Abstract
Background
People with type 2 diabetes mellitus (DM) are at increased risk of cardiovascular disease (CVD). Cardiovascular autonomic neuropathy (CAN) is an underdiagnosed risk factor for CVD, which is prevalent among people with 2DM and can lead to CVD and CVD-related mortality. Little is known about the risk factors associated with CAN in type 2DM. Thus, the study was aimed to assess CAN using five cardiovascular autonomic reflex tests (represented by Ewing’s score) and explore the factors associated with CAN in people with type 2DM. The studied factors include traditional and serological CVD risk factors obtained from a fasting blood sample and cardiorespiratory fitness (CRF) obtained via attainment of the highest peak of volumes of O2 (VO2Peak).
Results
Univariate analysis revealed a significant positive correlation between resting systolic blood pressure (SBP) and Ewing’s score (r=0.47, p=.02) and an inverse correlation between VO2Peak and Ewing’s score (r=−0.64, p=.001). Multivariate linear regression revealed that a significant model that included resting SBP and VO2Peak explained 93.8% of Ewing’s score variance.
Conclusion
CAN was associated with two CVD parameters, including resting SBP and CRF, which may indicate the importance of controlling these two factors to prevent or reduce CAN in people with type 2DM.
Similar content being viewed by others
Background
Diabetes mellitus (DM) is a metabolic disorder characterized by an elevated level of glucose (hyperglycemia) and disturbance of fat, protein, and carbohydrate metabolism caused mainly by the inability to produce or to utilize insulin [1]. DM may start early in life and be carried for a long time asymptomatic [2]. A report showed that the number of people with DM was 366 million in 2011, and half of these people did not know they have DM [3]. DM is alarmingly growing, as it is estimated that the number of people with DM worldwide will increase up to 552 million [3].
People with DM (type 1 or type 2) have an increased risk of cardiovascular disease (CVD) [4, 5], which accounts for more than 60% of the mortality rate among people with DM [6]. The risk of death from coronary heart disease, a type of CVD, is threefold higher in people with type 2DM than non-diabetic people [7]. A cluster of CVD risk factors is prevalent in people with DM, which contribute to the increased risk of CVD, including obesity [8], hypertension [9], dyslipidemia [9], physical inactivity [10], and cardiovascular autonomic neuropathy (CAN) [11, 12].
CAN is one of the underdiagnosed DM complications and one of the major risk factors for CVD in people with DM [13]. It is known as the impairment of the nerve innervated by the autonomic nervous system (ANS) that regulates the heart and the blood vessels [14]. The prevalence of CAN is higher in type 2DM and has been reported between 31 and 73%, whereas, in type 1DM, the prevalence reported between 17 and 66% [13]. Different methodologies and tests to examine CAN have contributed to this variation in prevalence. The presence of CAN among people with DM has been correlated with an increased 5-year CVD mortality rate [15]. Symptomatic manifestations associated with the presence of CAN include resting tachycardia, postural hypotension, exercise intolerance, silent myocardial ischemia, or infarction, and left ventricular systolic and diastolic function [5, 15].
Assessment of CAN involves both arms of the autonomic nervous system (ANS), the sympathetic and parasympathetic nervous system functioning. The gold standard method to assess CAN was established by Ewing et al. [16], which include a set of five cardiovascular autonomic reflex tests. Blood pressure (BP) response to standing, Valsalva manoeuver, and BP response to sustained handgrip test assess sympathetic function, and heart rate (HR) response to standing and HR response to deep breathing are to assess parasympathetic function. These tests have shown high validity and reliability in measuring ANS function in people with DM [17].
Little is known about the risk factors associated with CAN in people with DM. In longitudinal studies, several risk factors in people with DM were linked with increased risk of CAN, including duration of the disease, glycemic control [18], and CVD risk factors (obesity, smoking, hypertension, and hyperlipidemia) [13]. Age and presence of diabetic complications such as diabetic retinopathy and nephropathy were also reported in cross-sectional studies [19,20,21]. However, these findings were inconclusive and not generalizable as some of these studies were limited to type 1DM [21], and the information about the CVD risk factors for CAN in type 2DM was limited. For example, low cardiorespiratory fitness (CRF) is one of the main risk factors for CVD. Yet, in cross-sectional studies, it was not included as a potential risk factor for CAN. In a comparison study between type 1DM and type 2DM, CRF was reduced in type 2DM less than type 1DM, and there was a strong association between CAN and CRF only in type 1DM [22]. Thus, due to the limited information about the risk factors associated with CAN in type 2DM, the current study was aimed to assess CAN using cardiovascular autonomic reflex tests and explore the factors associated with CAN in people with type 2DM. It was hypothesized that CAN will be associated with CVD risk factors.
Methods
Study population
Twenty-six people with type 2DM (HbA1C ≥ 48 mmol/mol, and fasting glucose > 7.0 mmol) were recruited from diabetes educational classes between 2015 and 2016 at Brierley Hill Health and Social Care Centre, Dudley, UK. People with comorbidity incompatible with exercise as per American College of Sports Medicine (ACSM) guidelines [23], atrial fibrillation, established CVD, established or confirmed diagnosis of CAN prior to participation, neurological problems (e.g., Parkinsonism, dementia), uncontrolled hypertension (170/80 mmHg), or uncontrolled glucose level above 200 mmol/l were excluded. Additionally, severe pulmonary disease (e.g., COPD, pulmonary fibrosis) and mental or physical impairment causing the inability to perform any test were excluded. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the National Research Ethics Committee (IRA ID: 169234, Ref: 15/EM/0138), and all participants provided written informed consent before participation.
Protocol
The protocol used in the current study is similar to what was reported by Osailan et al. [24] with the addition of cardiovascular autonomic reflex tests. Participants were invited to the research laboratory on two different occasions. During visit one, height was measured to the nearest 0.5 cm using a standard height measure (Seca 214 Road Rod), weight and body mass index (BMI) were measured using a Tanita BC 418 MA Segmental Body Composition Analyser (Tanita Corporation, Tokyo, Japan), and brachial blood pressure was taken using an electronic sphygmomanometer (Datascope Accutor, Mahwah, NJ, USA). At the same time, the participant was seated, then a fasted blood sample was taken. This was followed by performing five cardiovascular autonomic reflex tests. On the second visit, an appropriate mask was fitted to the participant covering the nose and mouth to analyze inspired and expired gases, and electrocardiograph (ECG) (12-channel ECG, Custo cardio 200, Custo med, Leipzig, Germany) electrodes were attached (see Fig. 1). Two-minute baseline measurement was used to measure resting heart rate and volume of O2 consumption while seated, followed by an exercise tolerance test (ETT), which included 6 min of familiarization phase. Finally, a minimum of 6 min post ETT as a recovery period.
Collection of blood sample
Blood was collected from the patient’s antecubital vein using a butterfly needle equipped with the vacutainer system. The blood samples were analyzed for serological risk factors for cardiovascular disease, including full blood count and lipids. All analyses were carried out using routine laboratory procedures in the hospital’s research laboratory.
Cardiovascular autonomic reflex test
Five cardiovascular autonomic reflex tests were conducted consecutively, while ECG electrodes were attached to the participant to monitor heart rate changes during specific tasks. The cardiovascular autonomic reflex tests, commonly known as Ewing’s score, are valid and reliable tests for detecting CAN [17]. The credit of the development of these tests is to Ewing. Clarke and coworkers from Edinburgh. The total scoring of Ewing’s score is based on the achieved scores from a battery of five tests, including:
-
Valsalva manoeuver
-
Heart rate (HR) response to standing up
-
HR response to deep breathing
-
Blood pressure response to standing up
-
Blood pressure response to a sustained handgrip
Valsalva manoeuver
The participant was instructed to blow into a mouthpiece (with a closed glottis) with a pressure meter while maintaining a pressure of 40 mmHg for 15 s. The longest R-R interval ratio immediately after the manoeuver to the shortest R-R interval during the manoeuver was measured. Then, an average of three readings was taken (see Table 1 for interpretation of the test results).
HR response to standing
The participant was lying down in a supine position for 5 min, then was instructed to stand up immediately unaided without previous warning. The test provokes an increase in HR at the 15th beat, followed by a decrease in HR at the 30th beat. Thus, a ratio of 30:15 was measured and was quantified based on the longest R-R interval at the 30th beat to the shortest R-R interval at the 15th beat (see Table 1 for interpretation of the results of the test).
HR response to deep breathing
Six breaths per minute were elicited using a metronome for 2 min for familiarization while in a seated position. After that, every minute, the maximum HR and minimum HR were recorded for three consecutive breath cycles. The difference between the maximum and minimum HR was measured from the average readings during the three breath cycles (see Table 1 for interpretation of the test results).
Blood pressure response to standing
The participant was lying supine for 5 min, with an automated sphygmomanometer attached. Then at the end of the 5th min, blood pressure was measured. Then, the participant was instructed to stand up immediately, and another blood pressure reading was recorded. The difference between supine systolic blood pressure and standing systolic blood pressure was calculated (see Table 1 for interpretation of the test results).
Blood pressure response to a sustained handgrip
The participant was asked to practice using the dynamometer to obtain a full maximum handgrip. After 1 min of rest, resting blood pressure was measured. Then, the participant was asked to maintain 30% of the achieved maximum handgrip for 5 min. During every minute, blood pressure was measured. The difference between the resting diastolic blood pressure and the diastolic blood pressure at the end of the last minute was calculated (see Table 1 for interpretation of the test results).
Exercise tolerance test (ETT)
Before ETT, and for the participant’s safety, it was a criterion to have capillary blood glucose between 7 and 14 mmol/L [25]. ETT was performed on a treadmill (HP Cosmos Mercury, Nussdoerf-Traunstien, Germany). Six minutes was given to each participant for familiarization purposes before commencing the individualized ramp protocol test, which was modified according to the patient’s fitness and physical abilities [26]. During this familiarization period, the speed was set at the participant’s preference (approximately three kph) with 0% inclination for 6 min. After that, the treadmill’s speed was increased up to maximum brisk walking based on the participant’s ability. Then, the speed was set to be constant (maximum brisk walking) throughout the test while increasing the inclination by 1% every minute. Peak oxygen consumption (VO2Peak) was calculated using breath-by-by-breath gas analyses (Metalyzer 3B, Cortex, Leipzig, Germany). Heart rate was recorded before commencement, throughout the ETT, and during the recovery period using ECG. If volitional exhaustion was reached during ETT, or any relative or absolute contraindications of ACSM’s guidelines were met [23], the test was immediately terminated. Upon the test’s termination, the participant was seated on the chair for up to 6 min as a recovery period. A cardiac physiologist supervised the tests to monitor the relative and absolute contraindications. The cardiac physiologist was blinded to the aim of the study.
Outcome measures
Cardiovascular autonomic reflex test
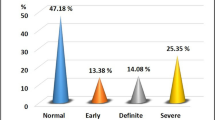
The scoring system used for each task’s results was based on the cut-off values suggested by Ewing et al. [16]. The cut-off values are presented in Table 1. A 0 (zero) score was given for the normal result, 0.5 for a borderline result, and 1 for the abnormal result (see Table 1). Thus, each participant’s total score was between 0 and 5 out of the five tests and was presented as Ewing’s score.
Blood sample analysis
Blood samples were analyzed for total cholesterol, triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL). Insulin resistance was analyzed using homoeostasis model assessment (HOMA) [27].
Cardiorespiratory fitness (VO2peak)
Peak aerobic capacity (VO2peak) was measured via calibrated breath-by-breath gas analyzer during treadmill ETT. Inspired and expired gas data were averaged every 2 s. VO2 reading data were further smoothened by taking the average of VO2 every 28 s (taking an average of 14 readings of VO2 ml/min). VO2peak was defined as the highest VO2 during the test and was expressed as ml/min/kg.
Statistical analysis
Statistical analysis was performed using SPSS27 (Chicago, IL, USA). The normality of the variables was tested using the Kolmogorov-Smirnov test. Normally distributed variables were presented as means and standard deviation. Skewed variables (body mass index, HOMA, and Ewing’s score) were presented as a median and interquartile range). Due to some of the variables’ skewness, including the main outcome measure, the bivariate spearman’s rank correlation was used to assess the relationship between Ewing’s score and other variables. Linear regression (using the enter method) was used to identify the independent factors associated with Ewing’s score. Only the variables significantly correlated with Ewing’s score in the univariate analysis were entered as independent variables and Ewing’s score as the dependent variable (all in one block). The level of significance for the analysis was set at ≤ 0.05. Power calculation analysis (GPower version 3.1) using a priori test indicated that the sample size required to achieve the power of (1-β error probability) = 0.85 was 26 with an effect size (d) of 0.55.
Results
Characteristics of the participants
The demographic characteristics of twenty-six type 2DM (60.8 ± 10.4 years, 38.5% female) are presented in Table 2. Comorbidities within the participants were bronchitis (3.8%), hypothyroidism (3.8%), depression (3.8%), sleep apnea (3.8%), osteoarthritis (3.8%), and osteoporosis (3.8%), and 11.5% were current smokers. The medications were not altered or discontinued at the time of the study. The most common medications used by the participants were statins (46.2%), Biguanides (53.8 %), and angiotensin-converting enzyme inhibitors (ACE inhibitors) (34.6%). Other medications are demonstrated in Table 2. All medications used by the participants were orally administered.
Correlation
Correlational analyses were used to assess the factors associated with Ewing’s score. Two variables were significantly associated with Ewing’s score. Resting SBP was positively associated with Ewing’s score (r (23) = 0.47, p= .02) (Fig. 2), whereas VO2peak was inversely associated with Ewing’s score (r (21) = −0.64, p= .001) (Fig. 3) (see Table 3). This indicated that higher resting SBP and poor CRF are related to higher abnormal cardiovascular autonomic reflex tests.
Linear regression
Linear regression was used to identify if related variables in the univariate analysis significantly predict Ewing’s score. Only the variables significantly correlated with Ewing’s score in the univariate analysis were entered in a multivariate linear regression analysis. Resting SBP and VO2peak were entered as independent variables and Ewing’s score as the dependent variable (see Table 4). The results of the regression indicated that a significant model, which included resting SBP and VO2peak explained 93.8% of the variance in Ewing’s score (F (2, 21) = 158.,8, p < .000).
Discussion
The current study was aimed to assess the relationship between common CVD risk factors and CAN assessed by cardiovascular autonomic reflex tests (identified by Ewing’s score). Not all CVD risk factors were associated with Ewing’s score. However, only two variables were moderately associated with Ewing’s score. The study showed that Ewing’s score was positively associated with resting SBP and inversely associated with CRF (measured via VO2peak). Besides, the multivariate linear regression showed a significant model which included resting SBP and VO2peak as independent predictors of Ewing’s score. This model explained most of the variance in Ewing’s score in the sample. This may suggest that high systolic blood pressure and low CRF contribute to worse Ewing’s score and, therefore, contribute to CAN.
According to the Ewing and colleagues method, the gold standard to measure the CAN is cardiovascular autonomic reflex tests [16]. The five tests reflect both arms of the sympathetic and parasympathetic nervous system, and a minimum of two abnormal tests define the presence of CAN in people with DM [28]. The presence of CAN with two abnormal tests was linked to higher CVD mortality rates [12]. Therefore, identifying risk factors associated with CAN may help health care professionals attenuate these factors and implement strategies to reduce future risk and mortality.
Studies investigating the risk factors associated with CAN in people with DM (type 1 and type 2) are scarce. In a study comparing between type 1 and type 2DM, a significant association was reported between the total scores of the cardiovascular autonomic reflex tests and SBP in type 2DM, whereas multiple significant associations were reported with type 1DM, including BMI, SBP, and HbA1c [29]. A similar significant moderate association (r = 0.54) was reported in the previous and current study between CAN and SBP among type 2DM [29]. Another study looking at the correlates of risk factors with CAN in pre-diabetic and DM people reported SBP as the only factor significantly associated with CAN [30]. In contrast to previous studies, a study in newly diagnosed type 2DM showed that BMI was independently associated with CAN after adjustment for age, sex, HbA1, pulse pressure, triglyceride-to-HDL cholesterol ratio, kidney function parameters, and antihypertensive treatment [31]. Peripheral neuropathy, prolonged QTc, higher age, and longer disease duration were reported to be associated with CAN in a different study among people with type 2DM [32]. Similar factors were also reported in another study with the addition of HbA1c, DBP, and Lower HDL cholesterol associated with CAN, however, in type 1DM [33]. Overall, it is complicated to understand this variation in the findings from different studies, but multiple reasons may contribute to it, such as different types of DM and different methodologies in the assessment of CAN. Some studies did not utilize the total score of the cardiovascular autonomic reflex tests, instead used percentiles of categories (early CAN, confirmed CAN, severe CAN) [31] and some utilized two tests only out of the five tests [33]. Therefore, it is difficult to relate the findings of the current study to the former ones.
In parallel with many previous studies, the current study reported a moderate association between high SBP and CAN. This association between SBP and CAN may be explained simply due to the role of sympathetic activity dominance over the parasympathetic activity in the increase of blood pressure [34, 35]. The function of ANS mainly involves both arms of the ANS working in balance with each other. However, with CAN, the balance between the two arms is absent or reduced. This mainly is manifested by reduced parasympathetic activity and dominant sympathetic influence over the heart and vascular system, especially in the muscular structure [36]. Indeed, sympathetic hyperactivity and higher sympathetic neural discharge are greater among people with type 2DM [37]. Furthermore, in vitro studies, it was found that replication of vascular smooth muscles is increased with catecholamines (e.g., adrenalin, noradrenalin), which may lead to vascular wall hyperplasia [38] and may eventually lead to arterial stiffening [39]. The positive association between SBP and CAN emphasize the importance of controlling blood pressure among people with type 2DM.
Surprisingly, no association was found in the current study between multiple traditional and serological CVD risk factors with Ewing’s score. Among the traditional CVD risk factors, BMI was one of the reported factors associated with CAN. In the current study, the absence of association between BMI or body fats percentage with CAN is perhaps due to the smaller sample size from other studies, which reported an inverse association [29, 31, 40]. This also applies to other CVD risk factors such as age and body fats percentage. The majority of the participants were on various medications, which can have a positive influence on many risk factors studied in the current study. For example, almost half of the participants used statins; thus, serological CVD risk factors such as cholesterol, triglycerides, and HDL were within the normal ranges (see Table 2). This might contribute to the absence of association between the factors mentioned earlier with CAN. Insulin resistance measured via HOMA was also found to be associated with CAN pre-diabetic people [41]. However, in the current study, the smaller sample size and different studied population may have contributed to the lack of detection of this association. These are just speculations, and further studies are needed to clarify these associations with the control of medications when possible.
To the best of knowledge, this is the first study that investigated the association in a cross-sectional study between CRF and CAN in people with type 2DM. Only one study was found assessing this relationship among recently diagnosed people with type 1 and 2 DM. Despite the reduction in CRF in type 2DM people more than type 1DM people, the inverse association between CRF and CAN was reported among people with type 1DM only but not among people with type 2DM [22]. In contrast, the current study found an inverse association between CRF and CAN in people with type 2DM. It is difficult to compare the findings of the current study with the former one due to the variation in methodology in the assessment of ANS function as the current study utilized cardiovascular autonomic reflex tests, whereas the former used heart rate variability (HRV) indices.
To explain the relationship between CRF and CAN, it is well-known that regular exercise and physical activity increase parasympathetic activity and reduce sympathetic hyperactivity in people with type 2DM [42]. Thus, concerning the inverse relationship between CRF and CAN, it is plausible that the reduction of CRF will alter parasympathetic activity via more influence from sympathetic hyperactivity [43]. Improved CRF is known to be associated with better baroreflex sensitivity, which is known to have a better regulatory functioning from ANS, and thus better regulatory function over the heart and vascular system. Regular aerobic exercises may aid ANS adaptation toward parasympathetic predominance via better vagal modulation and reduced sympathetic activity [44]. The association between CRF and CAN reported in the current study indicates the significance of targeting people with type 2DM to be enrolled in exercise training programs to prevent autonomic deficits.
The study has some limitations. Causality between the variables is not possible due to the cross-sectional design of the study. The number of people in this study is relatively small, making some of the commonly reported risk factors in the literature not associated with CAN in the univariate analysis. For ethical reasons, the use of medications was not discontinued or altered. As reported in the study, participants were on various medications that may influence the study’s findings. For example, metformin has shown improved ANS balance in type 2DM [43]; thus, the current study’s results need to be interpreted with caution. Furthermore, due to the variety of medications used by the participants, it was difficult to investigate these medications’ influence. Future studies should include a larger sample and control medications when possible.
Conclusion
The study results showed a moderate positive correlation between resting SBP and CAN and a moderate negative correlation between VO2peak and CAN in people with type 2DM. Both factors were independent predictors of CAN in people with type 2DM. This may indicate that control of SBP and improvement of CRF has a major contribution to preventing or reducing CAN in people with type 2DM. Future cross-sectional longitudinal studies should investigate if the management of these two factors reduced CAN among these people.
Availability of the data and materials
The data analyzed for this study is available from the author upon reasonable request.
Abbreviations
- ANS:
-
Autonomic nervous system
- ACE:
-
Angiotensin-converting enzyme
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- Ca:
-
Calcium
- CAN:
-
Cardiovascular autonomic neuropathy
- CRF:
-
Cardiorespiratory fitness
- CVD:
-
Cardiovascular disease
- COPD:
-
Chronic obstructive pulmonary disease
- DM:
-
Diabetes mellitus
- ECG:
-
Electrocardiograph
- ETT:
-
Exercise tolerance test
- HDL:
-
High-density lipoprotein
- HR:
-
Heart rate
- HOMA:
-
Homeostasis model assessment
- LDL:
-
Low-density lipoprotein
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- SPSS:
-
Statistical Package for Social Sciences
References
Organization WH (1999) Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. World health organization, Geneva https://apps.who.int/iris/handle/10665/66040. Accessed 12 Dec 2020
Todkar SS (2016) Diabetes mellitus the’Silent Killer’of mankind: an overview on the eve of upcoming World Health Day! J Med Allied Sci 6(1):39. https://doi.org/10.5455/jmas.214333
Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94(3):311–321. https://doi.org/10.1016/j.diabres.2011.10.029
Dokken BB (2008) The pathophysiology of cardiovascular disease and diabetes: beyond blood pressure and lipids. Diabetes Spectr 21(3):160–165. https://doi.org/10.2337/diaspect.21.3.160
Leon BM, Maddox TM (2015) Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes 6(13):1246–1258. https://doi.org/10.4239/wjd.v6.i13.1246
Kalofoutis C, Piperi C, Kalofoutis A, Harris F, Phoenix D, Singh J (2007) Type II diabetes mellitus and cardiovascular risk factors: current therapeutic approaches. Exp Clin Cardiol 12(1):17–28
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in non-diabetic subjects with and without prior myocardial infarction. N Engl J Med 339(4):229–234. https://doi.org/10.1056/NEJM199807233390404
Laakso M (2010) Cardiovascular disease in type 2 diabetes from population to man to mechanisms: the Kelly West Award Lecture 2008. Diabetes Care 33(2):442–449. https://doi.org/10.2337/dc09-0749
Matheus ASDM, Tannus LRM, Cobas RA, Palma CCS, Negrato CA, Gomes M d B (2013) Impact of diabetes on cardiovascular disease: an update. Int J Hypertens 2013:1–15. https://doi.org/10.1155/2013/653789
Silva DAS, Naghavi M, Duncan BB, Schmidt MI, de Souza M d FM, Malta DC (2019) Physical inactivity as risk factor for mortality by diabetes mellitus in Brazil in 1990, 2006, and 2016. Diabetol Metab Syndr 11(1):23. https://doi.org/10.1186/s13098-019-0419-9
Yun J-S, Park Y-M, Cha S-A, Ahn Y-B, Ko S-H (2018) Progression of cardiovascular autonomic neuropathy and cardiovascular disease in type 2 diabetes. Cardiovasc Diabetol 17(1):109. https://doi.org/10.1186/s12933-018-0752-6
Maser RE, Mitchell BD, Vinik AI, Freeman R (2003) The association between cardiovascular autonomic neuropathy and mortality in individuals with diabetes: a meta-analysis. Diabetes Care 26(6):1895–1901. https://doi.org/10.2337/diacare.26.6.1895
Fisher VL, Tahrani AA (2017) Cardiac autonomic neuropathy in patients with diabetes mellitus: current perspectives. Diabetes Metab Syndr Obes targets Ther 10:419. https://doi.org/10.2147/DMSO.S129797
Agashe S, Petak S (2018) Cardiac autonomic neuropathy in diabetes mellitus. Methodist Debakey Cardiovasc J 14(4):251–256. https://doi.org/10.14797/mdcj-14-4-251
Rolim LC, Sá JR, Chacra AR, Dib SA (2008) Diabetic cardiovascular autonomic neuropathy: risk factors, clinical impact and early diagnosis. Arq Bras Cardiol 90(4):e24–e31. https://doi.org/10.1590/s0066-782x2008000400014
Ewing DJ, Martyn CN, Young RJ, Clarke BF (1985) The value of cardiovascular autonomic function tests: 10 years experience in diabetes. Diabetes Care 8(5):491–498. https://doi.org/10.2337/diacare.8.5.491
Hartwig MS, Cardoso SS, Hathaway DK, Gaber AO (1994) Reliability and validity of cardiovascular and vasomotor autonomic function tests. Diabetes Care 17(12):1433–1440. https://doi.org/10.2337/diacare.17.12.1433
Jun JE, Lee S-E, Choi MS, Park SW, Hwang Y-C, Kim JH (2019) Clinical factors associated with the recovery of cardiovascular autonomic neuropathy in patients with type 2 diabetes mellitus. Cardiovasc Diabetol 18(1):29. https://doi.org/10.1186/s12933-019-0830-4
Low PA, Benrud-Larson LM, Sletten DM, Opfer-Gehrking TL, Weigand SD, O’Brien PC, Suarez GA, Dyck PJ (2004) Autonomic symptoms and diabetic neuropathy: a population-based study. Diabetes Care 27(12):2942–2947. https://doi.org/10.2337/diacare.27.12.2942
Valensi P, Paries J, Attali JR (2003) Cardiac autonomic neuropathy in diabetic patients: influence of diabetes duration, obesity, and microangiopathic complications—the French multicenter study. Metabolism. 52(7):815–820. https://doi.org/10.1016/s0026-0495(03)00095-7
Witte DR, Tesfaye S, Chaturvedi N, Eaton SE, Kempler P, Fuller JH (2005) Risk factors for cardiac autonomic neuropathy in type 1 diabetes mellitus. Diabetologia. 48(1):164–171. https://doi.org/10.1007/s00125-004-1617-y
Röhling M, Strom A, Bönhof G, Püttgen S, Bódis K, Müssig K, Szendrödi J, Markgraf D, Lehr S, Roden M, Ziegler D (2017) Differential patterns of impaired cardiorespiratory fitness and cardiac autonomic dysfunction in recently diagnosed type 1 and type 2 diabetes. Diabetes Care 40(2):246–252. https://doi.org/10.2337/dc16-1898
Franklin BA, Whaley MH, Howley ET, Balady GJ (2000) American College of Sports Medicine: ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins, Philadelphia
Osailan A, Metsios GS, Rouse PC, Ntoumanis N, Duda JL, Kitas GD, Van Zanten JJ (2016) Factors associated with parasympathetic activation following exercise in patients with rheumatoid arthritis: a cross-sectional study. BMC Cardiovasc Disord 16(1):1–8. https://doi.org/10.1186/s12872-016-0264-9
Kosinski C, Besson C, Amati F (2019) Exercise testing in individuals with diabetes, practical considerations for exercise physiologists. Front Physiol 10:1257. https://doi.org/10.3389/fphys.2019.01257
Myers J, Bellin D (2000) Ramp exercise protocols for clinical and cardiopulmonary exercise testing. Sports Med 30(1):23–29. https://doi.org/10.2165/00007256-200030010-00003
Radikova Z (2003) Assessment of insulin sensitivity/resistance in epidemiological studies. Endocr Regul 37(3):188–194
Didangelos T, Moralidis E, Karlafti E, Tziomalos K, Margaritidis C, Kontoninas Z, Hatzitolios A (2018) A comparative assessment of cardiovascular autonomic reflex testing and cardiac 123i-metaiodobenzylguanidine imaging in patients with type 1 diabetes mellitus without complications or cardiovascular risk factors. Int J Endocrinol 2018:1–7. https://doi.org/10.1155/2018/5607208
Spallone V, Maiello MR, Cicconetti E, Menzinger G (1997) Autonomic neuropathy and cardiovascular risk factors in insulin-dependent and non insulin-dependent diabetes. Diabetes Res Clin Pract 34(3):169–179. https://doi.org/10.1016/s0168-8227(96)01354-x
Hsu W-C, Yen AM-F, Liou H-H, Wang H-C, Chen TH-H (2009) Prevalence and risk factors of somatic and autonomic neuropathy in pre-diabetic and diabetic patients. Neuroepidemiology. 33(4):344–349. https://doi.org/10.1159/000254571
Zoppini G, Cacciatori V, Raimondo D, Gemma M, Trombetta M, Dauriz M, Brangani C, Pichiri I, Negri C, Stoico V, Bergamini C (2015) Prevalence of cardiovascular autonomic neuropathy in a cohort of patients with newly diagnosed type 2 diabetes: the Verona Newly Diagnosed Type 2 Diabetes Study (VNDS). Diabetes Care 38(8):1487–1493. https://doi.org/10.2337/dc15-0081
Pappachan JM, Sebastian J, Bino BC, Jayaprakash K, Vijayakumar K, Sujathan P, Adinegara LA (2008) Cardiac autonomic neuropathy in diabetes mellitus: prevalence, risk factors and utility of corrected QT interval in the ECG for its diagnosis. Postgrad Med J 84(990):205–210. https://doi.org/10.1136/pgmj.2007.064048
Kempler P, Tesfaye S, Chaturvedi N, Stevens LK, Webb DJ, Eaton S, Kerényi Z, Tamás G, Ward JD, Fuller JH, Eurodiab Iddm Complications Study Group (2002) Autonomic neuropathy is associated with increased cardiovascular risk factors: the EURODIAB IDDM Complications Study. Diabet Med 19(11):900–909. https://doi.org/10.1046/j.1464-5491.2002.00821.x
Singh JP, Larson MG, Tsuji H, Evans JC, O’Donnell CJ, Levy D (1998) Reduced heart rate variability and new-onset hypertension: insights into pathogenesis of hypertension: the Framingham Heart Study. Hypertension. 32(2):293–297. https://doi.org/10.1161/01.hyp.32.2.293
Julius S, Nesbitt S (1996) Sympathetic overactivity in hypertension: a moving target. Am J Hypertens 9(S4):113S–120S. https://doi.org/10.1016/0895-7061(96)00287-7
Ayad F, Belhadj M, Pariés J, Attali JR, Valensi P (2010) Association between cardiac autonomic neuropathy and hypertension and its potential influence on diabetic complications. Diabet Med 27(7):804–811. https://doi.org/10.1111/j.1464-5491.2010.03027.x
Huggett RJ, Scott EM, Gilbey SG, Stoker JB, Mackintosh AF, Mary DASG (2003) Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation. 108(25):3097–3101. https://doi.org/10.1161/01.CIR.0000103123.66264.FE
Johnson MD, Grignolo A, Kuhn CM, Schanberg SM (1983) Hypertension and cardiovascular hypertrophy during chronic catecholamine infusion in rats. Life Sci 33(2):169–180. https://doi.org/10.1016/0024-3205(83)90410-1
Giannattasio C, Mancia G (2002) Arterial distensibility in humans. Modulating mechanisms, alterations in diseases and effects of treatment. J Hypertens 20(10):1889–1899. https://doi.org/10.1097/00004872-200210000-00001
Dhumad MM, Hamdan FB, Khudhair MS, Al-Matubsi HY (2021) Correlation of staging and risk factors with cardiovascular autonomic neuropathy in patients with type II diabetes mellitus. Sci Rep 11(1):1–11. https://doi.org/10.1038/s41598-021-80962-w
Dimova R, Chakarova N, Grozeva G, Tankova T (2020) Evaluation of the relationship between cardiac autonomic function and glucose variability and HOMA-IR in prediabetes. Diab Vasc Dis Res 17(5):1479164120958619. https://doi.org/10.1177/1479164120958619
Bhati P, Shenoy S, Hussain ME (2018) Exercise training and cardiac autonomic function in type 2 diabetes mellitus: a systematic review. Diabetes Metab Syndr Clin Res Rev 12(1):69–78. https://doi.org/10.1016/j.dsx.2017.08.015
Röhling M, Strom A, Bönhof GJ, Roden M, Ziegler D (2017) Cardiorespiratory fitness and cardiac autonomic function in diabetes. Curr Diab Rep 17(12):125. https://doi.org/10.1007/s11892-017-0959-z
Hautala AJ, Kiviniemi AM, Tulppo MP (2009) Individual responses to aerobic exercise: the role of the autonomic nervous system. Neurosci Biobehav Rev 33(2):107–115. https://doi.org/10.1016/j.neubiorev.2008.04.009
Acknowledgements
The author would like to thank Dr Jet Veldhuizen Van Zanten, Prof. George Metsios, and Prof. George Kitas for their support and advice during the study. Also gratitude to the Russel Hall Hospital Research department for their advices and support. The author also would like to extend gratitude to the Deanship of Scientific research at Prince Sattam bin Abdulaziz University for providing the tools needed to complete this study.
Funding
The study did not receive funds from organization or private sectors.
Author information
Authors and Affiliations
Contributions
AO designed the study, conducted the testing, analyzed the data, and wrote the final draft of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the National Research Ethics Committee (IRA ID: 169234, Ref: 15/EM/0138) and all participants provided written informed consent before participation.
Consent for publication
Not applicable
Competing interests
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osailan, A. Cardiovascular autonomic neuropathy in people with type 2 diabetes mellitus; investigation of its association with classical cardiovascular risk factors using cardiovascular autonomic reflex tests: a cross-sectional study. Egypt Heart J 73, 44 (2021). https://doi.org/10.1186/s43044-021-00168-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-021-00168-3