Abstract
Background
Despite extensive research efforts, understanding the precise causes and molecular underpinnings of age-related macular degeneration (AMD) remains elusive. Exploring different populations becomes crucial to establish conclusive insights into the role of genetic factors in AMD.
Methodology
This study aimed to investigate the association between the well-documented major risk alleles in the HTRA1, ARMS2 and CFH genes with AMD in the Malaysian multi-ethnic population. A total of 205 subjects were enrolled in this study, 103 were diagnosed with AMD while 102 represented the control subjects. Genomic DNA was extracted from peripheral blood mononuclear cells and gene amplification was performed by polymerase chain reaction. Subsequently, genotyping for the HTRA1, ARMS2 and CFH genes was performed using direct DNA sequencing analysis.
Results
Significant associations (p < 0.05) were detected with AMD for both SNP rs11200638: G > A in the promoter of HTRA1 and rs10490924: G > T in ARMS2 but not for variant Y402H in CFH gene (p > 0.05) in our study population. The A allele frequency of rs11200638 in the HTRA1 promoter was 51.9% in cases versus 39.2% in controls (p = 0.010). The frequency of AA genotype was 28.2% for AMD cases, compared to 17.6% in controls (OR 2.58, 95% CI 1.19–5.58; p = 0.043). The frequency of the TT genotype of rs10490924 in ARMS2 was 25.2% in cases versus 8.8% in controls (OR 2.23, 95% CI 0.83–5.99; p = 0.002).
Conclusion
The study reveals an association between specific genetic variants in the HTRA1 and ARMS2 genes and the occurrence of AMD in the Malaysian population. However, contrary to expectations, the study did not identify a substantial correlation between AMD and the Y402H variant of the CFH gene in this specific population.
Similar content being viewed by others
Background
Age-related macular degeneration (AMD) is a complex, progressive disease which influenced by both genetic and environmental factors, yet its exact cause remains elusive despite extensive research [1, 2]. With an anticipated demographic shift towards aging populations, the prevalence of AMD is set to double in the coming years, posing a growing concern for older Malaysians [3]. Notably, the age-standardized prevalence of AMD in a multi-ethnic Asian cohort, comprising Singaporean Chinese (7.3%), Indian (5.7%), and Malay (7.7%) ethnic groups, exhibited similar rates [4].
AMD profoundly impacts both individuals and society at large, particularly among older adults, leading to significant vision loss and diminished quality of life. The economic implications of AMD are substantial, with high healthcare costs for ongoing medical care and assistive technologies, coupled with indirect costs from reduced workforce participation and productivity losses. Caregivers bear additional burdens, and the condition is associated with heightened rates of depression and anxiety, necessitating mental health support. The increasing prevalence of AMD also strains public health resources, emphasizing the crucial need for educational programs, early detection initiatives, and effective treatments. Therefore, addressing AMD in Malaysia requires a comprehensive approach, including regular screenings, promotion of healthy lifestyles, and continual research to enhance treatment options. Collaborative efforts shall be aimed at increasing awareness, improving access to care, and effectively managing AMD, thereby safeguarding vision and the quality of life of aging Malaysians.
Genes in the complement pathway and a region of chromosome 10 have been implicated as the major genetic contributors to AMD. Complement Factor H (CFH) gene is located on the q arm of chromosome 1 at position 32 with the Tyr402His polymorphism was one of the variants identified. CFH usually has the amino acid tyrosine (Tyr) at position 402, but occasionally it may contain the amino acid histidine (His) instead. This version is less effective at regulating the complement system than the version with Tyr at position 402, which may help explain the increased disease risk. Studies assessing the association between the CFH Tyr402His polymorphism and AMD have indicated that this polymorphism plays a role in the majority of AMD cases in the Caucasian population [5] than in the Asian cohorts.
Both Human High-Temperature Requirement A-1 (HTRA1) and Age-Related Maculopathy Susceptibility 2 (ARMS2) genes are in chromosome 10 on the q arm at positions 26.3 and 26.13, respectively. HTRA1 gene is reported as a likely causal variant for AMD with a population-attributed risk of 49.3% and 86% in the Caucasian [6] and Chinese populations [7], respectively. A functional HTRA1 protein is necessary for the cellular and environmental stress damage control system in Escherichia coli [8]. Aside from this, the expression HTRA1 gene was also found to be activated under oxidative stress thus, offering a protective barrier from cell death but at the same time, boosting early senescence [9]. This functional property of the HTRA1 gene could explain the enhanced expression of this protein in conditions relating to both wet and dry AMD lesions in the older age group [10].
ARMS2 gene encodes a hypothetical protein whose function may very likely be involved in the complement system, thus mediating the clearance of cellular debris due to apoptosis and/or necrosis [11]. It is highly expressed in placental and retinal tissues. A single-nucleotide polymorphism (SNP) known as rs10490924, maps to exon 1 of the ARMS2 gene changes putative amino acid 69 from alanine to serine (A69S) which alters the ARMS2 protein [12]. Notably, ARMS2 directly interacts with fibulin-6 (hemicentin-1) and mutations in the fibulin-6 gene were previously demonstrated to cause familial AMD [13].
Therefore, it is imperative to conduct studies in different populations to draw firm conclusions about the role of genetic factors in AMD. This prompted us to investigate whether the previously reported major risk alleles in the HTRA1, ARMS2 and CFH genes are associated with AMD in the multi-ethnic Malaysian population.
Subjects, materials and methods
Subject selection and recruitment
This study was approved by the Universiti Malaya Medical Centre (UMMC) Ethical Committee (Institutional Review Board), Kuala Lumpur, Malaysia, following the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use—Good Clinical Practice guideline and the Declaration of Helsinki (Reference No.: 757.48). Written informed consent was obtained from patients before they were enrolled on this study. Two groups of 103 patients with AMD and 102 control subjects were recruited in the duration of 12 months (Jan–Dec 2011) from the outpatient clinic of the Department of Ophthalmology, UMMC. All subjects were examined by a retinal surgeon and were subjected to a standard ophthalmic examination, including visual acuity measurement, slit lamp biomicroscopy, and dilated fundi examination. Coloured fundoscopy photos were taken for all these subjects and were interpreted by a second retinal surgeon for the AMD categories to avoid operator-dependent variability. Patients with confirmed cases of AMD based on a standardized set of diagnostic criteria established by the Age-Related Eye Disease Study (AREDS) categories 2, 3 and 4 were included in the study [14].
Briefly, those patients who have early stage of the disease with multiple small drusen, single or non-extensive intermediate drusen (63–124 µm), RPE pigmentary abnormalities, or any combination of these in one or both eyes and visual acuity of 20/30 or better in both eyes is considered as AMD category 2. While those patients who exhibited mid-stage disease with at least one eye having visual acuity of 20/30 or better and one large drusen (125 µm), extensive intermediate drusen, or geographic atrophy that did not involve the macula or any combination of these is considered AMD category 3. On the other hand, those patients with advanced AMD with substantial choroidal neovascularisation or geographic atrophy involving the macula in one or both eyes are considered AMD category 4. Further, patients who had AMD fulfilling category 4 by the AREDS had fluorescein and indocyanine green fundus angiography. On this basis, those individuals without evident signs of AMD, displaying no drusen, pigmentary abnormalities, or other notable retinal changes, and has a visual acuity of 20/30 or better in both eyes and consequently, were excluded from the study.
While the control cohort consisted of age-matched volunteers without visual impairment, no family history of AMD and no macular drusen or exhibited any clinical evidence of retinal disorder. Exclusion criteria for both cohorts include subjects with any eye disease, retinopathy, or media opacities. Further, subjects with mixed ancestry were excluded from the study to minimise the population stratification effects. In this cohort, the individuals of Indian descent exclusively belonged to the South Indian ancestry group.
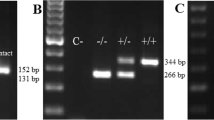
Genotyping analysis of the three SNPs: HTRA1 rs11200638, ARMS2 rs10490924 and CFH rs1061170
Blood samples were collected from all participants and the genomic DNA was extracted from the peripheral venous blood of each participant using QIAamp®DNA Minikit (Qiagen, Germany) according to the manufacturer’s protocol. PCR reactions were performed using a PCR thermal cycler (Biometra, Germany) in 50 μl PCR reaction tubes containing 100–250 ng of genomic DNA, 1X Taq buffer with KCl, 2.5 mM of MgCl, 200 μM of dNTPs, 8% dimethylsulfoxide, 1 unit of Taq DNA polymerase (Fermentas, USA) and 20 pmol of each forward and reverse primers. All primer sequences for the HTRA1, ARMS2 and CFH genes were sourced from Xu et al. [15]. Thirty-five cycles of amplification were carried out with standard PCR protocol at an annealing temperature of 55 °C for HTRA1 and ARMS2 and 53 °C for CFH gene for all reactions for 30 s. Direct DNA sequencing of the HTRA1, ARMS2 and CFH genes was carried out using ABI Prism Gene Sequencer, Model 3100, version 3.7 at Research Biolabs in Singapore, in duplicates. The genotyping process was conducted with the individuals deliberately unaware of the sample identities, ensuring a blinded approach to minimize bias or influence during the genotyping procedures.
Data analyses
The genetic Hardy–Weinberg equilibrium (HWE) of HTRA1, ARMS2 and CFH genes in cases and controls were calculated using Genepop version 4.2 population genetics software package [16]. The Statistical Package for Social Sciences version 26.0 (IBM, New York, USA) was used to analyse the data. One-sample Kolmogorov–Smirnov test was used to assess that a variable is normally distributed. The student’s t-test was used to compare means between the cases and controls for all data sets that showed normal distribution. Chi-square (X2) and/or Fisher’s exact tests were used for association studies between the HTRA1, ARMS2 and CFH gene polymorphisms and susceptibility to AMD, where applicable. Odds ratios (OR) and 95% confidence intervals (CI) were calculated as a relative measure of effect and the level of uncertainty around the measure of effect, respectively. A p value of less than 0.05 was considered statistically significant. The parameters for power calculation for HTRA1 and ARMS2 association studies, respectively, were set as follows using genetic power calculator [17].
High-risk allele frequency A/T set at | 0.5 |
Prevalence set at | 7% |
Genotype relative risk GA/GT | 1 |
Genotype relative risk AA/TT | 3 |
D-prime | 1 |
Marker allele frequency G | 0.5 |
Number of cases | 100 |
Control: case ratio | 1 |
Type I error | 0.05 |
Required sample size at power | 0.80 |
With that, the power for HTRA1 and ARMS2 chi-squared tests were 95% each, at 5% Type I error, using 100 cases and 100 controls.
Results
A total of 205 subjects were enrolled on this study; n = 103 subjects were with AMD whilst, n = 102 subjects represent the age-matched control group (Table 1). There was no significant association between groups of subjects and gender as well as ethnicity (Table 1). Additionally, upon employing the AREDS-based criteria [14] for the classification of AMD subjects, it was similarly observed that there was no statistically significant association between the groups of subjects and their respective ethnicities (Table 2).
The genotype and allele frequencies of the HTRA1, ARMS2 and CFH gene polymorphism among subjects with AMD and controls are tabulated in Table 3. Genotype distributions for SNPs at gene loci HTRA1, ARMS2 and CFH were in HWE (Table 3). The SNPs rs11200638: G > A in HTRA1 and rs10490924: G > T in ARMS2 promoter regions were significantly associated with AMD. The frequencies of the risk allele A in the former SNP were found significantly higher among those with AMD cases compared to controls whilst, similar risk T allele frequencies were observed in the ARMS2 gene (Table 3). A significant difference was found in the HTRA1 and ARMS2 genotype frequencies between AMD cases and controls (Table 3). On the other hand, no differences were observed in the genotypic and allelic frequencies of CFH variant Y402H between the groups of subjects (Table 3).
Table 4 demonstrates a joint genotypes association testing by using 9 possible combinations of ARMS2 and (followed by) HTRA1 genotypes in the groups of subjects demarcated according to the ethnicities of the subjects. The results showed that the genotype combination of TT AA of ARMS2 and HTRA1 was significantly associated with the susceptibility to AMD among the Malaysian Chinese and Indian ethnic groups compared to the control subjects, respectively (Table 4). However, the frequencies of combined genotypes of ARMS2 and HTRA1 were statistically similar between patients with AMD and controls among the Malaysian Malay ethnic group (Table 4), which may have resulted due to a relatively smaller sample size in this subpopulation.
Figure 1 demonstrates the age profile of patients who have the TT genotype for the ARMS2 gene and the three possible genotypes AA, GA, and GG for the HTRA1 locus. Patients with AMD appeared to have mostly AA and GA genotypes, whilst the control subjects, had GG genotypes. Despite being relatively advanced in age, the four control subjects belonging to the Chinese ethnic group who have the GG genotype for the HTRA1 gene did not develop AMD. Interestingly, we did have a relatively young subject (51 years old) in the control Malaysian Indian ethnic sub-group carrying the TT and AA genotypes for the ARMS2 and HTRA1 gene loci. Given the results of the present study that have shown a significant association between the genotypic combination of TT AA of ARMS2 and HTRA1 and susceptibility to AMD among the Malaysian Indian ethnic groups, it would be very interesting to follow up if this subject would develop AMD as time progresses.
Discussion
The main objective of this study was to examine if the major risk alleles in the HTRA1, ARMS2 and CFH genes were associated with AMD in the multi-ethnic Malaysian population. Wide inter-population variations of alleles of HTRA1, ARMS2 and CFH genes were observed, worldwide (Tables 5A-C). The distribution of alleles of HTRA1, ARMS2 and CFH genes in the Malaysian pooled population was generally comparable to other Asian populations (Tables 5, 6, and 7), except for a few studies involving CFH gene polymorphism [18,19,20]. The variation of alleles found in HTRA1, and ARMS2 genes observed in the present study were also similarly reported by Mohamed et al. [21], an antecedent study in which the treatment efficacies of ranibizumab among patients with neovascular AMD among Malaysians was examined thus, indicating our study was not biased neither by subject selection nor stratification effects.
Our study showed significant associations between the HTRA1 and ARMS2 variants with AMD in the Malaysian population. This is consistent with previous studies published across a wide range of other populations worldwide including the Chinese [15, 19, 25, 27, 40], Korean [26], Japanese [24, 32], Indian [18, 20], Thai [23], Pakistani [33], Caucasian [6, 28,29,30, 35], Middle Easterners [31, 41], Hispanic [34, 36, 42] and African [34] populations (Tables 5 and 6). Nevertheless, there are indeed subtle differences in the outcome of the analysis in part due to the differences in experimental/study design, subject’s inclusion criteria, grading of AMD, etc. in these studies. For example, the definition of cases and controls for the association analysis varies (Tables 5, 6, and 7), as some had categorized the subjects into the early and late stage of AMD or, wet and dry AMD whilst, this study rather took a more generalized view regardless of the stage of presentation. Aside from this, the diagnostic criterion of the present study was based on the AREDS (14, Table 2) whilst few other studies [18, 36, 37] had opted for either Wisconsin Age-Related Maculopathy Grading System, International Age-related Maculopathy Epidemiological Study Group or, Clinical Age-Related Maculopathy System. On the same note, there were also studies with no discernible diagnostic criteria mentioned [6, 20] or genotyping results [22].
ARMS2 and HTRA1 are both located in the chromosome 10q26 region, where the SNP rs11200638 resides (with T allele) in the promoter region of the HTRA1 gene (also known as PRSS11, NM_002775) and is approximately 6.1 kb downstream of the ARMS2 rs10490924 locus (with A allele). It was previously reported that both HTRA1 and ARMS2 SNPs appear to contribute equally to the increased disease risk [2]. An analysis by the AMD Gene Consortium reported that both the HTRA1 and the nearby ARMS2 SNP locus are in strong linkage disequilibrium [43]. However, both studies did not state whether the HTRA1 or ARMS2 is the causal gene in this locus. Since these two genes’ loci are in proximity, it is difficult to tell whether changes in one gene or another or possibly changes in both accounts for the increased disease risk. Although the polymorphism of Tyr402His in CFH rs1061170 has been identified as a common variant and a major genetic risk factor for AMD development, it did not appear to increase the risk of AMD in this Malaysian cohort. The collaborative genome-wide association study reported stronger evidence of the CFH variant for disease association among Europeans but a lower association among East Asians when stratified based on ancestry [43]. This also explains the consistently low frequencies of the risk-C allele in Asian populations except for a few studies [18,19,20, 33] (Table 7). In this study, we reported a null association for risk-C allele between the case and control groups of subjects (Table 3) as well as when they were further stratified according to three different Malaysian ethnic subgroups including Chinese as well as Indian and Malay (Table 4).
As observed among the Malaysian Chinese subjects, similar null association results were also reported in multiple other independent studies conducted in China [15, 37] and Japan [32, 44]. In addition, in agreement with the hypothesized significant ethnic differences in minor allele frequencies of Tyr402His [38], this variant was also not associated with AMD in the Mexican Zapotecos individuals [36], who also showed similar frequencies of C risk-allele (0.04) as that of the Japanese [45] and Chinese [37] populations. In contrast, Quan et al. [46] reported strong evidence for an association between CFH gene polymorphism and AMD in the Chinese population with a pooled C allele frequency of 0.05, via a meta-analysis study. Albeit studying a similar cohort of Chinese, contrasting results of the association study between the investigations of Chen et al. [37] and Quan et al. [46] is very likely due to the inclusion of subjects from various geographic areas of China comprised of 56 different ethnicities in the latter study, hence, a diverse genetic background. Aside from this, sample size, as well as the sampling frame, may also play a role in such inconclusive results [4].
In contrast to the null association between the CFH gene and AMD in the Malaysian Indian cohort found in this study (data not shown), Sharma et al. [39] and Kaur et al. [20] on the other hand, had reported otherwise among subjects with late stages of AMD in the North and South Indian population, respectively. In another study, Sundaresan et al. [18] investigated by including subjects hailing from the North and South regions of India with both early and late stages of AMD. Consistent with the prior-mentioned studies [20, 39], in this study too, an association was found between the CFH gene polymorphism and late stage of AMD. When the Malaysian Indian ethnic subpopulation harbouring AMD was further demarcated into early and late stages of AMD, we found that 19 subjects were diagnosed with an early stage of AMD (categories 2 and 3 of AREDS) whilst the remaining 11, are those with late stage (category 4 of AREDS, Table 2). Hence, we postulated that the lack of association between AMD and CFH gene polymorphism in the Malaysian Indian cohort in the present study might be due to the presence of the majority of subjects with early-stage of AMD. Nonetheless, the absence of an association with CFH gene polymorphism within the Malaysian Indian population is highly suggestive of alternative molecular pathways for the development of early AMD when compared with the Caucasian population.
Limitations of the study
A small sample size is the main limitation of this study particularly, when the subjects were further stratified according to their ethnic origins, such as Malaysian Chinese, Indian and Malay (Table 4). This is because when a small sample size is used, there is a high possibility that the observations observed would be due to chance hence, the estimates stemming from the study may be unintentionally biased. Given this, the data of the present study need to be carefully interpreted. Nevertheless, the number of recruits in each ethnic-based sub-group reflects the racial distribution of patients visiting the UMMC eye clinic.
Secondly, since the prevalence of AMD varies substantially between ethnicity/population, the inclusion of subjects from diversified ethnic origins in the initial analysis may have impeded the true reflection of the disease risk and variants of the genes examined. Nonetheless, we believe that this study has value as an investigation of AMD genotype–phenotype correlation and that these data can contribute to the body of knowledge as well as serve as a starting point for future prospective studies evaluating such associations in a larger multi-ethnic Malaysian population.
Thirdly, is the lack of study’s focus on the clinical outcomes in AMD (e.g., types, severity). This is because the study’s primary objective was to explore the genetic associations and genotype–phenotype correlations. However, indeed, this omission restricts the comprehensive understanding of how AMD manifests within various ethnic groups. Understanding the clinical nuances, including types and severity, is pivotal as it could offer crucial insights into tailored treatment approaches and disease management strategies specific to each ethnicity. Acknowledging this limitation underscores the necessity for future research to encompass not only genetic associations but also the diverse clinical presentations of AMD across ethnic populations for a more holistic understanding and improved patient care.
Conclusion
In summary, we have found significant associations between SNPs at HTRA1 and ARMS2 genes and AMD in the Malaysian population. However, there was no association of AMD with CFH gene polymorphism was found. These findings suggest that the sequence of pathways by which AMD develops in the Malaysian population may differ from those present in European populations but are consistent with our Asian counterparts. Nevertheless, the AMD genotype–phenotype correlations observed in this study need to be further validated in a clinically representative multi-ethnic Malaysian population particularly, by considering other genetic risk alleles associated with AMD development as well as confounding factors including diet (e.g., vitamins C and E, beta carotene, and zinc supplements), lifestyle (e.g., smoking status), epigenetics, environmental conditions, and the presence of other co-morbidities.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AMD:
-
Age-related macular degeneration
- AREDS :
-
Age-related eye disease study
- ARMS2 :
-
Age-Related Maculopathy Susceptibility 2 Gene
- CFH :
-
Complement Factor H Gene
- CI:
-
Confidence intervals
- HTRA1 :
-
Human High-Temperature Requirement A-1 Gene
- HWE :
-
Hardy–Weinberg equilibrium
- OR:
-
Odd ratios
- PCR:
-
Polymerase chain reaction
- SD:
-
Standard deviation
- SNP:
-
Single-nucleotide polymorphism
- Tyr:
-
Tyrosine
- UMMC:
-
Universiti Malaya Medical Centre
- X 2 :
-
Chi-square test
References
Wang W, Gawlik K, Lopez J, Wen C, Zhu J, Wu F et al (2016) Genetic and environmental factors strongly influence risk, severity and progression of age-related macular degeneration. Sig Transduct Target Ther 1(1):16016
Deangelis MM, Silveira AC, Carr EA, Kim IK (2011) Genetics of age-related macular degeneration: current concepts, future directions. Semin Ophthalmol 26(3):77–93
Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY et al (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2(2):e106–e116
Cheung CM, Tai ES, Kawasaki R, Tay WT, Lee JL, Hamzah H et al (2012) Prevalence of and risk factors for age-related macular degeneration in a multiethnic Asian cohort. Arch Ophthal 130(4):480–486
Kuo JZ, Wong TY, Ong FS (2013) Genetic risk, ethnic variations and pharmacogenetic biomarkers in age-related macular degeneration and polypoidal choroidal vasculopathy. Expert Rev Ophthalmol 8(2):127–140
Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ et al (2006) A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration. Science 314(5801):992–993
DeWan A, Liu M, Hartman S, Zhang SS-M, Liu DTL, Zhao C et al (2006) HTRA1 promoter polymorphism in wet age-related macular degeneration. Science 314(5801):989
Mohamedmohaideen NN, Palaninathan SK, Morin PM, Williams BJ, Braunstein M, Tichy SE et al (2008) Structure and function of the virulence-associated high-temperature requirement A of Mycobacterium tuberculosis. Biochemistry 47(23):6092–6102
Supanji, Shimomachi M, Hasan MZ, Kawaichi M, Oka C (2013) HTRA1 is induced by oxidative stress and enhances cell senescence through p38 MAPK pathway. Exp Eye Res 112:79–92
Clausen T, Southan C, Ehrmann M (2002) The HTRA family of proteases: Implications for protein composition and cell fate. Mol Cell 10(3):443–455
Micklisch S, Lin Y, Jacob S, Karlstetter M, Dannhausen K, Dasari P et al (2017) Age-related macular degeneration associated polymorphism rs10490924 in ARMS2 results in deficiency of a complement activator. J Neuroinflam 14(1):4
Kanda A, Chen W, Othman M, Branham KE, Brooks M, Khanna R et al (2007) A variant of mitochondrial protein LOC387715/ARMS2, not HTRA1, is strongly associated with age-related macular degeneration. PNAS 104(41):16227–16232
Kortvely E, Hauck SM, Duetsch G, Gloeckner CJ, Kremmer E, Alge-Priglinger CS et al (2010) ARMS2 is a constituent of the extracellular matrix providing a link between familial and sporadic age-related macular degenerations. Invest Ophthalmol Vis Sci 51(1):79–88
Age-Related Eye Disease Study Research Group (2001) A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthal 119(10):1417–1436
Xu Y, Guan N, Xu J, Yang X, Ma K, Zhou H et al (2008) Association of CFH, LOC387715, and HTRA1 polymorphisms with exudative age-related macular degeneration in a northern Chinese population. Mol Vis 14:1373–1381
Rousset F (2008) Genepop’007: a complete re-implementation of the genepop software for Windows and Linux. Mol Ecol Resour 8(1):103–106
Purcell S, Cherny SS, Sham PC (2003) Genetic power calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 19(1):149–150
Sundaresan P, Vashist P, Ravindran RD, Shanker A, Nitsch D, Nonyane BA et al (2012) Polymorphisms in ARMS2/HTRA1 and complement genes and age-related macular degeneration in India: findings from the INDEYE study. Invest Ophthalmol Vis Sci 53(12):7492–7497
Tian J, Yu W, Qin X, Fang K, Chen Q, Hou J et al (2012) Association of genetic polymorphisms and age-related macular degeneration in Chinese population. Invest Ophthalmol Vis Sci 53(7):4262–4269
Kaur I, Katta S, Hussain A, Hussain N, Mathai A, Narayanan R et al (2008) Variants in the 10q26 gene cluster (LOC387715 and HTRA1) exhibit enhanced risk of age-related macular degeneration along with CFH in Indian patients. Invest Ophthalmol Vis Sci 49(5):1771–1776
Mohamad NA, Ramachandran V, Mohd Isa H, Chan YM, Ngah NF, Ching SM et al (2019) Association of HTRA1 and ARMS2 gene polymorphisms with response to intravitreal ranibizumab among neovascular age-related macular degenerative subjects. Hum Genomics 13(1):13
Conroy SW, Supanji M, Sasongko BM (2018) Identifikasi single nucleotide polymorphism (SNP) gen HTRA1 pada age- related macular degeneration (AMD) di Indonesia: Studi deskriptif: Universitas Gadjah Mada
Ruamviboonsuk P, Tadarati M, Singhanetr P, Wattanapokayakit S, Kunhapan P, Wanitchanon T et al (2017) Genome-wide association study of neovascular age-related macular degeneration in the Thai population. J Hum Genet 62(11):957–962
Mori K, Horie-Inoue K, Kohda M, Kawasaki I, Gehlbach PL, Awata T et al (2007) Association of the HTRA1 gene variant with age-related macular degeneration in the Japanese population. J Hum Genet 52(7):636–641
Ng TK, Liang XY, Lai TYY, Ma L, Tam POS, Wang JX et al (2016) HTRA1 promoter variant differentiates polypoidal choroidal vasculopathy from exudative age-related macular degeneration. Sci Rep 6(1):28639
Lee SJ, Kim NR, Chin HS (2010) LOC387715/HTRA1 polymorphisms, smoking and combined effects on exudative age-related macular degeneration in a Korean population. Clin Exp Ophthalmol 38(7):698–704
Jiang H, Qu Y, Dang G, Zhang X, Yin N, Zhang Y et al (2009) Analyses of single nucleotide polymorphisms and haplotype linkage of LOC387715 and the HTRA1 gene in exudative age-related macular degeneration in a Chinese cohort. Retina 29(7):974–979
Matušková V, Zeman T, Ewerlingová L, Hlinomazová Z, Souček J, Vlková E et al (2020) An association of neovascular age-related macular degeneration with polymorphisms of CFH, ARMS2, HTRA1 and C3 genes in Czech population. Acta Ophthalmol. https://doi.org/10.1111/aos.14357
Weger M, Renner W, Steinbrugger I, Köfer K, Wedrich A, Groselj-Strele A et al (2007) Association of the HTRA1 -625G>A promoter gene polymorphism with exudative age-related macular degeneration in a Central European population. Mol Vis 13:1274–1279
Liutkeviciene R, Vilkeviciute A, Gedvilaite G, Kaikaryte K, Kriauciuniene L (2019) Haplotypes of HTRA1 rs1120638, TIMP3 rs9621532, VEGFA rs833068, CFI rs10033900, ERCC6 rs3793784, and KCTD10 rs56209061 gene polymorphisms in age-related macular degeneration. Dis Mark 2019:9602949
Chowers I, Cohen Y, Goldenberg-Cohen N, Vicuna-Kojchen J, Lichtinger A, Weinstein O et al (2008) Association of complement factor H Y402H polymorphism with phenotype of neovascular age related macular degeneration in Israel. Mol Vis 14:1829–1834
Tanimoto S, Tamura H, Ue T, Yamane K, Maruyama H, Kawakami H et al (2007) A polymorphism of LOC387715 gene is associated with age-related macular degeneration in the Japanese population. Neurosci Lett 414(1):71–74
Ayub H, Shafique S, Azam A, Muslim I, Qazi NA, Akhtar F et al (2019) Association of rs10490924 in ARMS2/HTRA1 with age-related macular degeneration in the Pakistani population. Ann Hum Genet 83(4):285–290
Spencer KL, Glenn K, Brown-Gentry K, Haines JL, Crawford DC (2012) Population differences in genetic risk for age-related macular degeneration and implications for genetic testing. Arch Ophthal 130(1):116–117
Ross RJ, Bojanowski CM, Wang JJ, Chew EY, Rochtchina E, Ferris FL 3rd et al (2007) The LOC387715 polymorphism and age-related macular degeneration: replication in three case–control samples. Invest Ophthalmol Vis Sci 48(3):1128–1132
Contreras AV, Zenteno JC, Fernandez-Lopez JC, Rodriguez-Corona U, Falfan-Valencia R, Sebastian L et al (2014) CFH haplotypes and ARMS2, C2, C3, and CFB alleles show association with susceptibility to age-related macular degeneration in Mexicans. Mol Vis 20:105–116
Chen LJ, Liu DT, Tam PO, Chan WM, Liu K, Chong KK et al (2006) Association of complement factor H polymorphisms with exudative age-related macular degeneration. Mol Vis 12:1536–1542
Grassi MA, Fingert JH, Scheetz TE, Roos BR, Ritch R, West SK et al (2006) Ethnic variation in AMD-associated complement factor H polymorphism p.Tyr402His. Hum Mutat 27(9):921–925
Sharma NK, Gupta A, Prabhakar S, Singh R, Sharma SK, Chen W et al (2013) Association between CFH Y402H polymorphism and age related macular degeneration in North Indian cohort. PLoS ONE 8(7):e70193
Zhuang W, Li H, Liu Y, Zhao J, Ha S, Xiang W et al (2014) Association of specific genetic polymorphisms with age-related macular degeneration in a Northern Chinese population. Ophthal Genet 35(3):156–161
Askari M, Nikpoor AR, Gorjipour F, Mazidi M, Sanati MH, Aryan H et al (2015) Association of Htra1 gene polymorphisms with the risk of developing AMD in Iranian population. Rep Biochem Mol Biol 4(1):43–49
Martínez-Velasco A, Perez-Ortiz AC, Zenteno JC, Luna-Angulo AB, Villa-Romero AR, Martínez-Villaseñor L et al (2017) CFH and HTRA1 genes associated with AMD in Mexican population. Invest Ophthalmol Vis Sci 58(8):2268
Fritsche LG, Chen W, Schu M, Yaspan BL, Yu Y, Thorleifsson G et al (2013) Seven new loci associated with age-related macular degeneration. Nat Genet 45(4):433–439
Gotoh N, Yamada R, Hiratani H, Renault V, Kuroiwa S, Monet M et al (2006) No association between complement factor H gene polymorphism and exudative age-related macular degeneration in Japanese. Hum Genet 120(1):139–143
Okamoto H, Umeda S, Obazawa M, Minami M, Noda T, Mizota A et al (2006) Complement factor H polymorphisms in Japanese population with age-related macular degeneration. Mol Vis 12:156–158
Quan YL, Zhou AY, Feng ZH (2012) Association between complementary factor H Y402H polymorphisms and age-related macular degeneration in Chinese: systematic review and meta-analysis. Int J Ophthalmol 5(2):242–246
Acknowledgements
We would like to acknowledge Dr Khang Tsung Fei from the Faculty of Sciences, Universiti Malaya for his contribution to the statistical analysis. This study was supported by the Ministry of Higher Education, the Fundamental Research Grant Scheme (FRGS), Malaysia (Grant Number: FP035/2010A). Also, during the preparation of this work, the author(s) have used OpenAI's ChatGPT (version 3.5) in order to improve language and readability of this manuscript. After using this tool, the author(s) have thoroughly reviewed and revised the content to ensure its accuracy and originality, taking full responsibility for the final publication.
Funding
This study was supported by the Ministry of Higher Education, the Fundamental Research Grant Scheme (FRGS), Malaysia (Grant Number: FP035/2010A).
Author information
Authors and Affiliations
Contributions
FI: Conceptualization, Methodology, Formal analysis, Visualization, Investigation, Writing—Original Draft, Writing—Review & Editing, Approved the final draft. SMJ: Conceptualization, Resources, Writing—Review & Editing, Supervision, Project administration, Funding acquisition, Approved the final draft. LCC: Methodology, Writing—Original Draft, Approved the final draft. JJJ: Formal analysis, Visualization, Writing—Original Draft, Writing—Review & Editing, Visualization, Approved the final draft. VS: Conceptualization, Resources, Writing—Review & Editing, Supervision, Project administration, Funding acquisition, Approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the UMMC Ethical Committee (Institutional Review Board) following the ICH-GCP guideline and the Declaration of Helsinki (Reference No.: 757.48). Written informed consent was obtained from patients before they were enrolled on this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ismail, F., Junit, S.M., Chin, L.C. et al. Association of ARMS2, HTRA1 and CFH genes polymorphisms in patients with age-related macular degeneration in the Malaysian population. Egypt J Med Hum Genet 25, 79 (2024). https://doi.org/10.1186/s43042-024-00549-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-024-00549-8