Abstract
Background
Triggering final oocyte maturation is a pivotal step in modern patient-tailored IVF/ICSI treatment, securing the optimal number of mature oocytes retrieved without compromising fertilization, embryo development, and live birth. Several factors need to be considered when deciding the time of the trigger: the size of the leading follicles, distribution of the follicular cohort, the duration of stimulation, the protocol used for stimulation, and ovarian response status.
Main body
The current narrative review aims to appraise all available evidence for determining the proper time for inducing final oocyte maturation following IVF treatment. Moreover, it discusses the impact of the stimulation protocol, follicular size, and magnitude of ovarian response on choosing the proper timing for trigger. Comprehensive literature search of all available articles and relevant articles studying the criteria for timing of final oocyte maturation trigger in IVF/ICSI cycles were included in this review. It was found that leading follicles size of 16–22 mm is associated with the optimum oocyte maturation ratio, size of the remaining cohort of follicles should be ≥ 14 mm, 10–12 days of minimum length of stimulation should be auspicated in normal responders before trigger, and the timing of trigger administration should not depend solely on hormonal levels.
Conclusion
In conclusion, the timing of triggering of final oocyte maturation in ICSI cycles should be individualized on a case-by-case basis.
Similar content being viewed by others
Background
The timing of the trigger is an essential part of the successful assisted reproductive technology (ART) cycle. Trigger timing is tailored to retrieve a high proportion of mature and competent oocytes from the available follicular cohort [1]. Nevertheless, limited evidence is available regarding trigger time in different stimulation protocols. In clinical practice, the time of triggering administration mostly depends on the extent of response and follicle size in different protocols [2]. A comprehensive knowledge about pharmacokinetics and pharmacodynamics of the triggering agents is important for answering the following questions: when to end the follicular phase, the ideal triggering agent to be used, its ideal dose, optimal timing of the oocyte retrieval [3, 4].
This review is a comprehensive search of literature regarding the proper timing of administration of the triggering agent in different stimulation protocols and in different patterns of ovarian response to ovarian stimulation.
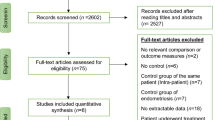
Comprehensive literature search of all available articles published in English on PubMed and Google Scholar libraries were searched independently from inception till January 2022 using the terms “final oocyte maturation,” “trigger,” “criteria,” “follicle size,” “stimulation phase length,” “delaying trigger,” “human chorionic gonadotropin,” and “agonist trigger.” Articles which were found to be relevant and studying the criteria for timing of final oocyte maturation trigger in IVF/ICSI cycles were included in this narrative literature review.
Main text
Ovulation trigger in ICSI cycles vs. natural cycles
Stimulated cycles differ from natural cycles in different aspects including supraphysiological follicular and luteal phase steroid levels due to multifollicular development, altered hypothalamic response due to the use of GnRH analogues, and low levels of endogenous gonadotropins during the luteal phase [1]. Moreover, the follicular growth rate is greater during ovarian stimulation cycles (1.69 ± 0.03 mm/day) compared to natural cycles (1.42 ± 0.05 mm/day), and the interval from dominant follicle selection to ovulation was found to be shorter during stimulated cycles (5.08 ± 0.07 days) compared to natural cycles (7.16 ± 0.23 days) [5].
A successful triggering should guarantee an LH exposure adequate for the resumption of meiosis, cytoplasmic maturation, and oocyte competence in harmony with a timely receptive endometrium [6,7,8]. Optimal triggering means “good yield with minimal or no complications” [9].
Factors influencing the timing of the trigger: when to end the follicular phase?
Timing of the trigger in ICSI cycles has an obvious effect on oocyte competence and endometrium receptivity [10]. Many factors have been studied for the determination of proper timing of trigger administration in ICSI cycles; they include follicle size, serum estradiol (E2) and progesterone levels, peak E2 per follicle, and previous response to ovarian stimulation (COS).
The most important factors influencing the choice of timing of trigger administration in ICSI cycles will be discussed in the current review.
Stimulation Phase Length (SPL)
The duration of gonadotropin stimulation is likely related to oocyte competence and endometrial readiness. Short and long stimulation could compromise ART cycle success [11,12,13,14,15]. In long agonist protocol, there is no clear indication that the duration of stimulation is associated with poor outcome [16,17,18].
Adding to the complexity of the situation are differential growth patterns of folliculogenesis in poor and normal responders [19,20,21].
In antagonist protocol, however, a short stimulation phase is associated with poor outcome only in normal responders. Conversely, in low responders, the short stimulation phase was not reported as a disadvantage [22].
A novel concept of “Term Oocyte Maturation” (TOM) has been recently proposed, referring to a minimal essential time to reach oocyte developmental competence [23]. TOM duration of 14 or 15 days could be a safe limit for oocyte competence, just like term pregnancy does for the wellbeing of a child. TOM tends to be shorter in stimulated cycles than in natural cycles due to faster follicular growth rate, higher FSH, and more mural/cumulus granulosa. Interestingly in some studies, deliberately delaying of trigger was not associated with an adverse outcome.
Table 1 displays the main characteristics of studies evaluating the effect of stimulation phase length on ICSI outcomes.
In conclusion, the impact of stimulation phase length on ICSI outcomes could be summarized:
-
1)
A minimum duration of ovarian stimulation is required for oocyte maturation before triggering ovulation (term oocyte maturation).
-
2)
From the best available evidence, a duration of 10–12 days of ovarian stimulation (OS) in normal responder women has been shown to be associated with better success outcomes.
-
3)
Duration of stimulation may have different impacts on women with extremes of ovarian response (hyper and poor responders).
-
4)
Prolongation of ovarian stimulation days to retrieve more oocytes appears to be more beneficial in agonist cycles rather than cycles stimulated with the antagonist protocol.
Sizes of the growing cohort of follicles
Timing of the trigger has been, for more than 3 decades, at least 3 follicles with a diameter of 17 mm or more [28,29,30,31].
Table 2 summarizes the main characteristics of the important studies correlating follicular size and several IVF success parameters.
Size of the leading follicle(s) on the day of the trigger
Determination of the follicle size essential for trigger is an important step in COS [37]. Vaginal ultrasound is used during (COS) to monitor follicles of different sizes that grow at different rates, thus adding to the complexity of evaluating their competence [38]. Most specialists tend to agree that oocytes are mainly aspirated from large follicles [28].
This is based on the concept that the cumulus oocyte complex is dissociated easily from the wall of “large follicles” under the effect of hyaluronidase expressed by the hCG trigger [39,40,41,42,43].
Despite this, there is no universal agreement on the minimum follicular size required to obtain a competent oocyte. The cutoff for obtaining a mature M2 oocyte is 16 mm in one view [31], and follicles smaller than 12 mm produce varying stages of oocyte immaturity [39, 44, 45]. Follicles above 22 mm often contain “post-mature” oocytes [31] that demonstrate decreased fertilization rate and impaired developmental competence [46]. To obtain a mature oocyte, an 18-mm cut-off was proposed by some authors [45, 47], 16 mm by others [48]. According to some publications [49, 50], follicles below 14-mm diameter do not contain MII oocytes, both in normal and polycystic ovaries. Moreover, while Dubey et al. [30] observed comparable fertilization rates in oocytes from 16- to 22-mm follicles to those from 22- to 26-mm follicles, Ectors et al. [31] found that follicles of 16–23 mm on the day of oocyte retrieval had higher fertilization rates than those > 23 mm. However, the percentage of good-scored oocytes was demonstrated to increase from 55.4% of follicle size of 16–23 mm to 64.6% of follicles > 23 mm. Knopman et al. tried to find an answer to the question “is bigger better?” [35]. It was found that delaying ovulation trigger to advance follicular growth does not appear to improve IVF outcomes. Indeed, those patients with 2 lead follicles ≥ 20 mm had a reduced (although non-significant) live birth rate (LBR). Although larger follicles are presumed to yield a higher quantity of mature oocytes and subsequently a greater number of resultant embryos, this study suggested that this hypothesis could be flawed as those women with follicles ≥ 20 mm had the lowest (p = 0.03) MII oocytes number amongst all women in the study. Moreover, they reported also the lowest 2PN zygotes and blastocyst numbers (although non-significant). Hence, the authors concluded that extension of ovarian stimulation to achieve marked follicular growth should not be done as it was not associated with improved outcomes. Similarly, it was found that a follicular size of 16 mm or more on OPU day is the best predictor of the fertilization potential of oocytes, even superior to the morphological appearance of COC [30]. This finding was also supported by another large study that found that oocytes retrieved from follicles above 18 mm have the best fertilization potential [45]. It can be concluded that follicles 16–22 mm in diameter are associated with the highest chance to retrieve mature oocytes [51], best fertilization protentional, and embryo developmental competence [31, 45].
Size of the cohort of the growing follicles on the day of trigger
The mechanism underlying the individual response of antral follicles to exogenous gonadotropin has not yet been clearly determined [52, 53]. However, it is known that early antral follicles do not necessarily grow coordinately in response to exogenous gonadotropins to reach simultaneous functional and morphologic maturation and that not necessarily all the FSH responding follicles have enough LH receptors to respond to the maturation signal induced by hCG [54, 55].
Moreover, in GnRH antagonist cycles, a physiological increase in the FSH level during the luteal-follicular transition phase provokes a heterogeneous follicular development leading to a slightly lower maturation rate when compared to agonist cycles. During the early follicular phase, early antral follicles present noticeable size heterogeneities that may be amplified during COS [56].
Thus, multifollicular growth may result in heterogeneous size of follicles and variable growth rate and also may cause secondary and tertiary cohorts [57,58,59].
The follicular size associated with the greatest chance of oocyte yield was studied by Hu et al. [10]. They categorized women treated with antagonist cycles by the proportion of 17 mm/10 mm follicles ratio on the day of trigger, as low (30% ≥ 17 mm), middle (30–60% ≥ 17 mm), or high proportion (> 60% ≥ 17 mm). Oocyte maturation rate in the middle- and high-proportion groups was higher than that in the low-proportion group. Implantation rate, pregnancy rate, and LBR were significantly higher in the high-proportion group compared with the low- and middle-proportion groups.
Another retrospective analysis was conducted by Abbara et al. [33]; they found that follicles with a mean diameter of 12–19 mm have the greatest odds of containing mature oocytes and this finding was noticed with both hCG and GnRH-agonist triggers.
A recent prospective study was conducted by Mohr-Sasson et al. [32] to assess the correlation between follicular size and oocyte and embryo quality. Before oocyte pickup, follicles were measured and divided into three groups according to maximum dimensions: large ≥ 16 mm, medium 13–15 mm, and small < 13 mm. Oocytes were obtained during aspiration from 76.3%, 70.3%, and 55.6% of the large, medium, and small follicle groups, respectively (the difference between medium and large groups was not significant). The mature oocyte (metaphase II) rate was significantly higher in the large (P = 0.001) and medium (P = 0.01) compared with the small follicle group. However, no differences were observed in fertilization or top-quality embryo (TQE) rates among mature oocytes regardless of the size of the follicle from which they originated. They reported also that triggering mode (hCG, GnRH agonist, or dual trigger) did not influence oocyte recovery rate in the different follicle size groups.
In conclusion, it appears that the size of follicles (both leading follicles and remaining follicular cohort) at the time of ovulation trigger can influence the likelihood that LH-like exposure can induce oocyte maturation. Most reproductive IVF centers administer the bolus trigger when two to three lead follicles are 17 to 18 mm in diameter provided that follicles grow as a tight representative cohort behind the lead follicle.
In the view of the best available evidence [60, 61], the European Society of Human Reproduction and Embryology (ESHRE) (2020) recommendations about the timing of trigger [62] are as follows: “Most often, final oocyte maturation is triggered at sizes of several of the leading follicles between 16–22 mm as data on specific follicle sizes that are most likely to yield an mature oocyte have predominantly been generated on the day of oocyte retrieval, at which time follicles of 16 to 22 mm are thought to be most likely to yield oocytes” [63].
Hormonal levels as determinants for the timing of trigger
Serum E2 level on the day of trigger administration
Serum estradiol levels during ovarian stimulation greatly vary depending on the size of the growing follicular cohort, the distribution of follicles between different size classes within the growing cohort, and the endocrine situation of the patient and the endocrine milieu of the stimulation cycle [62].
Several observational studies have been conducted aiming to find an association between outcomes of oocyte retrieval in IVF/ICSI cycles and estradiol levels on the day of trigger administration; some studies tried to correlate the estradiol levels (pg/mL) on the day of trigger [64,65,66] and other studies the effect of estradiol/follicle and estradiol/oocyte ratio as a parameter for triggering ovulation [67, 68].
To the best of our knowledge, there are no interventional studies performed assessing the use of serum estradiol and/or estradiol/follicle as a marker for timing the final oocyte maturation trigger.
Therefore, the guidelines of ESHRE 2020 for ovarian stimulation in IVF/ICSI do not recommend the use of either estradiol level or estradiol/follicle ratio as the sole parameter for the timing of trigger in IVF/ICSI cycles [62].
Serum progesterone (P) level on the day of trigger administration
In spite of the wide use of GnRH analogs during COS for ICSI, a subtle pre-ovulatory rise in the serum progesterone concentration before trigger administration for final oocyte maturation still occurred in 5–30% of COS cycles [69,70,71]; this phenomenon has been called premature luteinization. It has been recently proposed that “premature luteinization” is not an appropriate term for this condition because premature serum P rise occurs when the serum LH concentration is low. Therefore, excess serum P is unlikely to be produced by the luteinization process and is more probably due to accumulation from a large number of follicles [72,73,74]. The impact of this “pre-ovulatory” progesterone rise on outcomes of IVF/ICSI remains inconclusive and controversial. The majority of studies have advocated that progesterone rise on the day of hCG trigger adversely affects pregnancy outcome [75,76,77] due to its harmful effect on the endometrium and implantation process [78, 79] or affecting the quality of the developing oocytes and embryos [80, 81]. An interesting study reported significantly lower LBRs in patients with both low (≤ 0.05 ng/mL) and high (≥ 1.5 ng/mL) progesterone levels on the day of hCG trigger [82]. Nevertheless, other studies showed that progesterone rise does not appear to negatively affect IVF outcomes [72, 83, 84].
A randomized controlled trial showed that if the progesterone level is higher than 1 ng/ml, delaying the administration of hCG by 24 h has no effect on the number of mature oocytes. If the progesterone level is ≤ 1 ng/ml and 30–50% of the follicles have diameters ≥ 18 mm, delaying oocyte maturation by 24 h is advised [85]. However, another RCT [86] describes that even in patients with normal progesterone level (< 1 ng/ml) stimulated with antagonist protocol, delaying trigger administration by 24 h is not beneficial in any success outcome parameters.
Therefore, there is no sufficient evidence to recommend the use of serum progesterone to determine the timing of trigger administration. However, there are no clear cut-off values for normal and elevated progesterone levels.
Impact of the stimulation protocol on the timing of trigger administration
The question of whether it is better to delay or put forward the time of trigger administration in the different protocols remains elusive [52].
GnRH agonist protocol
In agonist cycles, upon administration of gonadotrophins, follicles are recruited in a backdrop of pituitary suppression, producing a pool of relatively equivalent follicles [87, 88]. In contrast, patients undergoing antagonist protocol maintain pituitary function, whereby endogenous gonadotrophin stimulates a degree of follicular development, augmented with exogenous gonadotrophins. This may induce additional follicle development, resulting in a more heterogeneous cohort of follicles [88].
There is a general agreement that, in GnRH agonist cycles, prolongation of the stimulation phase does not seem to have a detrimental effect on outcomes of IVF/ICSI.
A well-designed RCT by Mochtar et al. [61] investigated the effect of follicular diameter size on ongoing pregnancy rates (OPR) in agonist IVF/ICSI cycles. Women were randomized between timing oocyte collection when the leading follicle had a diameter of 22 mm or when the leading follicle had a diameter of 18 mm. In the 22-mm group, more women reached an ongoing pregnancy in comparison with the 18-mm group with a resulting relative risk (RR) of 1.6 (95% CI = 1.03–2.5). No statistically significant difference was reached for the secondary outcomes: clinical pregnancy rate (CPR) and LBR. The mean days of stimulation were, as predicted, more in the 22-mm group than in the 18-mm group (11.7 vs. 10.7). The mean number of oocytes retrieved and M-II oocytes was significantly higher in the 22-mm group; similarly, the mean number of top-quality embryos was found to be higher in the 22-mm group.
However, it has to be mentioned that to obtain optimal results in ICSI, the real paradigm might not be the stimulation regimens (mild or conventional) themselves but delaying oocyte collection to harvest more oocytes from the growing cohort, which then, in turn, leads to more high-quality embryos [61]. It is important to reiterate that better outcome with larger follicles could be restricted to long agonist protocol because delaying retrieval in antagonist could be associated with a poor outcome [14].
Similarly, another old study suggested that women would benefit from delayed administration of hCG in agonist cycles with proportionately more clinical pregnancies [89].
On the other hand, there are several studies showing no significant advantage of precise timing of hCG trigger in agonist cycles.
A RCT conducted to study different hCG criteria in patients undergoing IVF using the long GnRH-agonist protocol concluded that extending the duration of ovarian stimulation in a long GnRH agonist protocol by 2 days does not affect oocyte retrieval, fertilization, and pregnancy rates [90].
Chen et al. [60] performed a meta-analysis of 7 RCTs; in three trials, women were treated with agonist protocol and in the other four trials with antagonist protocol. Estradiol levels were significantly higher with either 24 h (p = 0.04) or 48 h (p < 0.00001) delay of hCG administration which reflects relatively more follicles come into maturation. The number of oocytes retrieved in the late hCG group was significantly higher than in the early hCG group (95% CI = 1.11–1.30, p < 0.00001), while CPRs and LBRs did not differ between the early and late hCG groups.
In conclusion, delaying the hCG trigger (1–2 days) in agonist ICSI cycles would result in better oocyte yield which in turn may have a positive impact on number of embryos and pregnancy rates; however, this could be associated with increased incidence of pre-ovulatory progesterone rise.
GnRH antagonist protocol
Since antagonist cycles do not involve pituitary desensitization, the ICSI cycle length is shorter than cycles treated with agonists [91].
It was reported that when GnRH antagonists are used, oocyte maturation is obtained at a lower follicle size than when a GnRH agonist is given in the classical “long” protocol [57].
It seems that, in antagonist ICSI cycles, the decision is usually made somewhat earlier than in agonist cycles [85]. In 2006, the Brussels GnRH antagonist Consensus Workshop Group stated that the optimal timing for triggering oocyte maturation when using a GnRH antagonist protocol needed to be explored further [92].
The criteria used for triggering the final maturation of oocytes in GnRH antagonist ICSI cycles are markedly variable between investigators. In the majority of studies, the trigger is administrated when at least 3 follicles ≥ 17 mm in diameter [91, 93,94,95,96]. Alternatively, triggering of final oocyte maturation is performed in the presence of 3 follicles with a maximum diameter of 18 mm [97] or in the presence of 1 follicle of 18 mm and 3 follicles of 15 mm [98]. It would therefore appear that follicles between 15 and 18 mm in diameter have good reproductive potential [99].
A RCT was conducted by Kolibianakis et al. [14] to assess the effect of prolongation of the follicular stimulation phase by 2 days in antagonist ICSI cycles. Patients were randomized to receive the bolus trigger of hCG either as soon as at least three follicles were 17 mm on ultrasound (early-hCG group) or 2 days later after this criterion was met (late-hCG group). A significantly lower OPR rate per retrieval and per transfer as well as a significantly lower ongoing implantation rate was present in the late-hCG as compared with the early-hCG group.
Morley et al. [87] performed a RCT to study the effect of precise timing vs. delayed trigger administration in antagonist cycles. All subjects were monitored daily from day 9 of stimulation until at least three follicles reached a diameter of ≥ 17 mm. Patients were then randomized to receive an injection of 10,000 units of hCG either on that day (group A) or delayed by either 24 h (group B) or 48 h (group C). The pregnancy rates per cycle were not statistically different among the groups.
Tremellen and Lane [99] conducted a retrospective analysis of 1642 IVF cycles to study the effect of advancing or delaying hCG administration by 1 day from the ideal time for the purpose of avoiding weekend oocyte pickups. “Ideal” timing of the hCG trigger administration for the collection of mature oocytes was the presence of two or more follicles ≥ 17 mm in diameter, with the majority of follicles being ≥ 14 mm.
Advancing or delaying trigger had no impact on ICSI outcome. The authors concluded that avoidance of weekend oocyte pickups had no detrimental effect on IVF pregnancy outcomes.
The effect of delaying hCG administration on endometrial development is still a debatable issue [14, 100]. Evidence described that endometrial biopsy taken on the day of oocyte pickup in women administered with hCG either as per normal protocol or with a 48-h delay showed that endometrial development was advanced by up to 3 days in the delayed hCG group [101].
In view of the available evidence, it could be concluded that in antagonist protocol, it seems that triggering oocyte maturation should be more precise (and usually earlier) than in agonist cycles; the timing of trigger should be when at least 3 follicles ≥ 17–18 mm and most of the remaining cohort of follicles are proportionately large follicle (≥ 14 mm) with consideration of appropriate estradiol level (100–400 pg/mL/ oocyte).
Progestin primed ovarian stimulation (PPOS) protocol
Since 2013, different progestins have been used as effective oral surrogates for preventing a premature luteinizing hormone (LH) surge in women undergoing COS. This protocol is called the progestin-primed ovarian stimulation (PPOS) protocol [100, 102, 103]. PPOS has proven effective for patients with a normal response, diminished ovarian reserve, polycystic ovarian syndrome (PCOS), and high body mass index (BMI) [104, 105].
Currently, there are no specific recommended criteria for timing of triggering final oocyte maturation in PPOS; however, the majority of studies investigating this new evolving protocol use dual trigger (a GnRH agonist and different doses of hCG) [106,107,108], hCG trigger alone [109], or agonist trigger alone [110]. Triggering of final oocyte maturation was performed in most studies when at least there are 3 follicles ≥ 17 mm and the majority of follicles are ≥ 14 mm [100, 102, 103, 106,107,108,109,110].
Influence of the state of predicted response to conventional ovarian stimulation (Normal, poor, or hyper-responders)
The question here “is there a need to also individualize the timing of trigger according to the predicted pattern of ovarian response?” or in other words, does the predicted response to ovarian stimulation affect the trigger timing? There are only a few studies that tried to find a valid answer to this question.
Poor responders
Individualized criteria for timing of ovulation trigger in poor responders are not yet established. Only very few studies tried to find out whether poor ovarian response could impact the timing of ovulation trigger in IVF/ICSI cycles.
Yang et al. [22] studied the effect of ovarian stimulation duration on different IVF population categories. In poor responder women, shorter and prolonged stimulation duration was found insignificant in terms of pregnancy rates.
In a similar study by Kahyaoglu et al. [111], a retrospective analysis of 3194 fresh IVF/ICSI cycles showed that in poor responders, MII oocyte number and fertilization rate were found to be higher with stimulation length between 9 and 12 days. With stimulation length > 12 days, the OPR was significantly decreased.
Aybar et al. [112] investigated if the stimulation phase length could affect IVF outcomes in women with poor ovarian response. They reported that the mean age in women with delayed response (≥ 9 days stimulation) was significantly higher compared to women with stimulation duration 6–8 days. CPR in delayed responders was significantly lower compared to others. However, when adjusted for age, the number of stimulation days did not have any significant effect on CPR and OPR.
Therefore, it was suggested that women with normal ovarian reserve and poor responder women cannot be judged in the same way during ovarian stimulation, considering early follicular recruitment, follicular growth rate, endometrial receptivity, and the stimulation durations. An optimal FSH stimulation duration together with follicular size criteria, serum estradiol, and progesterone levels are important parameters in determining trigger timing to balance between oocyte maturity and endometrial receptivity.
High responders (PCOS)
There is no absolute consensus on the best time for triggering ovulation in women with PCOS [52]. To the best of our knowledge, there are no interventional studies investigating specific criteria for the timing of final oocyte maturation for PCOS women. There are only a few studies investigating the effect of the duration of ovarian stimulation in PCOS women separately.
It has been hypothesized by some authors that it might be preferable, for example, to administer the trigger earlier in high responders than in normal and poor responders to avoid premature progesterone rise and consequently poor outcomes [2].
As aforementioned, Ryan et al. reported that stimulation longer than 13 days was not associated with decreased ART success for women with PCOS [24, 111].
These findings came in line with the results of a meta-analysis of 793 cycles with PCOS and 1116 matched controls which demonstrated that the duration of stimulation was 1.2 days longer in the PCOS group than in controls [113]. In another relevant study of Lin et al. [52], a new concept of proportion of dominant follicles (PDF) was investigated as a valid criterion for timing of trigger administration in PCOS women with different stimulation protocols. PDF was calculated by dividing the number of ≥ 18 mm follicles/number of ≥ 10 mm follicles on the hCG day. Cycles were divided into three sub-groups according to PDF in the GnRH agonist long protocol and the GnRH antagonist protocol, respectively: group A: PDF below 20%; group B: moderate PDF between 20 and 40%; group C: PDF of more than 40%. Top-quality embryos, implantation rate, and CPR were comparable among the three groups. However, there was a statistically significant increase in moderate and severe ovarian hyperstimulation syndrome (OHSS) with increased PDF. For GnRH antagonist cycles (347/718), the number of fertilized oocytes, available embryos, implantation rate, CPR, and moderate and severe OHSS were comparable between the three groups. From this study, it could be concluded that a PDF of 20 to 40% may be recommended in PCOS either in GnRH agonist long protocol or GnRH antagonist protocol in order to balance the risk of OHSS and the clinical pregnancy.
Conclusions
According to the currently available evidence, we could conclude that:
-
1.
The timing of triggering of final oocyte maturation in ICSI cycles (stimulation phase length) should be individualized on a case-by-case basis.
-
2.
The decision of administration of the trigger in ICSI cycles is multifactorial and many factors should be considered while making such decision as:
-
i.
Leading follicles size (16–22 mm) is associated with the optimum oocyte maturation ratio.
-
ii.
Size of the remaining cohort of follicles should be proportionally large follicles (≥ 14 mm).
-
iii.
The protocol used for ovarian stimulation:
-
a)
For GnRH agonist protocol: most of the available evidence suggested that prolongation of stimulation 24–48 h in agonist cycles would result in higher oocyte yield and more mature oocyte and in turn better outcomes.
-
b)
For GnRH antagonist protocol: according to the best knowledge; such a prolongation of stimulation beyond the precise timing (criteria) of trigger seems to have no added benefits in case of poor and high responders.
-
a)
-
i.
Availability of data and materials
Not applicable.
Abbreviations
- ARTs:
-
Assisted reproductive technologies
- CPR:
-
Clinical pregnancy rate
- COS:
-
Controlled ovarian stimulation
- COC:
-
Cumulus oocyte complex
- ESHRE:
-
European Society of Human Reproduction and Embryology
- GV:
-
Germinal vesicle
- IVF/ICSI:
-
In vitro fertilization/intracytoplasmic sperm injection
- LBR:
-
Live birth rate
- MI:
-
Metaphase I
- MII:
-
Metaphase II
- OPR:
-
Ongoing pregnancy rates
- OS:
-
Ovarian stimulation
- PCOS:
-
Polycystic ovarian syndrome
- PPOS:
-
Progestin primed ovarian stimulation
- PDF:
-
Proportion of dominant follicles
- RCT:
-
Randomized controlled trial
- RR:
-
Relative risk
- SPL:
-
Stimulation phase length
- TOM:
-
Term oocyte maturation
- TQE:
-
Top-quality embryos
References
Dosouto C, Haahr T, Humaidan P (2019) Advances in ovulation trigger strategies. Panminerva Med 61(1):42–51
Al-Azemi M, Kyrou D, Kolibianakis E, Humaidan P, Van Vaerenbergh I, Devroey P et al (2012) Elevated progesterone during ovarian stimulation for IVF. Reprod Biomed Online 24(4):381–388
Haahr T, Roque M, Esteves SC, Humaidan P (2017) GnRH agonist trigger and LH activity luteal phase support versus hCG trigger and conventional luteal phase support in fresh embryo transfer IVF/ICSI cycles-a systematic PRISMA review and meta-analysis. Front Endocrinol 8:116
Engmann L, Benadiva C, Humaidan P (2016) GnRH agonist trigger for the induction of oocyte maturation in GnRH antagonist IVF cycles: a SWOT analysis. Reprod Biomed Online 32(3):274–285
Baerwald AR, Walker RA, Pierson RA (2009) Growth rates of ovarian follicles during natural menstrual cycles, oral contraception cycles, and ovarian stimulation cycles. Fertil Steril 91(2):440–449
Voronina E, Wessel GM (2003) The regulation of oocyte maturation. Curr Top Dev Biol 58:53–110
Palomba S, Santagni S, La Sala GB (2015) Progesterone administration for luteal phase deficiency in human reproduction: an old or new issue? J Ovarian Res 8:77
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S (2011) Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril 96(2):344–348
Skorupskaite K, George JT, Anderson RA (2014) The kisspeptin-GnRH pathway in human reproductive health and disease. Hum Reprod Update 20(4):485–500
Hu X, Luo Y, Huang K, Li Y, Xu Y, Zhou C et al (2016) New perspectives on criteria for the determination of HCG trigger timing in GnRH antagonist cycles. Medicine 95(20):e3691
Depalo R, Lorusso F, Palmisano M, Bassi E, Totaro I, Vacca M et al (2009) Follicular growth and oocyte maturation in GnRH agonist and antagonist protocols for in vitro fertilisation and embryo transfer. Gynecol Endocrinol 25(5):328–334
Yoldemir T (2011) Does the duration of gonadotropin stimulation affect embryo quality on post-retrieval day 3? Gynecol Endocrinol 27(5):324–330
Tao T, Robichaud A, Nadeau S, Savoie R, Gallant B, Ouellette RJ (2006) Optimized hormonal stimulation is critical for production of viable embryos and establishment of subsequent implantation. J Assist Reprod Genet 23(1):23–28
Kolibianakis EM, Albano C, Camus M, Tournaye H, Van Steirteghem AC, Devroey P (2004) Prolongation of the follicular phase in in vitro fertilization results in a lower ongoing pregnancy rate in cycles stimulated with recombinant follicle-stimulating hormone and gonadotropin-releasing hormone antagonists. Fertil Steril 82(1):102–107
Huang CC, Lien YR, Chen HF, Chen MJ, Shieh CJ, Yao YL et al (2012) The duration of pre-ovulatory serum progesterone elevation before hCG administration affects the outcome of IVF/ICSI cycles. Hum Reprod 27(7):2036–2045
Martin JR, Mahutte NG, Arici A, Sakkas D (2006) Impact of duration and dose of gonadotrophins on IVF outcomes. Reprod Biomed Online 13(5):645–650
Chuang M, Zapantis A, Taylor M, Jindal SK, Neal-Perry GS, Lieman HJ et al (2010) Prolonged gonadotropin stimulation is associated with decreased ART success. J Assist Reprod Genet 27(12):711–717
Mardesic T, Mannaerts B, Abuzeid M, Levy M, Witjes H, Fauser BC et al (2014) Short follicular phase of stimulation following corifollitropin alfa or daily recombinant FSH treatment does not compromise clinical outcome: a retrospective analysis of the Engage trial. Reprod Biomed Online 28(4):462–468
Marci R, Caserta D, Dolo V, Tatone C, Pavan A, Moscarini M (2005) GnRH antagonist in IVF poor-responder patients: results of a randomized trial. Reprod Biomed Online 11(2):189–193
Pu D, Wu J, Liu J (2011) Comparisons of GnRH antagonist versus GnRH agonist protocol in poor ovarian responders undergoing IVF. Hum Reprod 26(10):2742–2749
Madani T, Ashrafi M, Yeganeh LM (2012) Comparison of different stimulation protocols efficacy in poor responders undergoing IVF: a retrospective study. Gynecol Endocrinol 28(2):102–105
Yang YC, Li YP, Pan SP, Chao KH, Chang CH, Yang JH et al (2019) The different impact of stimulation duration on oocyte maturation and pregnancy outcome in fresh cycles with GnRH antagonist protocol in poor responders and normal responders. Taiwan J Obstet Gynecol 58(4):471–476
Dozortsev DI, Pellicer A, Diamond MP (2020) Term oocyte maturation and term ovarian stimulation: impact on oocyte competence. Fertil Steril 114(2):221–222
Ryan A, Wang S, Alvero R, Polotsky AJ (2014) Prolonged gonadotropin stimulation for assisted reproductive technology cycles is associated with decreased pregnancy rates for all women except for women with polycystic ovary syndrome. J Assist Reprod Genet 31(7):837–842
Alport B, Case A, Lim H, Baerwald A (2011) Does the Ovarian Stimulation Phase Length Predict In vitro Fertilization Outcomes? Int J Fertil Steril 5(3):134–41. Epub 2011 Dec 22.
Purandare N, Emerson G, Kirkham C et al (2017) The duration of gonadotropin stimulation does not alter the clinical pregnancy rate in IVF or ICSI cycles. Ir J Med Sci 186;653–657. https://doi.org/10.1007/s11845-016-1526-3
Deepmala D, Jain K, Jain B (2019) Effect of stimulation phase length (SPL) on IVF/ICSI outcomes: a prospective study. Fertil Sci Res 6(2):133-139. https://doi.org/10.4103/fsr.fsr_15_19
Simonetti S, Veeck LL, Jones HW Jr (1985) Correlation of follicular fluid volume with oocyte morphology from follicles stimulated by human menopausal gonadotropin. Fertil Steril 44(2):177–180
Scott RT, Hofmann GE, Muasher SJ, Acosta AA, Kreiner DK, Rosenwaks Z (1989) Correlation of follicular diameter with oocyte recovery and maturity at the time of transvaginal follicular aspiration. J In Vitro Fert Embryo Transf 6(2):73–75
Dubey AK, Wang HA, Duffy P, Penzias AS (1995) The correlation between follicular measurements, oocyte morphology, and fertilization rates in an in vitro fertilization program. Fertil Steril 64(4):787–790
Ectors FJ, Vanderzwalmen P, Van Hoeck J, Nijs M, Verhaegen G, Delvigne A et al (1997) Relationship of human follicular diameter with oocyte fertilization and development after in-vitro fertilization or intracytoplasmic sperm injection. Hum Reprod 12(9):2002–2005
Mohr-Sasson A, Orvieto R, Blumenfeld S, Axelrod M, Mor-Hadar D, Grin L et al (2020) The association between follicle size and oocyte development as a function of final follicular maturation triggering. Reprod Biomed Online. 40:887–893
Abbara A, Vuong LN, Ho VNA, Clarke SA, Jeffers L, Comninos AN et al (2018) Follicle size on day of trigger most likely to yield a mature oocyte. Front Endocrinol 9:193
Orvieto R, Kirshenbaum M, Galiano V, Elkan-Miller T, Zilberberg E, Haas J, Nahum R (2020) Stop GnRH-Agonist Combined With Multiple-Dose GnRH-Antagonist Protocol for Patients With "Genuine" Poor Response Undergoing Controlled Ovarian Hyperstimulation for IVF. Front Endocrinol (Lausanne) 11:182. https://doi.org/10.3389/fendo.2020.00182.
Knopman JM, Grifo JA, Novetsky AP, Smith MB, Berkeley AS (2012) Is bigger better: the association between follicle size and livebirth rate following IVF?
Das M, Son WY, Buckett W, Tulandi T, Holzer H (2014) In-vitro maturation versus IVF with GnRH antagonist for women with polycystic ovary syndrome: treatment outcome and rates of ovarian hyperstimulation syndrome. Reprod Biomed Online 29(5):545–51. https://doi.org/10.1016/j.rbmo.2014.07.019. Epub 2014 Aug 12.
Wirleitner B, Okhowat J, Vištejnová L, Králíčková M, Karlíková M, Vanderzwalmen P et al (2018) Relationship between follicular volume and oocyte competence, blastocyst development and live-birth rate: optimal follicle size for oocyte retrieval. Ultrasound Obstet Gynecol 51(1):118–125
Miller KF, Goldberg JM, Falcone T (1996) Follicle size and implantation of embryos from in vitro fertilization. Obstet Gynecol 88(4):583–586
Scott RT, Hofmann GE, Muasher SJ, Acosta AA, Kreiner DK, Rosenwaks Z (1989) Correlation of follicular diameter with oocyte recovery and maturity at the time of transvaginal follicular aspiration. J In Vitro Fert Embryo Transf 6(2):73–75
Wittmaack FM, Kreger DO, Blasco L, Tureck RW, Mastroianni L Jr, Lessey BA (1994) Effect of follicular size on oocyte retrieval, fertilization, cleavage, and embryo quality in in vitro fertilization cycles: a 6-year data collection. Fertil Steril 62(6):1205–1210
Triwitayakorn A, Suwajanakorn S, Pruksananonda K, Sereepapong W, Ahnonkitpanit V (2003) Correlation between human follicular diameter and oocyte outcomes in an ICSI program. J Assist Reprod Genet 20(4):143–147
Suchanek E, Simunic V, Juretic D, Grizelj V (1994) Follicular fluid contents of hyaluronic acid, follicle-stimulating hormone and steroids relative to the success of in vitro fertilization of human oocytes. Fertil Steril 62(2):347–352
Oktay K, Briggs D, Gosden RG (1997) Ontogeny of follicle-stimulating hormone receptor gene expression in isolated human ovarian follicles. J Clin Endocrinol Metab 82(11):3748–3751
Bergh C, Broden H, Lundin K, Hamberger L (1998) Comparison of fertilization, cleavage and pregnancy rates of oocytes from large and small follicles. Hum Reprod 13(7):1912–1915
Rosen MP, Shen S, Dobson AT, Rinaudo PF, McCulloch CE, Cedars MI (2008) A quantitative assessment of follicle size on oocyte developmental competence. Fertil Steril 90(3):684–690
Clark L, Stanger J, Brinsmead M (1991) Prolonged follicle stimulation decreases pregnancy rates after in vitro fertilization. Fertil Steril 55(6):1192–1194
Mehri S, Levi Setti PE, Greco K, Sakkas D, Martinez G, Patrizio P (2014) Correlation between follicular diameters and flushing versus no flushing on oocyte maturity, fertilization rate and embryo quality. J Assist Reprod Genet 31(1):73–77
Shmorgun D, Hughes E, Mohide P, Roberts R (2010) Prospective cohort study of three- versus two-dimensional ultrasound for prediction of oocyte maturity. Fertil Steril 93(4):1333–1337
Teissier MP, Chable H, Paulhac S, Aubard Y (2000) Comparison of follicle steroidogenesis from normal and polycystic ovaries in women undergoing IVF: relationship between steroid concentrations, follicle size, oocyte quality and fecundability. Hum Reprod 15(12):2471–2477
Lee TF, Lee RK, Hwu YM, Chih YF, Tsai YC, Su JT (2010) Relationship of follicular size to the development of intracytoplasmic sperm injection-derived human embryos. Taiwan J Obstet Gynecol 49(3):302–305
Inaudi P, Germond M, Senn A, De Grandi P (1995) Timing of hCG administration in cycles stimulated for in vitro fertilization: specific impact of heterogeneous follicle sizes and steroid concentrations in plasma and follicle fluid on decision procedures. Gynecol Endocrinol 9(3):201–208
Lin HY, Li Y, Wang WJ, Qiu Q, Zhang QX, Li Y (2019) Role of the proportion of dominant follicles in patients with polycystic ovary syndrome undergoing in vitro fertilization-embryo transfer. Chin Med J 132(12):1448
Kahraman S, Cetinkaya CP, Cetinkaya M, Yelke H, Colakoglu YK, Aygun M et al (2017) The effect of follicle size and homogeneity of follicular development on the morphokinetics of human embryos. J Assist Reprod Genet 34(7):895–903
Devreker F, Pogonici E, De Maertelaer V, Revelard P, Van den Bergh M, Englert Y (1999) Selection of good embryos for transfer depends on embryo cohort size: implications for themild ovarian stimulation’debate. Hum Reprod 14(12):3002–3008
Opsahl M, Blauer K, Black S, Lincoln S, Thorsell L, Sherins R (2001) The number of embryos available for transfer predicts successful pregnancy outcome in women over 39 years with normal ovarian hormonal reserve testing. J Assist Reprod Genet 18(10):551–556
Fanchin R, Schonäuer LM, Cunha-Filho JS, Méndez Lozano DH, Frydman R (2005) Coordination of antral follicle growth: basis for innovative concepts of controlled ovarian hyperstimulation. Semin Reprod Med 23(4):354–62. https://doi.org/10.1055/s-2005-923393.
Nogueira D, Friedler S, Schachter M, Raziel A, Ron-El R, Smitz J (2006) Oocyte maturity and preimplantation development in relation to follicle diameter in gonadotropin-releasing hormone agonist or antagonist treatments. Fertil Steril 85(3):578–583
Depalo R, Lorusso F, Palmisano M, Bassi E, Totaro I, Vacca M et al (2009) Follicular growth and oocyte maturation in GnRH agonist and antagonist protocols for in vitro fertilisation and embryo transfer. Gynecol Endocrinol 25(5):328–334
Wiesak T (2002) Role of LH in controlled ovarian stimulation. Reprod Biol 2(3):215–227
Chen Y, Zhang Y, Hu M, Liu X, Qi H (2014) Timing of human chorionic gonadotropin (hCG) hormone administration in IVF/ICSI protocols using GnRH agonist or antagonists: a systematic review and meta-analysis. Gynecol Endocrinol 30(6):431–437
Mochtar MH, Custers IM, Koks CA, Bernardus RE, Verhoeve HR, Mol BW et al (2011) Timing oocyte collection in GnRH agonists down-regulated IVF and ICSI cycles: a randomized clinical trial. Hum Reprod 26(5):1091–1096
Ovarian Stimulation T, Bosch E, Broer S, Griesinger G, Grynberg M, Humaidan P, et al (2020) ESHRE guideline: ovarian stimulation for IVF/ICSI (dagger). Hum Reprod Open. 2020(2):hoaa009
Revelli A, Martiny G, Delle Piane L, Benedetto C, Rinaudo P, Tur-Kaspa I (2014) A critical review of bi-dimensional and three-dimensional ultrasound techniques to monitor follicle growth: do they help improving IVF outcome? Reprod Biol Endocrinol 12(1):107
Tao T, Robichaud A, Heudes R, Ouellette R (2013) Effects of estradiol levels and estradiol/follicle ratio on trigger day on the IVF pregnancy outcome. Fertil Steril 100(3):S262–S263
Melnick A, Murphy E, Khalifa A, Elias R, Rosenwaks Z (2014) Estradiol level as a parameter for optimal ovulation trigger day in IVF/ICSI cycles. Fertil Steril 102(3):e321–e322
Siddhartha N, Reddy NS, Pandurangi M, Tamizharasi M, Radha V, Kanimozhi K (2016) Correlation of serum estradiol level on the day of ovulation trigger with the reproductive outcome of intracytoplasmic sperm injection. J Hum Reprod Sci 9(1):23–27
Vaughan DA, Harrity C, Sills ES, Mocanu EV (2016) Serum estradiol: oocyte ratio as a predictor of reproductive outcome: an analysis of data from >9000 IVF cycles in the Republic of Ireland. J Assist Reprod Genet 33(4):481–488
Orvieto R, Zohav E, Scharf S, Rabinson J, Meltcer S, Anteby EY et al (2007) The influence of estradiol/follicle and estradiol/oocyte ratios on the outcome of controlled ovarian stimulation for in vitro fertilization. Gynecol Endocrinol 23(2):72–75
Melo M, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohí J (2006) The significance of premature luteinization in an oocyte-donation programme. Hum Reprod 21(6):1503–1507
Elnashar AM (2010) Progesterone rise on the day of HCG administration (premature luteinization) in IVF: an overdue update. J Assist Reprod Genet 27(4):149–155
Segal S, Glatstein I, McShane P, Hotamisligil S, Ezcurra D, Carson R (2009) Premature luteinization and in vitro fertilization outcome in gonadotropin/gonadotropin-releasing hormone antagonist cycles in women with polycystic ovary syndrome. Fertil Steril 91(5):1755–1759
Venetis C, Kolibianakis E, Papanikolaou E, Bontis J, Devroey P, Tarlatzis B (2007) Is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. Hum Reprod Update 13(4):343–355
Bosch E, Labarta E, Crespo J, Simon C, Remohi J, Jenkins J et al (2010) Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod 25(8):2092–2100
Kyrou D, Al-Azemi M, Papanikolaou E, Donoso P, Tziomalos K, Devroey P et al (2012) The relationship of premature progesterone rise with serum estradiol levels and number of follicles in GnRH antagonist/recombinant FSH-stimulated cycles. Eur J Obstet Gynecol Reprod Biol 162(2):165–168
Huang Y, Wang EY, Du QY, Xiong YJ, Guo XY, Yu YP et al (2015) Progesterone elevation on the day of human chorionic gonadotropin administration adversely affects the outcome of IVF with transferred embryos at different developmental stages. Reprod Biol Endocrinol. 13(1):1–10
Demir B, Kahyaoglu I, Guvenir A, Yerebasmaz N, Altinbas S, Dilbaz B et al (2016) Progesterone change in the late follicular phase affects pregnancy rates both agonist and antagonist protocols in normoresponders: a case-controlled study in ICSI cycles. Gynecol Endocrinol 32(5):361–365
Bu Z, Zhao F, Wang K, Guo Y, Su Y, Zhai J et al (2014) Serum progesterone elevation adversely affects cumulative live birth rate in different ovarian responders during in vitro fertilization and embryo transfer: a large retrospective study. PLoS ONE 9(6):e100011
Fanchin R, Righini C, Olivennes F, Ferreira AL, de Ziegler D, Frydman R (1997) Consequences of premature progesterone elevation on the outcome of in vitro fertilization: insights into a controversy. Fertil Steril 68(5):799–805
Bourgain C, Devroey P (2003) The endometrium in stimulated cycles for IVF. Hum Reprod Update 9(6):515–522
Papanikolaou EG, Kolibianakis EM, Pozzobon C, Tank P, Tournaye H, Bourgain C et al (2009) Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril 91(3):949–952
Huang B, Ren X, Wu L, Zhu L, Xu B, Li Y et al (2016) Elevated progesterone levels on the day of oocyte maturation may affect top quality embryo IVF cycles. PLoS ONE 11(1):e0145895
Santos-Ribeiro S, Polyzos N, Haentjens P, Smitz J, Camus M, Tournaye H et al (2014) Live birth rates after IVF are reduced by both low and high progesterone levels on the day of human chorionic gonadotrophin administration. Hum Reprod 29(8):1698–1705
Urman B, Alatas C, Aksoy S, Mercan R, Isiklar A, Balaban B (1999) Elevated serum progesterone level on the day of human chorionic gonadotropin administration does not adversely affect implantation rates after intracytoplasmic sperm injection and embryo transfer. Fertil Steril 72(6):975–979
Griesinger G, Mannaerts B, Andersen CY, Witjes H, Kolibianakis EM, Gordon K (2013) Progesterone elevation does not compromise pregnancy rates in high responders: a pooled analysis of in vitro fertilization patients treated with recombinant follicle-stimulating hormone/gonadotropin-releasing hormone antagonist in six trials. Fertil Steril. 100(6):1622–8. e3
Vandekerckhove F, Gerris J, Vansteelandt S, De Baerdemaeker A, Tilleman K, De Sutter P (2014) Delaying the oocyte maturation trigger by one day leads to a higher metaphase II oocyte yield in IVF/ICSI: a randomised controlled trial. Reprod Biol Endocrinol 12(1):1–9
Davar R, Naghshineh E, Neghab N (2017) The effect of 24 hours delay in oocyte maturation triggering in IVF/ICSI cycles with antagonist protocol and not-elevated progesterone: a randomized control trial. Int J Reprod BioMed 15(7):441
Morley L, Tang T, Yasmin E, Hamzeh R, Rutherford AJ, Balen AH (2012) Timing of human chorionic gonadotrophin (hCG) hormone administration in IVF protocols using GnRH antagonists: a randomized controlled trial. Hum Fertil 15(3):134–139
Fleming R (2002) Monitoring during gonadotrophin-releasing hormone antagonist protocols. Hum Fertil 5(1):G19–G27
Dimitry ES, Oskarsson T, Conaghan J, Margara R, Winston RM (1991) Beneficial effects of a 24 h delay in human chorionic gonadotrophin administration during in-vitro fertilization treatment cycles. Hum Reprod 6(7):944–946
Tan SL, Balen A, el Hussein E, Mills C, Campbell S, Yovich J et al (1992) A prospective randomized study of the optimum timing of human chorionic gonadotropin administration after pituitary desensitization in in vitro fertilization. Fertil Steril 57(6):1259–1264
Group EMEOS (2001) Comparable clinical outcome using the GnRH antagonist ganirelix or a long protocol of the GnRH agonist triptorelin for the prevention of premature LH surges in women undergoing ovarian stimulation. Hum Reprod 16(4):644–51
Tarlatzis B, Fauser B, Kolibianakis E, Diedrich K, Devroey P, Group BGACW (2006) GnRH antagonists in ovarian stimulation for IVF. Hum Reprod Update 12(4):333–40
Group EOS, Borm G, Mannaerts B (2000) Treatment with the gonadotrophin-releasing hormone antagonist ganirelix in women undergoing ovarian stimulation with recombinant follicle stimulating hormone is effective, safe and convenient: results of a controlled, randomized, multicentre trial. Hum Reprod 15(7):1490–1498
Group NAGS, Fluker M, Grifo J, Leader A, Levy M, Meldrum D, Muasher SJ et al (2001) Efficacy and safety of ganirelix acetate versus leuprolide acetate in women undergoing controlled ovarian hyperstimulation. Fertil Steril. 75:38–45
Kolibianakis E, Bourgain C, Albano C, Osmanagaoglu K, Smitz J, Van Steirteghem A et al (2002) Effect of ovarian stimulation with recombinant follicle-stimulating hormone, gonadotropin releasing hormone antagonists, and human chorionic gonadotropin on endometrial maturation on the day of oocyte pick-up. Fertil Steril 78(5):1025–1029
Kolibianakis EM, Albano C, Kahn J, Camus M, Tournaye H, Van Steirteghem AC et al (2003) Exposure to high levels of luteinizing hormone and estradiol in the early follicular phase of gonadotropin-releasing hormone antagonist cycles is associated with a reduced chance of pregnancy. Fertil Steril 79(4):873–880
Garcia-Velasco JA, Isaza V, Vidal C, Landazábal A, Remohí J, Simón C et al (2001) Human ovarian steroid secretion in vivo: effects of GnRH agonist versus antagonist (cetrorelix). Hum Reprod 16(12):2533–2539
de Jong D, Macklon NS, Fauser BC (2000) A pilot study involving minimal ovarian stimulation for in vitro fertilization: extending the “follicle-stimulating hormone window” combined with the gonadotropin-releasing hormone antagonist cetrorelix. Fertil Steril 73(5):1051–1054
Tremellen K, Lane M (2010) Avoidance of weekend oocyte retrievals during GnRH antagonist treatment by simple advancement or delay of hCG administration does not adversely affect IVF live birth outcomes. Hum Reprod 25(5):1219–1224
Wang L, Yin M, Liu Y, Chen Q, Wang Y, Ai A et al (2017) Effect of Frozen Embryo Transfer and Progestin-primed Ovary Stimulation on IVF outcomes in women with high body mass index. Sci Rep 7(1):1–12
Kolibianakis EM, Bourgain C, Papanikolaou EG, Camus M, Tournaye H, Van Steirteghem AC et al (2005) Prolongation of follicular phase by delaying hCG administration results in a higher incidence of endometrial advancement on the day of oocyte retrieval in GnRH antagonist cycles. Hum Reprod 20(9):2453–2456
Massin N (2017) New stimulation regimens: endogenous and exogenous progesterone use to block the LH surge during ovarian stimulation for IVF. Hum Reprod Update 23(2):211–220
Wang N, Wang Y, Chen Q, Dong J, Tian H, Fu Y et al (2016) Luteal-phase ovarian stimulation vs conventional ovarian stimulation in patients with normal ovarian reserve treated for IVF: a large retrospective cohort study. Clin Endocrinol 84(5):720–728
Chen Q, Wang Y, Sun L, Zhang S, Chai W, Hong Q et al (2017) Controlled ovulation of the dominant follicle using progestin in minimal stimulation in poor responders. Reprod Biol Endocrinol 15(1):71
Wang Y, Chen Q, Wang N, Chen H, Lyu Q, Kuang Y (2016) Controlled ovarian stimulation using medroxyprogesterone acetate and hMG in patients with polycystic ovary syndrome treated for IVF: a double-blind randomized crossover clinical trial. Medicine. 95(9):e2939
Huang J, Xie Q, Lin J, Lu X, Zhu J, Gao H et al (2019) Progestin-primed ovarian stimulation with dydrogesterone versus medroxyprogesterone acetate in women with polycystic ovarian syndrome for in vitro fertilization: a retrospective cohort study. Drug Des Dev Ther 13:4461
Wang N, Zhu Q, Ma M, Liang Z, Tao Y, Wang Y et al (2020) Comparison of a progestin-primed ovarian stimulation protocol with a flexible GnRH antagonist protocol in patients with polycystic ovary syndrome who are participating in an IVF programme: study protocol for a randomised controlled trial. BMJ Open 10(12):e038153
Yu S, Long H, Chang HYN, Liu Y, Gao H, Zhu J et al (2018) New application of dydrogesterone as a part of a progestin-primed ovarian stimulation protocol for IVF: a randomized controlled trial including 516 first IVF/ICSI cycles. Hum Reprod 33(2):229–37
Turkgeldi E, Yildiz S, Cekic SG, Shakerian B, Keles I, Ata B (2020) Effectiveness of the flexible progestin primed ovarian stimulation protocol compared to the flexible GnRH antagonist protocol in women with decreased ovarian reserve. Hum Fertil (Camb) 25(2):306-312. https://doi.org/10.1080/14647273.2020.1794060. Epub 2020 Jul 16.
d’Argent EM, Ferrier C, Zacharopoulou C, Ahdad-Yata N, Boudy AS, Cantalloube A et al (2020) Outcomes of fertility preservation in women with endometriosis: comparison of progestin-primed ovarian stimulation versus antagonist protocols. J Ovarian Res 13(1):1–7
Kahyaoglu I, Dogru HY, Kaplanoglu I, Dilbaz S, Mollamahmutoglu L (2019) Impact of the duration of controlled ovarian stimulation on assisted reproduction cycle outcomes. Gynecol Obstet Reprod Med 25(1):28–32
Aybar F, Cil A, Batmaz G, Temel S, Kahraman S (2013) Does ovarian stimulation duration make any difference on pregnancy outcomes in poor responder patients undergoing IVF-ICSI cycles with GnRH antagonist protocol? Fertil Steril 100(3):S266
Heijnen E, Eijkemans M, Hughes E, Laven J, Macklon N, 3, Fauser B (2006) A meta-analysis of outcomes of conventional IVF in women with polycystic ovary syndrome. Hum Reprod Update 12(1):13–21
Acknowledgements
None.
Funding
The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Author information
Authors and Affiliations
Contributions
HS, AS, and HS wrote the first draft of the manuscript. SR and ME contributed to the design and data collection. ASA and FDG contributed to the revision process improving the quality of the paper. PD is responsible for the main concept. All authors discussed the results and contributed to the final manuscript with the specific support of PD.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
PD has been a consultant to Merck Healthcare KGaA (Darmstadt, Germany) from April 2021 till June 2023 and is a Merck employee (Medical Director, Global Medical Affairs Fertility) with Merck Healthcare KGAaA (Darmstadt, Germany) since July 2023. He declares honoraria for lecturing from Merck KGaA, MSD, Organon, and Ferring. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maghraby, H., Saleh, H., Fourtia, I.L. et al. The dilemma of the trigger timing in IVF: a review. Middle East Fertil Soc J 29, 8 (2024). https://doi.org/10.1186/s43043-024-00166-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-024-00166-w