Abstract
Background
The aim of controlled ovarian stimulation is to achieve an optimal number of mature oocytes to obtain good-quality embryos. High follicular fluid (FF) concentrations of FSH, hCG, and LH promote oocyte maturation and are associated with a higher probability of fertilization. LH concentrations in FF are consistently higher in follicles that will lead to a successful IVF outcome. The levels of some of these FF biomarkers may vary among different ovarian stimulation schemes; however, the effects of corifollitropin alfa, recombinant FSH (rFSH), LH (rLH), and highly purified urinary menotropins uhMG on these biomarkers are still unknown. The objective of this study was to characterize the profile of FF biomarkers (leptin, vascular endothelial growth factor (VEGF), metalloproteinases (MMPs), and NO2−/NO3−) according to three different protocols of controlled ovarian stimulation (COS) in poor ovarian responders (POR) and to evaluate the association between these profiles and clinical outcomes. Three groups of POR patients were examined according to the protocols used.
Results
Group C showed significant higher levels in all biomarkers (p < 0001). FF samples from Group B had the lowest levels of VEGF and Pro-MMP-9. Group A showed the lowest concentration of pro-MMP-2. The VEGF level and number of captured oocytes were positively correlated in Group C (r = 0.534, p = 0.01). MMP-9 and fertilization rate were negatively correlated in Group C (r = −0.476, p = 0.02). We found negative correlations between proMMP-2 and serum estradiol levels on the day of rhCG administration.
Conclusion
We found significant variations in the biomarker concentrations between the different controlled ovarian stimulation schemes used in POR patients. These differences can be potentially explained by the nature and composition of the gonadotropins. Our results support the hypothesis that some of these molecules should be thoroughly investigated as noninvasive predictors of egg quality.
Similar content being viewed by others
Introduction
There is still lack of consensus regarding the definition of POR in the IVF setting [1]. Poor responders are not a homogeneous group of patients, and the prognosis of the couple may vary according to certain patient characteristics [2]. Different criteria have been proposed to define this population. Initially, the Bologna criteria were proposed [3], but they were demonstrated to have limitations. More recently, the POSEIDON group proposed a new stratified classification with the asset of identifying subgroups with different prognosis according to the ability to obtain at least one euploid blastocyst for transfer [4]. This novel system relies on female age, ovarian reserve markers, ovarian sensitivity to exogenous gonadotropin, and the number of oocytes retrieved, which will assist in the identification of the patients with low prognosis and stratify such patients into one of four groups with “expected” or “unexpected” impaired ovarian response to exogenous gonadotropin stimulation. Furthermore, it introduced a new measure of clinical success in ART, namely, the ability to retrieve the number of oocytes needed to obtain at least one euploid blastocyst for transfer in each patient [5]. The incidence of POR has been reported between 5 and 35% of patients undergoing COS for IVF/ICSI [2]. Therefore, these patients represent a commonly found challenge in the clinical arena. Importantly, biomarkers expressed in FF have been shown to have an effect on oocyte growth and maturation impacting directly clinical IVF results; hence, this biological fluid provides a unique chance to have a better understanding of the processes that occur during follicular maturation [6].
Despite recent advances in assisted reproductive techniques, the selection of oocytes and embryos based on morphological and morphometric parameters is not sufficiently satisfactory, creating the need to develop biomarkers predictive of fertilization and/or implantation [7]. Therefore, an important aim of current fertility treatment is to develop an accurate, noninvasive, and cost-effective predictive test of oocyte development potential [8].
The FF composition is a possible predictor of the development potential of oocytes and embryos. It reflects the metabolism of the entire follicle and contains regulatory molecules that are crucial for successful oocyte maturation [7]. Previous studies examined hormones, growth factors, and reactive oxygen species concentrations in human FF and tried — with limited success — to relate them with the fertilization rate, oocyte development potential, and pregnancy outcome [9]. Others presented earlier data on the examinations of FF VEGF, nitric oxide (NO), interleukin-1β (IL-1β), and leptin [10].
A relationship between perifollicular blood flow, follicular oxygen content, and the developmental capacity of the developing oocyte/embryo has been suggested [11, 12], and well-vascularized follicles are associated with increased FF VEGF, good-quality oocytes and embryos, a well-vascularized endometrium, and increased pregnancy rates [13].
Nitric oxide (NO) is a regulatory molecule with vascular and inflammatory effects; it is negatively correlated with the oocyte potential to fertilize [14]. High levels of NO may exert effects on pregnancy status through complex mechanisms of endometrial receptivity (implantation) or may have negative (toxic) effects on embryos that commit them to apoptosis before implantation [15].
Leptin is produced by granulosa cells, and it is involved in multiple regulatory functions, including angiogenesis [16]. Leptin has been signaled as a potential marker of follicular hypoxia [10]. Studies have demonstrated that elevated leptin concentrations in FF at oocyte pickup are significantly associated with an adverse pregnancy outcome in women undergoing IVF [17].
The family of matrix metalloproteinases (MMP) participates in the degradation of the extracellular matrix and tissue remodeling. MMPs have a primary role in follicular rupture as evidenced in the rupture of the basal membrane of the granulosa cells and the fragmentation of the collagen matrix at the follicular apex [8, 10, 18]. Atabakhsh et al. demonstrated direct correlations between activity of MMP2 and MMP9 in FF with oocyte quality and fertilization rate [19].
The goal of controlled ovarian stimulation (COS) is to achieve an optimal number of mature oocytes to obtain good-quality embryos, to assure that at least one will lead to pregnancy. High FF concentrations of FSH, hCG, and LH have been reported to promote oocyte maturation and to be associated with eggs having a high chance of fertilization [20,21,22]. Follicular fluid FF LH was observed to be consistently higher in follicles containing oocytes that resulted in embryos leading to successful IVF attempts [23]. The levels of some of these FF biomarkers may vary among different gonadotropin stimulation schemes; however, the individual effects of currently used recombinant corifollitropin alfa, recombinant FSH (rFSH) and LH (rLH), and highly purified urinary menotropins uhMG, on these biomarkers, are still unknown [24].
The aim of this study was to characterize the FF profile of leptin, vascular endothelial growth factor (VEGF), metalloproteinases (MMPs), and NO2−/NO3− according to three different protocols of COS in POR (POSEIDON Group 2). Secondarily, we evaluated the association between these profiles and clinical outcomes.
Material and methods
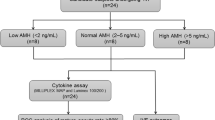
A prospective cohort clinical study was conducted at Centro de Reproducción Arcos S.C, Nascere, and was approved by Centro Médico ABC (ABC-18-35) Research and Ethics Committee. All patients provided written informed consent to participate in the study. In the period April 2016 to April 2018, a total of 60 patients met the inclusion criteria: POSEIDON criteria (Group 2), which satisfied the following features: maternal age ≥ 35 years, AMH ≥ 1.2 ng/ml or antral follicle count ≥ 5 follicles, and/or 0–9 oocytes retrieved in previous ovarian stimulation cycles (Humaidan et al., 2011). Exclusion criteria were patients with azoospermic male partners, as azoospermia may have per se an impact on embryo-developmental competence [25,26,27,28,29], and those who refused to sign the informed consent. A figure of the study design was made for better comprehension (Fig. 1).
Design of the study. Prospective cohort clinical study. In the period April 2016 to April 2018, a total of 60 patients met the inclusion criteria. Patients were assigned to three groups, all based on the use of a GnRH antagonist scheme. After the oocyte recovery, each patient’s pooled FF samples from the first gentle aspiration were divided in 4 aliquots and collected in cryotubes for examination of leptin, VEGF, MMPs, and NO2/NO3 quantification
Patients were assigned to three groups according to the attending physician criteria, all based on the use of a GnRH antagonist scheme: Group A: patients were administered a single dose of 150 μg corifollitropin alfa (Elonva®; MSD) on cycle day 3, followed from the 8th day by the application of a daily dose of 300 IU of rFSH (Gonal F®; Merck); Group B: patients received a daily dose of 300 IU of rFSH (Gonal F®; Merck) plus 150 IU of urinary menotropins uhMG (Merapur®; Ferring) starting on day 3; and Group C: patients were treated with two ampules daily of 150 IU of rFSH plus 75 IU of rLH (Pergoveris®; Merck) also starting on cycle day 3. Patients were not pretreated with OCP.
Group A utilized corifollitropin alpha + rFSH and therefore was characterized as a two recombinant FSH preparation with a high FSH dose and containing no LH; Group B used a standard combination of rFSH and uhMG (highly purified urinary menotropins) with a high FSH dose and a ratio of FSH:LH of 2:1; and Group C used the only available rFSH + rLH protocol commercially available in Mexico containing a fixed intermediate dose of recombinant FSH in an FSH:LH ratio of 2:1.
Starting on the 7th day of the cycle, all groups were given a daily GnRH antagonist dose (Cetrotide®; Merck) of 0.25 mg. All medications continued until the day of the trigger. When ≥ 2 follicles reached a diameter ≥ 17 mm by vaginal ultrasonography, a single dose of 250 mcg of rhCG (Ovidrel®; Merck) was applied to trigger ovulation (36 h before oocyte recovery).
The follicles were aspirated via ultrasound-guided transvaginal approach from each ovary using the standard aspirating needle suction pump (100 mm Hg) system routinely used in our program. Each follicle was aspirated individually. Initially, each follicle was gently aspirated into a vacuum-sealed tube devoid of culture medium. This initial gentle aspiration was limited inside the follicle in terms of time, needle manipulation, and volume aspirated to minimize contamination with blood. After disconnecting the tube, a sample of FF (usually clear in appearance or minimally contaminated with blood, giving a clear amber color) was withdrawn immediately by capillary action into a sterile 0.8-mm-inside diameter capillary tube. All initial aspirations from a given patient were pooled. Immediately, with the aspirating needle remaining in the follicle, a repeat aspiration was performed into a second vacuum-sealed tube containing Dulbecco’s phosphate-buffered saline (GIBCO Laboratories, Grand Island, NY, USA) to ensure oocyte collection.
Immediately after the oocyte recovery, each patient’s pooled FF samples from the first gentle aspiration were divided in 4 aliquots and collected in cryotubes (Cryovial, Simport), for examination of leptin, and VEGF and MMPs quantification; they were stored in a plastic rack for cryovials freezing at −25 °C. In the specific case of NO2−/NO3−, the tubes were placed in reeds immersed in liquid nitrogen and stored at −196 °C.
Leptin
Leptin determination was done by ELISA (enzyme-linked immunosorbent assay), using the Human Leptin DuoSet kit (R&D, Minneapolis, USA), with a sensitivity range of 31.3–2000 pg/mL. The standard curve consisted of a blank and seven standards: 31.3, 62.5, 125, 250, 500, 1000, and 2000 pg/mL of human recombinant leptin. A volume of 100 μL was used for each of the samples. The plate was read at 450 nm.
VEGF
VEGF quantification was carried out by a commercial Human VEGF DuoSet ELISA (R&D, Minneapolis, USA), with a sensitivity range of 31.3–2000 pg/mL. The sample volume used was 100 μL per well. The standard curve was constructed with a blank and seven standards: 31.3, 62.5, 125, 250, 500, 1000, 2000 pg/mL of VEGF. The plate was read at 450 nm.
MMP
Protein quantification was performed with the bicinchoninic acid method. The total proteins obtained from the initial FF aspiration were quantified by means of the Pierce™ BCA Protein Assay Kit reagent (Thermo Scientific), by constructing a standard curve at an absorbance of 542 nm with Gen5 3.0 software on the Synergy HT BioTek device.
Metalloproteinase zymography was used to examine the gelatinolytic activity of the initial FF sample and was determined by gels/substrate as shown in Fig. 2. Aliquots containing 10 μg of protein from each of the media were subjected to electrophoresis in 8% polyacrylamide gels with sodium dodecyl sulfate co-polymerized with swine type A gelatin (Sigma, St. Louis, MO, USA) at 1% in non-denaturing conditions, using a mini-gel format system (Bio-Rad, Richmond, CA, USA).
Representative MMP gels per clinical group. MMP-2 and MMP-9 activity in follicular liquids. Representative gelatin zymography of the three study groups: A EA, B EB, and C EC, showing two forms of MMP-9, a 92 kDa proenzyme and a 84 kDa enzyme activity. MMP-2 evidenced the 72 kDa pro-enzyme form. Supernatant of U937 cells was used as a marker of gelatinolytic activity
Enzymatic-activity zones appeared as clear lysis bands against an undegraded substrate background. Activity markers for MMP-2 and MMP-9 were included in each experiment using the supernatant obtained from the U937.11 promyelocyte cell line. The bands obtained were analyzed by densitometry by image analyzer (UVP, Southern, CA, USA) and expressed as optical density.
NO
The concentration of nitric oxide in the initially aspirated FF fluids was indirectly evaluated by a commercial ELISA test, using the Nitrate/Nitrite Colorimetric Assay Kit (Cayman Chemicals, Mi, USA), with a detection limit of 2.5 μM. The sample volume used was 80 μL in each of the wells. The standard curve was constructed with seven standards and a blank that were used in duplicate: 0, 5, 10, 15, 20, 25, and 30 μM of nitrates. The plate was read at an absorbance of 540 nm.
FSH, LH, estradiol, progesterone, AMH, and prolactin were measured by ELISA following standard clinical protocols used in our program.
Intracytoplasmic sperm injection (ICSI) was performed in all metaphase II oocytes (MII at aspiration or 5 h later from conversion from metaphase I stage), and expanded blastocysts were vitrified. Warmed blastocysts were transferred in a deferred cycle of estrogen and progesterone supplementation, on days 5–7 of progesterone administration, according to the individual development of the blastocysts by single embryo transfer (SET) or double embryo transfer (DET). The embryo quality on day 3 was determined according to the morphological assessment criteria of ASEBIR (2015) [30, 31].
Outcome measures and statistical analysis
Blastocyst number on day 5, blastocyst mean quality on day 5, metaphase II oocytes rate (oocytes in metaphase II/total number of captured oocytes), fertilization rate (oocytes that developed two pronuclei/number of injected oocytes), embryo transfer rate (ratio of patients with transferred embryos among the number of total patients in the group), pregnancy rate (ratio of pregnant patients with a positive beta-hCG among the number of patients with transferred embryos), and live birth rate (ratio of patients with at least one live newborn, either by delivery or caesarean section, among the number of pregnant patients) were calculated. Once the data were captured, the statistical analysis was performed using GraphPad Prism Version 7 program (GraphPad Software, Inc. San Diego, CA, USA). Normality test was done using Kolmogórov-Smirnov test, qualitative variables were expressed in proportions as measures of absolute and relative frequency, and for the quantitative measures, central tendency and dispersion measures were used, expressed as median and interquartile ranges. The following hypothesis tests were used; for the quantitative variables, Kruskal-Wallis or ANOVA tests were used depending on the case, and the qualitative variables were analyzed with Fisher’s exact test. After analysis of variance, the Benjamini and Hochberg post hoc test was applied to identify which groups differ in the concentrations of follicular markers. The correlations were made by means of Spearman’s nonparametric correlation coefficient test and Pearson correlation test, as the case may be. p ≤ 0.05 was considered statistically significant.
Results
Demographic data of the couples among the three groups were similar (Table 1). There were no significant differences among groups regarding cause of infertility (tubal, endometriosis, PCO, and male factor (data not shown). All patients completed the stimulation and aspiration protocols.
In terms of COS and fertilization results, no significant differences were found between groups in triggering day, number of follicles with a diameter ≥ 17 mm, serum estradiol and progesterone on the day of rhCG application, total number of captured oocytes, number of metaphase II oocytes, number of injected and fertilized oocytes, diploid embryos, and number of embryos on day 3 or day 5 (Table 2).
Table 3 shows the examined intrafollicular biomarkers per clinical group and the overall statistical differences, and Table 4 presents significant differences in their concentrations when comparing group to group. Importantly, FF samples from patients from Group C had significantly higher levels of all the studied biomarkers (p < 0.0001) (Table 3). Group B had the lowest levels of FF VEGF and proMMP-9 (p < 0.0004 compared to Group A), whereas Group A had the lowest levels of proMMP-2 (p < 0.005 compared to Group B) (Table 4). There were no differences in major reproductive outcomes between groups, the results are shown in Table 5
In Group C, VEGF levels and number of captured oocytes were positively correlated (r = 0.534, p = 0.01), and MMP-9 levels and fertilization rate were negatively correlated (r = −0.476, p = 0.029). A negative correlation was found between proMMP-2 and serum estradiol levels on the day of rhCG administration in Groups A, B, and C (r = −0.454, p = 0.04; r = −0.577, p = 0.007, and r = −0.556, p = 0.01), respectively. Also, positive correlations between leptin and number of captured oocytes (r = 0.453, p = 0.04) and leptin and metaphase II rate (r = 0.434, p = 0.056) were observed in Group B.
All MMPs studied were significantly higher in Group C (Table 3). A representative gel is shown in Fig. 2. ProMMP-2 and MMP-9 were negatively correlated in Group B (r = −0.491, p = 0.0278). A negative correlation between MMP-9 and follicles ≥ 17 mm on triggering day (r = −0.458, p = 0.03) was found in Group A. For Group C, there were negative correlations between MMP-9 and the number of follicles with a diameter ≥ 17 mm (r = −0.037, p = 0.03) as well as between MMP-9 and fertilization rate (r = −0.476, p = 0.029).
Finally, there were significant lower concentrations of NO2−/NO3 in Group A (p = 9.7e−10) and B (p = 4.0e−12) in contrast to Group C (17.6 μM). Also, a negative correlation between NO2−/NO3− and follicles with a diameter ≥ 17 mm (r = −0.488, p = 0.02) was found in Group B.
Discussion
The main objective of this study was to characterize the profiles of FF biomarkers (leptin, VEGF, MMPs, and NO2−/NO3−) according to three different protocols for COS protocols in women with POR classified as POSEIDON Group 2.
First, this prospective clinical and research cohort study showed unequivocal and significant differences in FF biomarker concentrations among three commonly used COS protocols in POR, i.e., corifollitropin alfa + rFSH, rFSH + urinary menotropins (uhMG), and a fixed dose rFSH + rLH protocol. Importantly, Group C patients, who received a fixed and a lower dose of FSH and LH (in the forms of rFSH + rLH), showed significantly higher concentrations of all intrafollicular biomarkers compared to the other two groups. Patients in Group A were stimulated with pure FSH (no LH) in the forms of corifollitropin and rFSH, and patients in Group B received FSH and LH, and possibly hCG, all of them present in uhMG. The fundamental differences between the three stimulation protocols were higher doses of FSH in Groups A and B and the absence/presence, nature, and dose of the LH used.
To obtain a urinary menotropin preparation with equal proportions of FSH and LH, highly reproducible preparation procedures are needed. If the LH activity is very low, hCG is added to compensate. The pharmaceutical behind urinary menotropins (Merapur®; Ferring) has stated that it does not add external hCG to the drug, and that its purity is comparable to that obtained with recombinant gonadotropin products; however, in a study conducted by Van de Weijer et al., the analysis of the composition of this drug revealed the presence of not two but three hormones: FSH, LH, and hCG, in addition to a significant percentage of impurities (30%). These differences may have had an impact on the follicular fluid profiles of the patients studied herein [32].
FSH, LH, and hCG belong to a family of glycoproteins that are heterodimers of two subunits (α and β). These hormones have the same α subunit but differ in the β subunit, which determines the biological specificity of each molecule. LH and hCG have a rather similar β subunit, which only differs by the extension of the carboxyl-terminal peptide (CTP) from the hCG subunit. Corifollitropin alfa is composed of the union between the hCG CTP and the β subunit of the FSH [33].
Although the physiologic role of LH during the follicular phase of a natural cycle is unquestionable, the impact of LH addition during COS remains controversial [34]. It has been documented that addition of LH leads to different patterns in the synthesis of follicular steroids, which may affect oocyte maturation and competence [34]. For example, use of recombinant LH resulted in an LH-dose-dependent increase of follicular fluid E2, androstenedione, and testosterone, which in turn may affect follicular through different regulatory molecules. Furthermore, there appears to be an optimal level of LH action with low levels resulting in egg incompetence for meiosis and high levels leading to oocyte atresia, and more high-quality embryos were observed using highly purified sing pure FSH [35].
Additionally, there is growing evidence that the addition of LH has a positive effect in patients with age over 35 years, and patients diagnosed with POR, since it increases FSH receptor expression and growth, improves follicular recruitment, and it also reduces the granulosa cell apoptosis [3]. The mechanism by which the addition of LH improves ovarian response in patients with POR is not clear. An excessive suppression of endogenous LH after downregulation with a GnRH analogue is a plausible explanation, while another is related to the presence of polymorphisms in the LH molecule (LH β-chain variant), reducing the bioactivity of the molecule or polymorphisms of the LH receptor [36].
Recombinant FSH is the preferred choice of gonadotropins in POR patients, and there is ample high-quality evidence showing that rFSH is superior to urinary FSH and human menopausal gonadotropin (hMG) as a means to increase the oocyte yield [37]. This is crucial, since the POSEIDON criteria rely on oocyte numbers to increase the chances of having at least one euploid blastocyst for transfer. The most recent systematic review and a further meta-analysis have shown that adding rLH to COS protocols is beneficial for two subgroups of patients: (i) women with an adequate ovarian reserve having an unexpected hyporesponse to rFSH monotherapy, i.e., POSEIDON groups 1 and 2, and (ii) patients 36–39 years of age [38, 39]. Therefore, adding rLH to COS in POSEIDON groups 1 and 2 patients should be considered [36], and that was the rationale for introducing the combination of rFSH + rLH into our protocols.
The recommended maximum daily dose of rFSH is 300 IU, as higher doses do not increase neither the clinical pregnancy rate nor the live birth rate [40]. Corifollitropin alfa, a long-acting rFSH, has the advantage of a rapid increase in FSH serum level, which leads to early recruitment and an increase in the number of preovulatory follicles [41, 42]. In a randomized control trial that included POR patients following Bologna criteria, corifollitropin alfa did not increase the pregnancy rate compared to rFSH; however, significantly more embryos were available for freezing, which could potentially increase the cumulative birth rate by increasing the chance of having at least one euploid embryo for transfer [42].
Second, we investigated the individual variations among the studied biomarkers according to COS protocols. High levels of follicular leptin were previously shown to negatively correlate with follicular PO2, resembling a possible marker of follicular hypoxia and suboptimal embryonic development [24]. Moreover, it has been described that the average leptin concentration is higher in FF of oocytes that present two pronuclei compared to those that had no evidence of fertilization [43]. In the present study, we found significant differences in this hormone levels between the A vs C and B vs C groups. LH and hCG are characterized by specific molecular and biochemical features; they interact with distinct binding sites of the same receptor, resulting in lower dissociation rate by hCG than LH binding [44]. Gonadotropin-specific ligand-receptor features imply different gene expression and intracellular signaling in vitro. According to Casarini et al. (2016), downstream signaling pathways of gonadotropins consist of LH-related proliferative and anti-apoptotic signals vs. high steroidogenic potential and pro-apoptotic activity of hCG in human primary granulosa cells [45]. Here, we found a positive correlation between leptin and number of captured oocytes and leptin versus number of metaphase II eggs (Group B). Several reports have demonstrated that a narrow-leptin range is necessary to maintain a normal reproductive function, and that concentrations below or above these levels could interfere with the function of the hypothalamic-pituitary-gonadal axis [16].
Multiple studies have established that FF VEGF levels are significantly correlated with the degree of follicular peripheral vascularization [4, 11, 12, 46]. However, its correlation with reproductive outcomes is still controversial. Higher levels of intrafollicular VEGF have been observed in oocytes with fertilization failure. Furthermore, they have been negatively associated with the estrogen peak, number of metaphase II oocytes, and embryonic morphology [10, 24, 29]. Conversely, Monteleone et al. reported that VEGF levels are positively correlated with the degree of peripheral vascularization; additionally, oocytes obtained from follicles with a higher degree of vascularization had a higher fertilization rate and a better embryonic quality [11]. Similar results were obtained in this study, where a positive correlation between VEGF and number of captured oocytes was found in Group C (rFSH + rLH). Our results provide further support to the hypothesis raised by Monteleone et al. about the crucial role of vascularization in follicular development. Group C had statistically significant higher levels of VEGF compared to the other groups. Min-zhi-Gao et al. support this concept as they found a positive correlation between VEGF and the dose of gonadotropins administered [12].
Barrionuevo et al. concluded that elevated levels of nitric oxide in FF may be useful for predicting a poor embryo outcome measured as the mature-oocytes potential to fertilize [47]. Here, a negative correlation between nitric oxide with follicles with a diameter > 17 mm was found in Group B. In the same way, Revelli et al. pointed that excessive nitric oxide production in the microenvironment surrounding the oocyte could trigger apoptosis inside the follicle before fertilization, which affects the oocyte development [24]. Likewise, serum nitric oxide was associated with implantation failure. This could be explained as high levels of nitric oxide in follicular fluid could generate an inflammatory reaction that negatively affects fertilization [10]. Taken together, these data suggest that an excessive production of NO in the microenvironment surrounding the oocyte could trigger apoptosis within the follicle before fertilization, thus affecting oocyte development [24]. FF concentrations of nitrites/nitrates could eventually be used a negative markers of oocyte quality; however, their assessment is rather tricky, and their intrafollicular levels were not found to correlate with IVF outcome [48]; thus, it is unlikely that the measurement of NO or its derivates will be used to identify optimal oocytes.
Matrix metalloproteinases (MMPs) catalyze the normal turnover of extracellular matrix (ECM) macromolecules [49]. MMPs are membrane bound and depict gelatinase activity and hydrolyze gelatin into polypeptides, peptides, and amino acids that can then be secreted through the cellular membrane. MMP-2 and MMP-9 belong to gelatinases and facilitate both gelatin and collagen-binding through three fibronectin type-II-like repeat domains inserted in the catalytic domain of the structure [50]. The rupture of the basal membrane of granulosa cells and the collagen matrix fragmentation at the follicular apex occur through the action of a cascade of proteolytic events that involve an increase in MMP activity before ovulation [14]. Here, we showed that levels of Pro-MMP-2 in FF were negatively correlated with serum estradiol levels on the day of rhCG application and the number of captured oocytes in all groups. Nevertheless, Atabakhsh et al. did not observe a correlation between MMP-2 activity with oocyte count and fertilization rate. Moreover, Yang et al. concluded that higher levels of MMP-2 in IVF/ICSI cycles were positively correlated with the oocyte maturation and fertilization rates and proposed this metalloproteinase as a possible marker of oocyte maturation rate [19, 51].
We also found a negative correlation between MMP-9 levels with fertilization rate in Group C. Nevertheless, Atabakhsh et al. reported no significantly correlation between these two variables but demonstrated a positive correlation between MMP-9 and oocyte morphology [19]. We observed a negative correlation between MMP-9 with number of follicles > 17 mm in Group A. To allow accurate remodeling and limit the site and extent of proteolytic degradation by MMPs, there must be a delicate balance between the activity of MMPs and their inhibitors [18].
Third, we evaluated the association between the FF biomarker profiles and clinical outcomes. Results of rate of metaphase II oocytes, fertilization rate, transfer rate, pregnancy rate, AND live birth rate were not different among groups, although the sample sizes regarding pregnancy were limited.
Although POR typically consist of a nonhomogeneous group of patients, the restriction of patients’ enrolment to POSEIDON Group 2 eliminates many of those concerns as all studied subgroups groups were similar in terms of age, AMH values, antral follicular count, and number of eggs recovered. However, we acknowledge that this study has some limitations. They include a relatively small sample size, its non-randomized design, and the fact that the total doses of gonadotropins used in the three arms were not equivalent. Future prospective, controlled, and randomized studies may be necessary to validate these results.
Conclusions
We found significantly higher levels of leptin, VEGF, nitric oxide, MMP-2, MMP-9, and ProMMP-9 in patients who received rFSH + rLH, indicating a variation in these biomarkers’ concentration according to the composition of the gonadotropins administered (LH and FSH) and their nature (recombinant or urinary) in POR patients classified as POSEIDON Group 2. We speculate that the specific effect of LH at a cellular level could explain some of the differences between FF fluid biomarkers and follicle dynamics. Whether these implications apply to other types of responders to COS remains to be investigated.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to patient privacy but could be available from the corresponding author on reasonable request.
References
Polyzos NP, Devroey P (2011) A systematic review of randomized trials for the treatment of poor ovarian responders: is there any light at the end of the tunnel? Fertil Steril 96:1058–61.e7
Oudendijk JF, Yarde F, Eijkemans MJC, Broekmans FJM, Broer SL (2012) The poor responder in IVF: is the prognosis always poor? A systematic review. Hum Reprod Update 18:1–11
Drakopoulos P, Bardhi E, Boudry L, Vaiarelli A, Makrigiannakis A, Esteves SC et al (2020) Update on the management of poor ovarian response in IVF: the shift from Bologna criteria to the Poseidon concept. Ther Adv Reprod Heal 14:263349412094148
Alviggi C, Andersen CY, Buehler K, Conforti A, De Placido G, Esteves SC et al (2016) A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril 105:1452–1453
Esteves SC, Alviggi C, Humaidan P, Fischer R, Andersen CY, Conforti A et al (2019) The POSEIDON criteria and its measure of success through the eyes of clinicians and embryologists. Front Endocrinol 10:814 Frontiers Media S.A. Available from: https://pubmed.ncbi.nlm.nih.gov/31824427
Zamah AM, Hassis ME, Albertolle ME, Williams KE (2015) Proteomic analysis of human follicular fluid from fertile women Clin. Proteomics 12:1–12
Chen F, Spiessens C, D’Hooghe T, Peeraer K, Carpentier S (2016) Follicular fluid biomarkers for human in vitro fertilization outcome: proof of principle. Proteome 14:1–11. https://doi.org/10.1186/s12953-016-0106-9
Wallace M, Cottell E, Gibney MJ, McAuliffe FM, Wingfield M, Brennan L (2012) An investigation into the relationship between the metabolic profile of follicular fluid, oocyte developmental potential, and implantation outcome. Fertil Steril 97:1078–84
Julie D, Lamb A, Zamah M, Shen S, McCulloch C, Cedars MI, Rosen MP (2010) Follicular fluid steroid hormone levels are associated with fertilization outcome after intracytoplasmic sperm injection. Fertil Steril 94:952–957
Barroso G, Barrionuevo M, Rao P, Graham L, Danforth D, Huey S et al (1999) Vascular endothelial growth factor, nitric oxide, and leptin follicular fluid levels correlate negatively with embryo quality in IVF patients. Fertil Steril 72:1024–1026
Monteleone P, Giovanni Artini P, Simi G, Casarosa E, Cela V, Genazzani AR (2008) Follicular fluid VEGF levels directly correlate with perifollicular blood flow in normoresponder patients undergoing IVFJ. Assist Reprod Genet 2008(25):183–186
Gao MZ, Zhao XM, Lin Y, Sun ZG, Zhang HQ (2012) Effects of EG-VEGF, VEGF and TGF-β1 on pregnancy outcome in patients undergoing IVF-ET treatment. J Assist Reprod Genet 29:1091–1096
Vural F, Vural B, Doğer E, Çakıroğlu Y, Çekmen M (2016) Perifollicular blood flow and its relationship with endometrial vascularity, follicular fluid EG-VEGF, IGF-1, and inhibin-a levels and IVF outcomes. J Assist Reprod Genet 33:1355–1362
Vignini A, Turi A, Giannubilo SR, Pescosolido D, Scognamiglio P, Zanconi S et al (2008) Follicular fluid nitric oxide (NO) concentrations in stimulated cycles: the relationship to embryo grading. Arch Gynecol Obstet 277:229–232
Yalçınkaya E, Cakıroğlu Y, Doğer E, Budak O, Cekmen M, Calışkan E (2013) Effect of follicular fluid NO, MDA and GSH levels on in vitro fertilization outcomes. J Turkish Ger Gynecol Assoc 14:136–141
Caprio M, Fabbrini E, Isidori AM, Aversa A, Fabbri A (2001) Leptin in reproduction. Trends Endocrinol Metab 12:65–72
Al-Aqbi M, Hart R, Ajuogu P, de Touw TV, McFarlane J, Smart N (2020) Follicular fluid leptin as a marker for pregnancy outcomes in women undergoing IVF treatment: a systematic review and meta-analysis. Hum Fertil (Camb) 25:1–10
Curry TE, Osteen KG (2003) The matrix metalloproteinase system: changes, regulation, and impact throughout the ovarian and uterine reproductive cycle. Endocr Rev 24:428–465
Atabakhsh M, Khodadadi I, Amiri I, Mahjub H, Tavilani H (2018) Activity of matrix metalloproteinase 2 and 9 in follicular fluid and seminal plasma and its relation to embryo quality and fertilization rate. J Reprod Infertil 19:140–145
Ellsworth LR, Balmaceda JP, Schenken RS, Silverman AY, Prihoda TJ, Asch RH (1984) Human chorionic gonadotropin and steroid concentrations in human follicular fluid in relation to follicle size and oocyte maturity in stimulated ovarian cycles. Acta Eur Fertil 15:343–346
Cha KY, Barnes RB, Marrs RP, Lobo RA (1986) Correlation of the bioactivity of luteinizing hormone in follicular fluid with oocyte maturity in the spontaneous cycle. Fertil Steril 45:338–341
Enien WM, Chantler E, Seif MW, Elstein M (1998) Human ovarian granulosa cells and follicular fluid indices: the relationship to oocyte maturity and fertilization in vitro. Hum Reprod 13:1303–1306
Mendoza C, Ruiz-Requena E, Ortega E, Cremades N, Martinez F, Bernabeu R et al (2002) Follicular fluid markers of oocyte developmental potential. Hum Reprod 17:1017–1022
Revelli A, Piane LD, Casano S, Molinari E, Massobrio M, Rinaudo P (2009) Follicular fluid content and oocyte quality: from single biochemical markers to metabolomics. Reprod Biol Endocrinol 7:1–13
Palermo GD, Schlegel PN, Hariprashad JJ, Ergün B, Mielnik A, Zaninovic N et al (1999) Fertilization and pregnancy outcome with intracytoplasmic sperm injection for azoospermic men. Hum Reprod 14:741–748
Balaban B, Urman B, Isiklar A, Alatas C, Mercan R, Aksoy S et al (2001) Blastocyst transfer following intracytoplasmic injection of ejaculated, epididymal or testicular spermatozoa. Hum Reprod 16:125–129
Vernaeve V, Tournaye H, Osmanagaoglu K, Verheyen G, Van Steirteghem A, Devroey P (2003) Intracytoplasmic sperm injection with testicular spermatozoa is less successful in men with nonobstructive azoospermia than in men with obstructive azoospermia. Fertil Steril 79:529–533
Loutradi KE, Tarlatzis BC, Goulis DG, Zepiridis L, Pagou T, Chatziioannou E et al (2006) The effects of sperm quality on embryo development after intracytoplasmic sperm injection. J Assist Reprod Genet 23:69–74
Mazzilli R, Cimadomo D, Vaiarelli A, Capalbo A, Dovere L, Alviggi E et al (2017) Effect of the male factor on the clinical outcome of intracytoplasmic sperm injection combined with preimplantation aneuploidy testing: observational longitudinal cohort study of 1,219 consecutive cycles. Fertil Steril [Internet] 108:961–972.e3. https://doi.org/10.1016/j.fertnstert.2017.08.033 Elsevier Inc
Hurtado de Mendoza MV, Ten J (2015) Evaluación morfológica de cada estadio de D+0 a D+3. Cuad Embriol clínica criterios ASEBIR valoración morfológica oocitos embriones tempranos y blastocistos humanos. p 9–20
Gardner DK, Schoolcraft WB (1999) Culture and transfer of human blastocysts. Curr Opin Obstet Gynecol 11:307–311
van de Weijer BHM, Mulders JWM, Bos ES, Verhaert PDEM, van den Hooven HW (2003) Compositional analyses of a human menopausal gonadotrophin preparation extracted from urine (menotropin). Identification of some of its major impurities. Reprod Biomed Online 7:547–557. https://doi.org/10.1016/S1472-6483(10)62071-8 Reproductive Healthcare Ltd, Duck End Farm, Dry Drayton, Cambridge CB23 8DB, UK
Woodward BJ (2020) Textbook of assisted reproduction Textb. Assist. Reprod
Bosch E, Labarta E, Kolibianakis E, Rosen M, Meldrum D (2016) Regimen of ovarian stimulation affects oocyte and therefore embryo quality. Fertil Steril 105:560–570
Smitz J, Andersen AN, Devroey P, Arce J-C (2007) Endocrine profile in serum and follicular fluid differs after ovarian stimulation with HP-hMG or recombinant FSH in IVF patients. Hum Reprod 22:676–687
Abu-Musa A, Haahr T, Humaidan P (2020) Novel physiology and definition of poor ovarian response; clinical recommendations. Int J Mol Sci 21:1–20
Andersen AN, Devroey P, Arce J-C (2006) Clinical outcome following stimulation with highly purified hMG or recombinant FSH in patients undergoing IVF: a randomized assessor-blind controlled trial. Hum Reprod 21:3217–3227
Alviggi C, Conforti A, Esteves SC, Andersen CY, Bosch E, Bühler K et al (2018) Recombinant luteinizing hormone supplementation in assisted reproductive technology: a systematic review. Fertil Steril 109:644–664
Conforti A, Esteves SC, Di Rella F, Strina I, De Rosa P, Fiorenza A et al (2019) The role of recombinant LH in women with hypo-response to controlled ovarian stimulation: a systematic review and meta-analysis. Reprod Biol Endocrinol 17:18 BioMed Central. Available from: https://pubmed.ncbi.nlm.nih.gov/30728019
Baker VL, Brown MB, Luke B, Smith GW, Ireland JJ (2015) Gonadotropin dose is negatively correlated with live birth rate: analysis of more than 650,000 assisted reproductive technology cycles. Fertil Steril 104:1145
Fauser BCJM, Alper MM, Ledger W, Schoolcraft WB, Zandvliet A, Mannaerts BMJL (2010) Pharmacokinetics and follicular dynamics of corifollitropin alfa versus recombinant FSH during ovarian stimulation for IVF. Reprod BioMed Online 21:593–601
Drakopoulos P, Vuong TNL, Ho NAV, Vaiarelli A, Ho MT, Blockeel C et al (2017) Corifollitropin alfa followed by highly purified HMG versus recombinant FSH in young poor ovarian responders: a multicentre randomized controlled clinical trial. Hum Reprod 32:2225–2233
Kleiner DE, Stetlerstevenson WG (1994) Quantitative zymography: detection of picogram quantities of gelatinases. Anal Biochem 218:325–329 Available from: http://www.sciencedirect.com/science/article/B6W9V-45PMGFG-7K/2/8aca7f7c8c92a018d6518cd804d2cf1f
Huhtaniemi IT, Catt KJ (1981) Differential binding affinities of rat testis luteinizing hormone (lH) receptors for human chorionic gonadotropin, human lH, and ovine LH. Endocrinology 108:1931–1938
Casarini L, Riccetti L, De Pascali F, Nicoli A, Tagliavini S, Trenti T et al (2016) Follicle-stimulating hormone potentiates the steroidogenic activity of chorionic gonadotropin and the anti-apoptotic activity of luteinizing hormone in human granulosa-lutein cells in vitro. Mol Cell Endocrinol 422:103–114. https://doi.org/10.1016/j.mce.2015.12.008. Elsevier
Kim KH, Oh DS, Jeong JH, Shin BS, Joo BS, Lee KS (2004) Follicular blood flow is a better predictor of the outcome of in vitro fertilization-embryo transfer than follicular fluid vascular endothelial growth factor and nitric oxide concentrations. Fertil Steril 82:586–592
Barrionuevo MJ, Schwandt RA, Rao PS, Graham LB, Maisel LP, Yeko TR (2000) Nitric oxide (NO) and interleukin-1β (IL-1β) in follicular fluid and their correlation with fertilization and embryo cleavage. Am J Reprod Immunol 44:359–364
Manau D, Balasch J, Jiménez W, Fábregues F, Civico S, Casamitjana R et al (2000) Follicular fluid concentrations of adrenomedullin, vascular endothelial growth factor and nitric oxide in IVF cycles: relationship to ovarian response. Hum Reprod 15:1295–1299
Raeeszadeh-Sarmazdeh M, Do LD, Hritz BG (2020) Metalloproteinases and their inhibitors: potential for the development of new therapeutics. Cells 9:1313
Eckhard U, Huesgen PF, Schilling O, Bellac CL, Butler GS, Cox JH et al (2016) Active site specificity profiling of the matrix metalloproteinase family: proteomic identification of 4300 cleavage sites by nine MMPs explored with structural and synthetic peptide cleavage analyses. Matrix Biol 49:37–60
Yang WJ, Liu FC, Hsieh JS, Chen CH, Hsiao SY, Lin CS (2015) Matrix metalloproteinase 2 level in human follicular fluid is a reliable marker of human oocyte maturation in in vitro fertilization and intracytoplasmic sperm injection cycles. Reprod Biol Endocrinol 13:2–9. https://doi.org/10.1186/s12958-015-0099-8
Acknowledgements
This study was directed by Juan Gerardo Barroso Villa to obtain a PhD degree in Doctorado en Investigación en Medicina graduate program at Instituto Politécnico Nacional.
Funding
The development of this project was financed by Centro de Reproducción Arcos, S.C.
Author information
Authors and Affiliations
Contributions
GB provided general input throughout the design, creation, and review processes of this manuscript. CV made minor corrections and reviewed the entire manuscript for approval. AW and AM provided general input throughout the design, creation, analysis, and writing processes of this manuscript. FP quantified the follicular fluid markers and performed the corresponding zymography. IP reviewed the manuscript and provided significant suggestions for its improvement. SO was the final internal reviewer and suggested significant changes to the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Centro Médico ABC (ABC-18-35) Research and Ethics Committee. All patients provided written informed consent to participate in the study.
Consent for publication
All authors of this study approve its publication in this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barroso-Villa, G., Valdespin-Fierro, C., Weiser-Smeke, AE. et al. Follicular fluid biomarkers for prediction of human IVF outcome in women with poor ovarian response. Middle East Fertil Soc J 28, 2 (2023). https://doi.org/10.1186/s43043-023-00128-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-023-00128-8