Assoc 102(10):906–913
Kannel WB, Benjamin EJ (2008) Status of the epidemiology of atrial fibrillation. Med Clin N Am 92(1):17–ix
Friberg J, Buch P, Scharling H, Gadsbøll N, Jensen GB (2003) Rising rates of hospital admissions for atrial fibrillation. Epidemiology 14(6):666–672
Kirchhof P, Curtis AB, Skanes AC, Gillis AM, Samuel Wann L, John Camm A (2013) Atrial fibrillation guidelines across the Atlantic: a comparison of the current recommendations of the European Society of Cardiology/European Heart Rhythm Association/European Association of Cardiothoracic Surgeons, the American College of Cardiology Foundation/American Heart Association/Heart Rhythm Society, and the Canadian Cardiovascular Society. Eur Heart J 34(20):1471–1474
Nguyen TN, Hilmer SN, Cumming RG (2013) Review of epidemiology and management of atrial fibrillation in developing countries. Int J Cardiol 167(6):2412–2420
Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D’Agostino RB, Newton-Cheh C, Yamamoto JF, Magnani JW, Tadros TM et al (2009) Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. The Lancet 373(9665):739–745
Chamberlain AM, Agarwal SK, Folsom AR, Soliman EZ, Chambless LE, Crow R, Ambrose M, Alonso A (2011) A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the Atherosclerosis Risk In Communities [ARIC] Study). Am J Cardiol 107(1):85–91
Alonso A, Krijthe BP, Aspelund T, Stepas KA, Pencina MJ, Moser CB, Sinner MF, Sotoodehnia N, Fontes JD, Janssens AC et al (2013) Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc 2(2):e0001002
Chao T-F, Chen S-A (2014) Stroke risk predictor scoring systems in atrial fibrillation. J Atr Fibrillation 6(5):998–998
Li YG, Pastori D, Farcomeni A, Yang PS, Jang E, Joung B, Wang YT, Guo YT, Lip GYH (2019) A simple clinical risk score (C(2)HEST) for predicting incident atrial fibrillation in Asian subjects: derivation in 471,446 Chinese subjects, with internal validation and external application in 451,199 Korean subjects. Chest 155(3):510–518
Lip GYH, Skjøth F, Nielsen PB, Larsen TB (2020) Evaluation of the C(2)HEST risk score as a possible opportunistic screening tool for incident atrial fibrillation in a healthy population (from a nationwide Danish cohort study). Am J Cardiol 125(1):48–54
Li Y-G, Bisson A, Bodin A, Herbert J, Grammatico-Guillon L, Joung B, Wang Y-T, Lip G, Fauchier L (2019) C2 HEST score and prediction of incident atrial fibrillation in poststroke patients: a French nationwide study. J Am Heart Assoc 8:e012546
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1-34
Sotiriadis A, Papatheodorou SI, Martins WP (2016) Synthesizing Evidence from Diagnostic Accuracy TEsts: the SEDATE guideline. Ultrasound Obstet Gynecol 47(3):386–395
Lathyris D, Haidich AB (2021) Meta-analysis of diagnostic test accuracy: just another meta-analysis?. Intensive Crit Care Nurs 1028
Song F, Khan KS, Dinnes J, Sutton AJ (2002) Asymmetric funnel plots and publication bias in meta-analyses of diagnostic accuracy. Int J Epidemiol 31(1):88–95
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31
Hu WS, Lin CL (2020) Prediction of new-onset atrial fibrillation for general population in Asia: a comparison of C2HEST and HATCH scores. Int J Cardiol 313:60–63
Hulme OL, Khurshid S, Weng LC, Anderson CD, Wang EY, Ashburner JM, Ko D, McManus DD, Benjamin EJ, Ellinor PT et al (2019) Development and validation of a prediction model for atrial fibrillation using electronic health records. JACC Clin Electrophysiol 5(11):1331–1341
Khurshid S, Kartoun U, Ashburner JM, Trinquart L, Philippakis A, Khera AV, Ellinor PT, Ng K, Lubitz SA (2021) Performance of atrial fibrillation risk prediction models in over 4 million individuals. Circ Arrhythm Electrophysiol 14(1):e008997
Hu WS, Lin CL (2020) Comparison of CHA2DS2-VASc and C2HEST scores for predicting the incidence of atrial fibrillation among patients with end-stage renal disease. Perfusion 35(8):842–846
Li YG, Bisson A, Bodin A, Herbert J, Grammatico-Guillon L, Joung B, Wang YT, Lip GYH, Fauchier L (2019) C(2) HEST score and prediction of incident atrial fibrillation in poststroke patients: a French nationwide study. J Am Heart Assoc 8(13):12546
Liang W, Wu Y, Xue R, Wu Z, Wu D, He J, Dong Y, Lip GYH, Zhu W, Liu C (2021) C(2)HEST score predicts clinical outcomes in heart failure with preserved ejection fraction: a secondary analysis of the TOPCAT trial. BMC Med 19(1):44
Guo Y, Wang H, Zhang H, Chen Y, Lip GYH (2020) Population-based screening or targeted screening based on initial clinical risk assessment for atrial fibrillation: a report from the Huawei heart study. J Clin Med 9(5):1493
Li YG, Pastori D, Miyazawa K, Shahid F, Lip GYH (2021) Identifying at-risk patients for sustained atrial high-rate episodes using the C(2)HEST score: the West Birmingham atrial fibrillation project. J Am Heart Assoc 10(6):7519
Acknowledgements
We wish to thank all our colleagues in Allied Health Sciences School, Ahvaz Jundishapur University of Medical Sciences.
Funding
None.
Author information
Authors and Affiliations
Contributions
FR conceived the manuscript and revised it. HH and KSh did the statistical analysis, wrote the manuscript, and prepared tables and figures. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest. All procedure performs in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of HELSINKI and its later amendments or compare ethical strand.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Table S1: Study quality of included studies based on the Newcastle-Ottawa scale.
Additional file 2
. Table S2: Study quality of included studies based on the QUADAS-2 tool.
Additional file 3
. Table S3: Different predictive ability of C2HEST score for AF-associated risk in Asian patients or non-Asian patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haybar, H., Shirbandi, K. & Rahim, F. C2HEST score for atrial fibrillation risk prediction models: a Diagnostic Accuracy Tests meta-analysis. Egypt Heart J 73, 104 (2021). https://doi.org/10.1186/s43044-021-00230-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-021-00230-0