Abstract
Background
This retrospective study aimed to compare the outcomes of day 3 double embryo transfer (DET) with single blastocyst transfer (SBT) during frozen embryo transfer (FET) cycles. A total of 999 women below the age of 38 years who underwent FET at Malaysia’s KL Fertility and Gynaecology Centre from January 2019 to December 2021 were analyzed. Patients with autologous eggs were recruited in the study. All the eggs were inseminated by intracytoplasmic sperm injection. The embryos were vitrified on day 3 cleavage-stage or blastocyst stage with Cryotop® method. The FET was performed following natural cycle (NC), modified natural cycle (m-NC), or hormone replacement therapy (HRT) cycles. The NC and m-NC groups received oral dydrogesterone for luteal phase support.
Results
There were no statistical differences in the rates of positive pregnancy, clinical pregnancy, and ongoing pregnancy between the two groups. However, implantation rates were significantly higher in the SBT group (50.1% versus 37.6%, p < 0.05). The day 3 DET group had significantly higher multiple pregnancy rates (28.7% versus 1.1%, p < 0.05). Subgroup analysis of embryo transfers performed following NC, m-NC, or HRT cycles showed similar results.
Conclusions
This study suggests that SBT is the better choice for embryo transfers as it had higher implantation rates and its pregnancy rates were similar to day 3 DET. The SBT also significantly reduced the incidence of multiple pregnancies without compromising pregnancy rates.
Similar content being viewed by others
Background
Although multiple embryo transfers can increase the likelihood of live births for women undergoing in vitro fertilization (IVF), multiple pregnancies, maternal complications, and neonatal complications can occur [1]. Women with multiple pregnancies are more likely to suffer miscarriages, fetal deaths, fetal malformations, and pregnancy complications than single pregnancies [2]. Multiple pregnancies have resulted from difficulty in selecting the most competent embryos on day 2/3 for transfer during IVF treatment, and hence transferring more than one embryo to ensure higher pregnancy rates [3].
The approach of blastocyst transfers has gained traction due to the reduced risk of multiple pregnancies and improved clinical outcomes than the use of embryos at earlier embryonic development stages (cleavage embryo transfer) [2, 4,5,6,7]. However, at the time of writing this paper, there are no guidelines or consensus on blastocyst and cleavage-stage transfers. There is a 2022 consensus on embryo transfer, but the publication was focused on technical aspects before, during, and after the procedure [8]. Several studies have examined the clinical outcomes of the blastocyst-stage transfer but a 2022 Cochrane review concluded that more evidence was needed to determine the impact of the stage of transfer on cumulative live births and pregnancy rates [9]. Our objective in the present study was to assess the success rates between day 3 double cleavage-stage embryo transfer (DET) and single blastocyst transfer (SBT) in women undergoing frozen embryo transfer (FET) with three different endometrial preparation methods, i.e., natural cycle (NC), modified natural cycle (m-NC), and hormone replacement therapy (HRT) in a single fertility center in Malaysia.
Methods
Subjects
This retrospective study included data from 999 female patients below the age of 38 years who underwent day 3 DET or SBT during FET cycles at the KL Fertility and Gynaecology Centre, Malaysia from January 2019 to December 2021. Patients with primary and secondary subfertility, male factors, tubal factors, polycystic ovary syndrome, and endometriosis were included. Exclusion criteria were gamete donation, embryo donation, preimplantation genetic testing, assisted hatching, and cases with incomplete information such as overseas patients or patients referred from other centers.
All the patients’ details were deidentified.
Culture of embryos
All the eggs were inseminated by intracytoplasmic sperm injection (ICSI) at 38 to 40 h after human chorionic gonadotrophin (hCG) administration. The day of insemination was defined as day 0. Embryos were examined for fertilization on day 1 (16–18 h post-ICSI), and subsequently examined on day 3 and day 5/6/7 for embryo grading. Two day 3 embryos of high-quality grade 1 or 2 were vitrified as per the center’s protocol, and the rest were cultured further to day 5/6/7. For the blastocyst stage, inner cell mass (ICM) and trophectoderm of grades BC, CB, or above were selected for vitrification. Embryo culture was performed at 37 °C, under 6% CO2, 5% O2, and 89% N2 using sequential culture media (COOK, Sydney IVF) in the benchtop incubator (Origio/Planer BT37).
Embryo grading
Grade 1 day 3 cleavage-stage embryo consisted of (1) 6–10 cells, (2) even-sized blastomeres, and (3) no fragmentation. Grade 2 day 3 cleavage-stage embryo consisted of (1) 6–8 cells, (2) slightly uneven-sized blastomeres, and (3) fragmentation < 10%. Grade 3 cleavage-stage embryo consisted of (1) < 6 cells, (2) uneven-sized blastomeres, and (3) 10–25% fragmentation. And Grade 4 cleavage-stage embryo consisted of (1) < 4 cells, (2) uneven-sized blastomeres, and (3) > 25% fragmentation. For day 3 DET, embryos with grade 1 and grade 2 were chosen for vitrification and transfer.
For day 5/6/7 blastocyst grading, inner cell mass, and trophectoderm were graded as A, B, C, and D respectively. Grade A is excellent, grade B is good, grade C is average and grade D is poor. Full blastocyst, expanded blastocyst, hatching blastocyst, or fully hatched blastocyst with ICM and trophectoderm of grades A, B, or C were selected for vitrification and embryo transfer.
Vitrification and thawing of cleavage-stage embryos and blastocysts
The cleavage-stage embryos and blastocysts were vitrified and thawed with Kitazato vitrification media and Kitazato thawing media (Kitazato Corporation, Japan) as described by Kuwayama (2007) [10] using the Cryotop method.
The cleavage-stage embryos were exposed to the equilibrium solution at room temperature for 12 min while the blastocyst was exposed for 15 min before being transferred into the vitrification solution for dehydration for 1 min. The embryos were subsequently loaded into the Cryotop. The carrier was directly plunged into liquid nitrogen.
The cleavage-stage embryo and blastocyst underwent the same thawing procedure. During thawing, the Cryotop is quickly immersed into the thawing solution (at 37 °C, for 1 min). Next, the embryos were transferred into dilution solution for 3 min followed by washing solution 1 (for 5 min) and washing solution 2 (for 1 min). Finally, the embryos were transferred to the blastocyst medium (COOK, Sydney IVF) for further culture until embryo transfer.
Frozen embryo transfer
For endometrial preparation, the endometrium was adjusted to the cleavage stage or the transfer window of blastocysts.
The FET was performed following natural cycle (NC), modified natural cycle (m-NC), or hormone replacement therapy (HRT) cycles. Patients who underwent NC cycles were scanned at day 2–3 menses to exclude cysts or prevailing corpus luteum from the previous cycle. Transvaginal ultrasound scans were carried out again on days 10–12 to determine the size of the dominant follicle. Once the dominant follicle attained a size of 16 mm or above, daily self-testing of urine luteinizing hormone (LH) was done to ascertain the timing of ovulation. Embryo transfers were carried out 4 or 6 days after a positive LH test. Oral dydrogesterone 10 mg twice daily was given as luteal phase support (LPS) until tested positive for pregnancy and extended to 12 weeks of gestation.
The initial monitoring for m-NC was similar to that for NC and patients were scanned by transvaginal ultrasound on days 10–12 of the menstrual cycle to determine the size of the dominant follicles. Ovulation was triggered with 5000 i.u hCG when the dominant follicle reached a mean diameter of 16 mm. Embryo transfers were carried out 4 or 6 days after ovulation induction. Oral dydrogesterone 10 mg twice daily was given as LPS.
Patients who underwent HRT cycles were scanned at day 2–3 menses and started on a fixed constant dose of oral estradiol valerate 6 mg daily (Progynova 2 mg × 3 daily) for 10–12 days. A transvaginal ultrasound was performed after 10–12 days of estradiol administration to measure endometrial thickness and confirm the absence of leading follicles. When the endometrial thickness reached 7 mm and above, vaginal micronized progesterone supplementation (Utrogestan 200 mg × 3 times daily) was commenced and FET was scheduled 4 or 6 days later. The hormonal treatment was continued until 12 weeks in the event of pregnancy, which was determined by serum measurement of hCG 10–12 days after transfer.
For women with cleavage embryos and blastocysts, two day 3 cleavage-stage embryos were transferred. If there was no pregnancy, a single blastocyst was used. For women who only had one day 3 cleavage-stage embryo and blastocysts, a single blastocyst was used first.
Outcome measures
Positive pregnancy was defined as elevated hCG concentration > 25 IU/L on day 10 or day 12 post-transfer respectively. The rate of positive pregnancy was calculated as the percentage of positive pregnancies over the total number of transfer cycles.
Clinical pregnancy was defined as evidenced by transvaginal ultrasound of an intrauterine sac at 5 weeks after transfer (with or without a fetal heart). The rate of clinical pregnancy was calculated as a percentage of clinical pregnancy over the total number of transfer cycles.
Implantation was defined as implanted embryos at six weeks. The rate of implantation was calculated as a percentage of implanted embryos at six weeks over the total of transferred embryos.
Multiple pregnancies were defined as the presence of two or more gestational sacs at 12 weeks. The rate of multiple pregnancies was calculated as a percentage of twin pregnancies over the total of clinical pregnancies.
Ongoing pregnancy was defined as a pregnancy that completed 12 weeks of gestation. The rate of ongoing pregnancy was calculated as a percentage of ongoing pregnancies over the total of transfer cycles.
Statistical methods
Collected data were analyzed using the SPSS version 26.0. A chi-square test was performed for categorical variables and one-way ANOVA was performed for continuous variables.
Results
Baseline characteristics
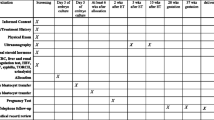
Of the 999 women included in the analysis, 274 were DET, and 725 were SBT. The mean ages [SD] of the women were similar in both groups (DET 33.2[2.9] years and SBT 32.9[2.9] years; p = 0183). Table 1 shows the baseline characteristics for DET versus SBT. In terms of FET cycles, 400 underwent NC, 243 underwent m-NC, and 356 underwent HRT cycles. Table 2 compares the overall success rates for double cleavage-stage transfer and single blastocyst transfer.
Clinical outcomes
Overall, there were no statistical differences in the rates of positive pregnancy, clinical pregnancy, and ongoing pregnancy between the day 3 DET and SBT groups (Table 1). Implantation rates were significantly higher in the SBT group (50.1% versus 37.6%, p < 0.05). The day 3 DET group had significantly higher multiple pregnancy rates (28.7% versus 1.1%, p < 0.05).
Table 3 shows the comparison of patients who underwent NC, m-NC, and HRT cycles either with double embryo transfer on day 3 or single blastocyst transfer.
Subgroup analysis of embryo transfers performed following NC, m-NC, or HRT cycles showed similar results for implantation rates in NC and HRT groups and for multiple pregnancies in all three groups (Table 4). The implantation rates were 34.9% for DET day 3 and 49.7% for SBT (P = 0.001) in NC; 40.4% for DET day 3 and 48.6% for SBT (P = 0.153) in m-NC; and 38.5% for DET day 3 and 52.0% for SBT (P = 0.004) in HRT cycles. The multiple pregnancies rates were 23.2% for DET day 3 and 1.4% for SBT (P = 0.000) in NC; 33.3% for DET day 3 and 0.0% for SBT (P = 0.000) in m-NC; and 30.9% for DET day 3 and 1.5% for SBT (P = 0.000) in HRT cycles.
Discussion
Our real-world study showed that implantation rates during FET were significantly higher with SBT than day 3 DET (50.1% versus 37.6%, p < 0.05), which was in line with evidence in the literature which showed SBT to have better implantation rate than day 3 DET [1, 11, 12]. This may be attributed to better-quality embryos if embryo cultures are maintained until day 5 [3, 4].
In our study, the SBT group had significantly lower multiple pregnancy rates than the day 3 DET group (1.1% versus 28.7%, p < 0.05). Other studies also demonstrated low multiple pregnancy rate with SBT [3, 13,14,15]. The patients included in these studies were younger than 36 years while our study included women up to the age of 38 years. Reducing the risk of multiple pregnancies is important due to its medical, psychological, social, and financial implications [14].
Our study did not demonstrate statistical differences in the rates of positive pregnancy, clinical pregnancy, and ongoing pregnancy between SBT and day 3 DET, indicating that positive pregnancy outcomes are possible with SBT [1, 4, 7, 16, 17]. According to Gardner et al. (2000) [17], a good-quality blastocyst can increase the rate of pregnancy by more than 60%. Rao et al. (2021) [1], in a similar study, found similar pregnancy rates for DET and day 5 SBT groups, but the day 6 SBT group had a significantly higher pregnancy rate than either of these groups. Our study did not differentiate the results for day 5 and day 6 groups, as a recent study found comparable pregnancy rates for SBT that were cryopreserved either on day 5 or day 6 [18].
Higher implantation rates and lower multiple pregnancy rates with SBT were seen in our study regardless of NC, m-NC, and HRT cycles. This may have important implications as patients who underwent HRT cycles are likely to have worse obstetric and perinatal outcomes [19]. Another study also showed no significant difference in live-birth clinical pregnancy rates between NC and m-NC cycles [20].
The key strengths of our study were that the data was current (2019–2021), a large number of patients (n = 999) were included, and the inclusion of women up to the age of 38 years. The mean age of women in our study was 33 years, which is higher than the ages of women in similar studies [1, 4]. However, the findings of our study may not be applicable to older women. Another advantage is that as a single-center study, the allocation of patients was done by all physicians following stringent center clinical protocol, and cultures and transfer of embryos were done using the same standard following embryology protocol, thus removing the effects of different culture media and techniques on the study results. This is important as culture media can affect neonatal births [6, 21].
The limitations of our study were its retrospective design and that comparisons between double cleavage transfer and single blastocyst transfer were not done for the same woman. As a retrospective study, patients were allocated to embryo transfer groups according to the physician and the preferences of the patients and were not randomly assigned. However, Stoop et al. (2011) highlighted that physicians and patients may be anxious with a randomized controlled study design [22]. In addition, information on maternal body mass index, smoking status, and alcohol consumption which could affect neonatal outcomes [21], and information on semen quality which could affect blastocyst formation [23] were not collected.
Conclusions
Our retrospective study showed that success rates for both day 3 DET and SBT were comparable. However, SBT is the better choice for embryo transfers than day 3 DET due to SBT’s higher implantation rate, comparable pregnancy rate, and significantly lower incidence of multiple pregnancies. These findings are useful for physicians when they counsel patients on expectations of outcomes and make well-informed decisions on the best treatment option available. However, data from prospective, randomized trials and the inclusion of older patients are needed to provide better guidance in clinical practice.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DET:
-
Double embryo transfer
- FET:
-
Frozen embryo transfer
- HRT:
-
Hormone replacement therapy
- m-NC:
-
Modified natural cycle
- NC:
-
Natural cycle
- SBT:
-
Single blastocyst transfer
References
Rao J, Qiu F, Tian S, Yu Y, Zhang Y, Gu Z, Cai Y, Jin F, Jin M (2021) Clinical outcomes for Day 3 double cleavage-stage embryo transfers versus Day 5 or 6 single blastocyst transfer in frozen-thawed cycles: a retrospective comparative analysis. J Int Med Res 49(12):3000605211062461. https://doi.org/10.1177/03000605211062461
Long X, Wang Y, Wu F, Li R, Chen L, Qian W, Qiao J (2020) Pregnancy outcomes of single/double blastocysts and cleavage embryo transfers: a retrospective cohort study of 24,422 frozen-thawed cycles. Reprod Sci 27(12):2271–2278. https://doi.org/10.1007/s43032-020-00247-x
Guerif F, Frapsauce C, Chavez C, Cadoret V, Royere D (2011) Treating women under 36 years old without top-quality embryos on day 2: a prospective study comparing double embryo transfer with single blastocyst transfer. Hum Reprod 26(4):775–781. https://doi.org/10.1093/humrep/der020
Hatırnaz Ş, Kanat Pektaş M (2017) Day 3 embryo transfer versus day 5 blastocyst transfers: A prospective randomized controlled trial. Turk J Obstet Gynecol 14(2):82–88. https://doi.org/10.4274/tjod.99076
He QH, Wang L, Liang LL, Zhang HL, Zhang CL, Li HS, Cui SH (2016) Clinical outcomes of frozen-thawed single blastocyst transfer in patients requiring whole embryo freezing. Syst Biol Reprod Med 62(2):133–138. https://doi.org/10.3109/19396368.2015.1128991
Park DS, Kim JW, Eum JH, Lee WS, Yoon TK, Lyu SW (2020) Clinical and pregnancy outcomes of double and single blastocyst transfers related with morphological grades in vitrified-warmed embryo transfer. Taiwan J Obstet Gynecol 59(3):398–402. https://doi.org/10.1016/j.tjog.2020.03.011
Zander-Fox DL, Tremellen K, Lane M (2011) Single blastocyst embryo transfer maintains comparable pregnancy rates to double cleavage-stage embryo transfer but results in healthier pregnancy outcomes. Aust NZ J Obstet Gynaecol 51(5):406–410. https://doi.org/10.1111/j.1479-828X.2011.01324.x
D'Angelo A, Panayotidis C, Alteri A, Mcheik S, Veleva Z (2022) Evidence and consensus on technical aspects of embryo transfer. Hum Reprod Open (4):hoac038. https://doi.org/10.1093/hropen/hoac038
Glujovsky D, Quinteiro Retamar AM, Alvarez Sedo CR, Ciapponi A, Cornelisse S, Blake D (2022) Cleavage-stage versus blastocyst-stage embryo transfer in assisted reproductive technology. Cochrane Database of Syst Rev Issue 5:CD002118. https://doi.org/10.1002/14651858.CD002118.pub6
Kuwayama M (2007) Highly efficient vitrification for cryopreservation of human oocytes and embryos: the Cryotop method. Theriogenology 67(1):73–80. https://doi.org/10.1016/j.theriogenology.2006.09.014
Guo J, Zeng Z, Li M, Huang J, Peng J, Wang M, Liang X, Zeng H (2021) Clinical outcomes after single-versus double-embryo transfers in women with adenomyosis: a retrospective study. Arch Gynecol Obstet 304(1):263–270. https://doi.org/10.1007/s00404-020-05924-5
Zhang X, Gao Y, Liu W, Liu J, Wu L, Xiong S, Zhu J, Han W, Wang J, Hao X, Han S, Huang G (2021) Frozen blastocyst embryo transfer vs. frozen cleavage-stage embryo transfer in couples with recurrent implantation failure: a cohort study. Hum Fertil (Camb) 24(4):284–289. https://doi.org/10.1080/14647273.2019.1633021
Abuzeid OM, Deanna J, Abdelaziz A, Joseph SK, Abuzeid YM, Salem WH, Ashraf M, Abuzeid MI (2017) The impact of single versus double blastocyst transfer on pregnancy outcomes: a prospective, randomized control trial. Facts Views Vis Obgyn 9(4):195–206
Kahraman S, Duzguner INB, Duzguner S, Sahin Y, Sen C (2021) Incidence of multiple births in relation to current regulations in Turkey regarding embryo transfer. BMC Pregnancy Childbirth 21(1):117. https://doi.org/10.1186/s12884-021-03616-9
Khalaf Y, El-Toukhy T, Coomarasamy A, Kamal A, Bolton V, Braude P (2008) Selective single blastocyst transfer reduces the multiple pregnancy rate and increases pregnancy rates: a pre- and postintervention study. BJOG 115(3):385–390. https://doi.org/10.1111/j.1471-0528.2007.01584.x
De Croo I, Colman R, De Sutter P, Stoop D, Tilleman K (2022, 2022) No difference in cumulative live birth rates between cleavage versus blastocyst transfer in patients with four or fewer zygotes: Results from a retrospective study. Hum Reprod Open (3):hoac031. https://doi.org/10.1093/hropen/hoac031
Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB (2000) Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril 73(6):1155–1158. https://doi.org/10.1016/s0015-0282(00)00518-5
Wu TF, Chen MJ, Lee MS, Huang CC, Ho ST, Cheng EH, Lee TH (2023) Comparison of clinical outcome between day 5 and day 6 single blastocyst transfers in cycles undergoing preimplantation genetic testing for aneuploidy. Taiwan J Obstet Gynecol 62(3):429–433. https://doi.org/10.1016/j.tjog.2023.03.005
Busnelli A, Schirripa I, Fedele F, Bulfoni A, Levi-Setti PE (2022) Obstetric and perinatal outcomes following programmed compared to natural frozen-thawed embryo transfer cycles: a systematic review and meta-analysis. Hum Reprod 37(7):1619–1641. https://doi.org/10.1093/humrep/deac073
Kadour-Peero E, Feferkorn I, Bellemare V, Arab S, Buckett W (2022) A comparison of frozen-thawed embryo transfer protocols in 2920 single-blastocyst transfers. Arch Gynecol Obstet 306(3):887–892. https://doi.org/10.1007/s00404-022-06588-z
Vergouw CG, Kostelijk EH, Doejaaren E, Hompes PG, Lambalk CB, Schats R (2012) The influence of the type of embryo culture medium on neonatal birthweight after single embryo transfer in IVF. Hum Reprod 27(9):2619–2626. https://doi.org/10.1093/humrep/des252
Stoop D, Van Landuyt L, Van den Abbeel E, Camus M, Verheyen G, Devroey P (2011) Should a single blastocyst transfer policy be a clinical decision or should it depend on the embryological evaluation on day 3? Reprod Biol Endocrinol 9:60. https://doi.org/10.1186/1477-7827-9-60
Xue X, Li W, Li M (2023) Optimal number of high-quality cleavage-stage embryos for extended culture to blastocyst-stage for transfer in women 38 years and older. Gynecol Endocrinol 39(1):2181642. https://doi.org/10.1080/09513590.2023.2181642
Acknowledgements
We thank the clinical, nursing, and embryology teams of KL Fertility Centre for their contributions to this study. We also thank Anne John Michael for medical writing assistance.
Funding
The authors did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors for the conduct of the study. The medical writing support was sponsored by Firstline Pharmaceuticals Sdn Bhd.
Author information
Authors and Affiliations
Contributions
LYH was the main author responsible for the research and writing of the paper. SPK was responsible for data collection and PN was responsible for reviewing and revising the paper. All authors read and approved the final manuscript.
Authors’ information
Dr. Yun-Hsuen Lim is a Fertility Specialist and consultant in Obstetrics & Gynaecology at KL Fertility Centre. Dr. Lim qualified as a fellow from the Royal College of O&G, UK, and with a Master’s degree from Universiti Kebangsaan Malaysia. She was a Senior Lecturer at the Department of Obstetrics & Gynaecology at Universiti Kebangsaan Malaysia and a Clinical Associate Professor at the University Tunku Abdul Rahman Malaysia.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No informed consent was required because of the retrospective design of the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lim, YH., Sim, P.K. & Nadkarni, P. A retrospective comparative study of double cleavage-stage embryo transfer versus single blastocyst in frozen-thawed cycles. Middle East Fertil Soc J 29, 17 (2024). https://doi.org/10.1186/s43043-024-00177-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-024-00177-7