Abstract
Background
Inter-individual variations in the clinical manifestations of SARS-CoV-2 infection are among the challenging features of COVID-19. The known role of telomeres in cell proliferation and immune competency highlights their possible function in infectious diseases. Variability in telomere length is an invaluable parameter in the heterogeneity of the clinical presentation of diseases.
Result
In this study, our aim was to investigate the possible association between leukocyte telomere length (LTL) and COVID-19 severity. LTL was measured in 100 patients with moderate and severe forms of COVID-19 using the quantitative PCR (q-PCR) method. Statistical analysis confirmed a strong inverse correlation between relative LTL and COVID-19 severity.
Conclusions
These findings suggest that LTL can be a useful parameter for predicting disease severity in patients, as individuals with short telomeres may have a higher risk of developing severe COVID-19.
Similar content being viewed by others
Introduction
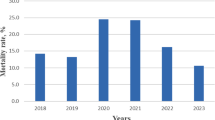
Severe acute respiratory syndrome coronavirus (SARS-CoV)-2 first emerged in Wuhan City, China, in late December 2019. The World Health Organization announced “COVID-19” as the name of this dangerous and deadly disease. Within a short period of time, the COVID-19 pandemic has spread with alarming speed and threatens millions of people around the world [1]. SARS-CoV-2 is an enveloped virus with a positive-sense, single-stranded RNA genome of 29.8 kb. There are different scenarios for the origin of the virus; however, phylogenetic analyses have shown that this virus has likely originated by sequential recombination of bat SARS-CoVs [2, 3]. Epidemiological investigations have demonstrated that SARS-CoV-2 affects all ages, but elderly people with underlying diseases are more susceptible. A systematic review of Chinese cases reported a 3.2% case fatality rate, ranging from 2 to 4% for COVID-19. However, higher age and preexisting comorbid conditions were described as the main risk factors for mortality in this study [4, 5]. The clinical spectrum of COVID-19 is highly heterogeneous, ranging from asymptomatic to acute respiratory distress syndrome and multi-organ dysfunction. SARS-CoV-2 mainly infects the respiratory system, but recent findings have revealed that, besides the respiratory system, the circulatory system, liver, immune system, urogenital system, myocardial, gastrointestinal, renal system, and even the central nervous system could be the target organs for infection [6, 7]. Lymphopenia is one of the common features of COVID-19, which is a decline in the numbers of CD4/CD8 T cells but not B cells. Comprehensive systematic literature searches of online databases have revealed that the significant reduction of T cell count is a hallmark of severe COVID-19. The current results propose that lymphopenia at the initial presentation of COVID-19 is linked poor prognosis in patients [8, 9].
Telomeres are located at the ends of linear chromosomes and are composed of distinct protein elements that bind to telomeric DNA. These nucleoprotein structures protect the chromosomal ends from DNA breaks and preserve the stability of the genome. In most cell types, the continuous shortening of telomeres occurs during cell division due to the incomplete replication of chromosomal ends. Maintenance of telomere length is critical for the efficient proliferation of cells, and therefore telomere length dynamics play a critical role in the biology of diseases [10]. Regardless of chronological aging, several physiological, environmental, and behavioral factors such as smoking, lack of physical activity, obesity, exposure to hazardous air pollutants, stress, childhood adversities, and major depressive disorder can potentially increase the rate of telomere shortening [11, 12].
Leukocyte telomere length (LTL) is a heritable and complex polygenic trait with large inter-individual variation [13]. Genome-wide association studies (GWAS) implicate the involvement of at least eight different gene loci in LTL [14,15,16,17,18,19]. Based on our present knowledge, short telomeres limit immune cells’ ability to proliferate. There is an interconnecting relationship between shortening of LTL and lymphopoiesis. Telomere attrition to a critical and threshold length can limit the proliferative capacity of immune cells. Shorter LTL is tightly coupled with increased synthesis of proinflammatory cytokines, poorer immune responses to infections, and consequently the development of severe disease [20]. Findings from a cohort study on healthy young and midlife adults demonstrated that shorter CD8CD28− T cell telomere length is associated with increased risk for experimentally induced acute upper respiratory tract infection and clinical illness [21]. Additionally, several studies have highlighted the significant association of shorter telomeres with increased severity of COVID-19 [22,23,24,25,26]. Based on the above, the susceptibility to viral infections with respect to telomere length is not a new idea. Therefore, in this replication study, we attempted to investigate the possible relationship between LTL and the severity of COVID-19 in our population.
Materials and methods
Subjects
This study was conducted on 50 intubated adult patients patients, comprising 22 female and 28 male patients with ages ranging from 26 to 91 years old, who were admitted to the ICU with severe COVID-19 infection. Additionally, 50 individuals, comprising 22 female and 28 male patients with ages ranging from 31 to 88 years old, who were hospitalized with moderate COVID-19, were included. The groups were gender matched. Blood samples were collected from May to July 2022, during which the Omicron strain was the dominant variant of the virus in Iran [27].
The key steps involved in identifying and enrolling eligible participants included a positive nasopharyngeal reverse transcription polymerase chain reaction (RT-PCR) test and the presence of symptoms. Participants were 18 years or older. We classified disease severity based on clinical symptoms, breathing problems, and radiological features. Patients with COVID-19 were considered to have severe illness if they had SpO2 < 90% on room air at sea level, a respiratory rate > 30 breaths/min, PaO2/FiO2 < 200 mm Hg, or lung infiltrates > 60. Patients were considered to have moderate illness if they had SpO2 < 94% on room air at sea level, a respiratory rate > 25 breaths/min, 200 < PaO2/FiO2 < 300 mm Hg, or 60 > lung infiltrates > 30. We investigated five comorbid conditions including hypertension (HTN), type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), chronic obstructive pulmonary disease (COPD) and chronic kidney disease (CKD) in patients with COVID-19.
DNA isolation and quantitative PCR (q-PCR)
Blood samples were obtained on the first day of admission from all patients. Genomic DNA was extracted from buffy-coat samples using the QIAamp 96 DNA Blood Kit by Qiagen (Hilden, Germany) and stored at − 20 °C. Next, the quantity and purity of the DNA were assayed using a NanoDrop 2000 spectrophotometer (Thermo Scientific, Wilmington, DE, USA), and all DNA samples had OD260/OD280 values of 1.7–2.1. The DNA samples were stored at − 80 °C until further use. The relative measurement of the LTL was carried out by the quantitative polymerase chain reaction (qPCR)-based assay according to a method described by Cawthon [28] with small modifications. A specially designed oligonucleotide primer set hybridized to genomic DNA and amplified telomeric DNA. For accurate and reliable relative telomere length analysis, we normalized the results of the telomere reaction using a specific single-copy gene, 36B4 gene, which encodes an acidic ribosomal phosphoprotein P0 (RPLP0). Briefly, the final reaction mixture contained 5 ng of buffy-coat-derived genomic DNA, 5 µl of SYBR Green master mix (Applied Biosystems), 300 nM of forward and 300 nM of reverse primers, and enough double-distilled water to yield a 10 µl reaction. For each DNA sample, two consecutive reactions were performed with the following primer pairs for the telomeric sequence and housekeeping gene. The list of primers used in this study is summarized in Table 1. The thermal cycle conditions of each qPCR analysis were set at 95 °C for 10 min, followed by 25 cycles of 10 s at 95 °C, 120 s at 56 °C for the amplification of the telomeric sequence, and for 36B4 PCR, followed by 30 cycles of 10 s at 95 °C, 60 s at 58 °C. All assays were carried out in triplicates. Each reaction also contained a 6-point standard curve from 0.625 to 20 ng using pooled buffy-coat-derived genomic DNA. The acceptable standard deviation (s.d.) of the triplicate threshold cycle (Ct) values was set at 0.3. The telomere repeat copy number to single-gene copy number (T/S) ratio was calculated using the following equation: − ΔCt (ΔCt = CtTel − Ct36B4). The relative average telomere length was determined using the Rotor-Gene quantification software in a Rotor-Gene 3000 real-time System.
Statistical analysis
The normal distribution of quantitative data was evaluated using the Kolmogorov–Smirnov test. In the presence of a normal distribution, the correlation between data was assessed using the Pearson test. If the normal distribution was not followed, the Spearman test was used instead. Differences between quantitative data were analyzed using the Mann–Whitney test. The predictive effect of telomere length on the severity of COVID-19 was evaluated using binary logistic regression models with a forward stepwise selection process. All statistical analyses were performed using GraphPad Prism software version 8. A p-value under 0.05 was considered significant.
Results
This article aims to assess the role of telomere length in COVID-19 severity. As expected, we observed a strong inverse correlation between relative LTL and COVID-19 severity. However, our results suggest that there is no significant association between gender, smoking status, and comorbidities in terms of the relative length of telomeres in patients with moderate and severe forms of COVID-19. Our findings indicate a strong negative correlation between telomere length and age of patients with the severe and moderate forms of COVID-19. The present data revealed no significant association between hospitalization duration, occurrence of septic shock, and death with the relative length of telomeres in the subject groups. Finally, related clinical characteristics were compared between two groups of patients with moderate and severe COVID-19 and revealed that there was no significant difference regarding gender, smoking, comorbidities and age (p-value = 0.99, 0.79, 0.06 and 0.54, respectively). See supplementary material (Additional file 1: Table S1) for supporting content.
Telomere length was associated with the severity of COVID-19
To evaluate the association between the severity of COVID-19 disease, gender, smoking status, and comorbidities with the length of telomeres, we used the Student t-test. Based on the data (Fig. 1A), the relative length of telomeres in patients with severe form of COVID-19 was significantly shorter than those affected with moderate COVID-19 disease (p-value = 0.005).
There was no significant difference between men and women in terms of the relative length of telomeres in patients with moderate and severe forms of COVID-19 disease (Fig. 1B) (p-value = 0.141 and 0.259, respectively).
According to our data, no significant association was found between current or ex-smokers and non-smokers regarding the relative length of telomeres in patients with moderate and severe forms of COVID-19 disease (p-value = 0.19 and 0.61, respectively; Fig. 1C).
Finally, the investigation revealed no significant association between the length of telomeres and comorbidities in patients with moderate and severe forms of COVID-19 disease (p-value = 0.40 and 0.92, respectively; Fig. 1D).
Additionally, logistic regression analysis was performed to evaluate the predicting value of variables regarding the severity of COVID-19 disease. Based on the univariate logistic regression analysis, telomere length and comorbidities were regarded as significant predictors of COVID-19 severity. Multivariate logistic regression analysis showed that telomere length, along with age, had significant predictive values regarding the severity of COVID-19 disease in our study population (Table 2).
Telomere length was inversely correlated with age in both severity groups
We used the Pearson test for COVID-19 patients with moderate severity due to the normal distribution of age data and the Spearman test for COVID-19 patients with the severe form of the disease to measure the correlation between telomere length, assessed by quantitative PCR, and age of the patients.
Our findings revealed a strong negative correlation between telomere length and age of COVID-19 patients with moderate severity (r = − 0.79; p < 0.0001) (Fig. 2A). The same type of correlation was found between telomere length and age of patients with the severe type of COVID-19 (r = − 0.82; p < 0.0001). Therefore, the present data showed a significant correlation between the telomeres shortening and the advanced age of the COVID-19 patients, and this correlation was stronger in patients with the severe form of the disease.
Also, evaluating the overall correlation of telomere length with age and length of hospitalization of patients (regardless of disease severity) showed that the age of patients with COVID-19 had a strong and significant inverse correlation with telomere length (r = − 0.79, p-value = 0.00021), while the duration of hospitalization of COVID-19 patients had a relatively weak inverse but significant correlation with telomere length (r = − 0.23, p-value = 0.01).
We also evaluated the correlation between telomere length and hospitalization duration in COVID-19 patients with moderate and severe forms of the disease using Spearman analysis. Our results showed that there was no correlation between telomere length and hospitalization duration in moderately affected COVID-19 patients (r = − 0.02; p = 0.82) and also in patients with the severe form of COVID-19 (r = − 0.16; p = 0.24) (Fig. 2B).
Telomere length was not associated with septic shock and death
Finally, we assessed the possible association of telomere length with the occurrence of septic shock and death in patients with the severe form of COVID-19. As shown in Fig. 3, the present data revealed no significant association between the length of telomeres and the occurrence of septic shock (p = 0.84) (Fig. 3A), or death (p = 0.98) (Fig. 3B), in patients who were affected by the severe form of the disease.
Discussion
Our approach in this study was to test the association between leukocyte telomere length (LTL) and the severity of COVID-19 in 100 Iranian patients. These findings showed that the telomere length in patients with a severe form of COVID-19 is significantly shorter than those with a moderate form of the disease.
The nine tentative hallmarks of aging include genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and altered intercellular communication. Telomere attrition or shortening is one of the most well known of these hallmarks. Chronological and biological aging, as well as environmental factors, can affect the rate of telomere attrition [29]. Immunosenescence is a complex phenomenon characterized by dynamic changes occurring in innate and adaptive immune systems, leading to the accumulation of senescent immune cells, subsequently causing the progressive decline in immune system function [30]. Increased levels of circulating pro-inflammatory cytokines [31], reduced percentage of naive lymphocytes [32], and telomere shortening [33] are the main age-associated changes in the immune system and play pivotal roles in reducing immune competency in humans. According to our current knowledge, the cytokine storm is associated with severity and death in COVID-19 patients [34]. Although the promotion of massive lymphopoiesis is crucial for the successful clearance of viral infections, a drastically reduced number of circulating lymphocytes, lymphopenia, has been introduced as a reliable prognostic marker for COVID-19 severity [35]. The survival, proliferation, and maturation of lymphocytes in bone marrow, thymus, and secondary lymphoid organs are tightly coupled with telomere length [36]. Longitudinal follow-up studies on telomere shortening have revealed a heterogeneous pattern in the rate of telomere shortening among individuals [37, 38]. Short telomeres in leucocytes are associated with immune dysfunction and many chronic diseases. Experimental exposure to rhinovirus in healthy young and midlife adults showed a significant association between shorter CD8CD28− cell telomere length and upper respiratory tract infection and clinical illness [21]. Based on a simplified hypothesis, Aviv discussed the possible role of LTL in COVID-19 severity and mortality [39]. Our recent study suggested that telomere attrition and epigenetic alterations are the main predictors of biological aging and cellular senescence that can influence the severity of COVID-19 [40]. A recent study showed a significant association between LTL and lymphopenia among elderly patients with COVID-19 [41]. Two separate studies on LTL in patients demonstrated that the risk of developing severe COVID-19 is higher in individuals with short telomere length in peripheral leukocytes [23, 26]. Additionally, a comparison of LTL in 53 individuals without COVID-19 and patients with different clinical severity showed that patients with the severe form of COVID-19 had the shortest LTL. In comparison with the subjected individuals without COVID-19 and mild groups, patients with moderate COVID-19 had a shorter LTL. No significant differences were reported in LTL between negative and mild groups [42].A cohort study on 6775 participants in the UK Biobank demonstrated the association between shorter LTL and a higher risk of developing severe COVID-19 [25]. In our study, we confirmed a significant inverse correlation between relative LTL and age of COVID-19 patients. Severe patients showed a stronger inverse correlation between relative LTL and age compared to moderate patients. There is also a significant association between relative LTL and COVID-19 severity. According to these findings, individuals with short telomeres have a higher risk of developing severe COVID-19.
Several studies have shown that baseline LTL varies with sex and genetic background. Males have shorter overall LTL and higher attrition rates [43, 44]. However, in our study, there was not enough statistical evidence to show sex-specific associations between telomere length and moderate and severe COVID-19 patients. The differences in methodology (Flow-FISH or qPCR) or statistical analysis (quantile or linear regression) may explain the controversial results of the median LTL between sexes. Therefore, further research needs to be done to better understand this phenomenon [45].
Despite the biological links, smoking habits can affect LTL dynamics among individuals. A systematic review of 84 studies showed that ever smokers had shorter telomeres compared to those who never smoked. Current smokers also had shorter telomeres compared to former smokers [46]. A recent random-effects meta-analysis introduced smoking as a risk factor for the progression of COVID-19; therefore, smoking-control strategies can be effective in blunting the COVID-19 pandemic [47]. However, based on our findings, there was no statistically significant association between smoking and LTL in either moderate or severe COVID-19 patients. Further research on all clinical spectrums of COVID-19, ranging from asymptomatic to mild, moderate, severe, and critical disease, is needed. The results of two different studies suggested that telomere length is associated with a greater risk of developing a critical disease, such as being admitted to ICU or death without ICU. These studies indicated that shorter LTL can influence the severity of COVID-19 [23, 42]. However, in a recent study analyzing telomere length in a cohort of severe hospitalized COVID-19 patients, the role of telomere length was supported as a potential risk factor for hospitalization in COVID-19, but not for in-hospital complications nor persistent post-COVID-19 manifestations [48]. In the present study, we did not detect a significant association between LTL and hospitalization duration or more severe outcomes such as the occurrence of septic shock or death, in hospitalized patients with moderate and severe forms of COVID-19. Therefore, the number of people we included in the study was too small to provide convincing evidence, and further comprehensive research can provide more precise estimates of the effects of LTL on hospitalization duration, the occurrence of septic shock, or death.
A recent bidirectional Mendelian randomization study revealed that there is no significant association between LTL and COVID-19 [49]. The limitations of this study may explain these controversial results. The current research has only focused on hospitalized COVID-19 patients with moderate to severe disease without any specific trends in age, sex, or race/ethnicity. Additionally, the differences in methodology or statistical analysis can affect the results. Therefore, these limitations can serve as an opportunity to identify new gaps, and consequently, new research. Although the power of the main hypothesis of the study was acceptable, the results of the subgroup analysis might be influenced by the relatively low power of the study in subgroups.
Conclusion
The assessment of leukocyte telomere length (LTL) in moderate and severe COVID-19 patients revealed that telomere length was associated with the severity of COVID-19. However, it was not associated with smoking status, hospitalization duration, or clinical implications such as the occurrence of septic shock or hospital mortality. This study paves the way for further investigations on LTL as a potential prognostic factor for COVID-19. Understanding the causes of inter-individual variations in COVID-19 outcomes can provide new insights into potential targets of telomerase activation and personalized therapeutic interventions.
Availability of data and materials
Data and materials are available upon request.
References
Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. The lancet 395(10223):470–473
Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R (2020) COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res 24:91
Wu A, Peng Y, Huang B et al (2020) Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe 27(3):325–328
Clark A, Jit M, Warren-Gash C et al (2020) Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 8(8):e1003–e1017
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323(13):1239–1242
Sheervalilou R, Shirvaliloo M, Dadashzadeh N et al (2020) COVID-19 under spotlight: a close look at the origin, transmission, diagnosis, and treatment of the 2019-nCoV disease. J Cell Physiol 235(12):8873–8924
Zhang Y, Geng X, Tan Y et al (2020) New understanding of the damage of SARS-CoV-2 infection outside the respiratory system. Biomed Pharmacother 127:110195
Huang I, Pranata R (2020) Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J Intensive Care 8:1–10
Zhao Q, Meng M, Kumar R et al (2020) Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a systemic review and meta-analysis. Int J Infect Dis 96:131–135
Bojesen SE (2013) Telomeres and human health. J Intern Med 274(5):399–413
Srinivas N, Rachakonda S, Kumar R (2020) Telomeres and telomere length: a general overview. Cancers 12(3):558
Starkweather AR, Alhaeeri AA, Montpetit A et al (2014) An integrative review of factors associated with telomere length and implications for biobehavioral research. Nurs Res 63(1):36
Honig LS, Kang MS, Cheng R et al (2015) Heritability of telomere length in a study of long-lived families. Neurobiol Aging 36(10):2785–2790
Codd V, Mangino M, Van Der Harst P et al (2010) Common variants near TERC are associated with mean telomere length. Nat Genet 42(3):197–199
Delgado DA, Zhang C, Chen LS et al (2018) Genome-wide association study of telomere length among South Asians identifies a second RTEL1 association signal. J Med Genet 55(1):64–71
Levy D, Neuhausen SL, Hunt SC et al (2010) Genome-wide association identifies OBFC1 as a locus involved in human leukocyte telomere biology. Proc Natl Acad Sci 107(20):9293–9298
Mangino M, Christiansen L, Stone R et al (2015) DCAF4, a novel gene associated with leucocyte telomere length. J Med Genet 52(3):157–162
Mangino M, Hwang S-J, Spector TD et al (2012) Genome-wide meta-analysis points to CTC1 and ZNF676 as genes regulating telomere homeostasis in humans. Hum Mol Genet 21(24):5385–5394
Prescott J, Kraft P, Chasman DI et al (2011) Genome-wide association study of relative telomere length. PLoS ONE 6(5):e19635
Dodig S, Čepelak I, Pavić I (2019) Hallmarks of senescence and aging. Biochem Med 29(3):483–497
Cohen S, Janicki-Deverts D, Turner RB et al (2013) Association between telomere length and experimentally induced upper respiratory viral infection in healthy adults. JAMA 309(7):699–705
Aviv A (2021) Short telomeres and severe COVID-19: the connection conundrum. EBioMedicine. https://doi.org/10.1016/j.ebiom.2021.103513
Froidure A, Mahieu M, Hoton D et al (2020) Short telomeres increase the risk of severe COVID-19. Aging (Albany NY) 12(20):19911
Tsilingiris D, Tentolouris A, Eleftheriadou I, Tentolouris N (2020) Telomere length, epidemiology and pathogenesis of severe COVID-19. Eur J Clin Investig 50(10):e13376
Wang Q, Codd V, Raisi-Estabragh Z et al (2021) Shorter leukocyte telomere length is associated with adverse COVID-19 outcomes: a cohort study in UK Biobank. EBioMedicine 70:103485
Sanchez-Vazquez R, Guío-Carrión A, Zapatero-Gaviria A, Martínez P, Blasco MA (2021) Shorter telomere lengths in patients with severe COVID-19 disease. Aging (Albany NY) 13(1):1
Olfatifar M, Shojaee S, Sabokbar T, Pourhoseingholi MA (2022) Predicting the status of the new strain of coronavirus, omicron, in Iran for the next 4 months. Canon J Med 3(1):1–2
Cawthon RM (2002) Telomere measurement by quantitative PCR. Nucl Acids Res 30(10):e47-e
Oeseburg H, de Boer RA, van Gilst WH, van der Harst P (2010) Telomere biology in healthy aging and disease. Pflügers Archiv-Eur J Physiol 459(2):259–268
Gruver A, Hudson L, Sempowski G (2007) Immunosenescence of ageing. J Pathol: J Pathol Soc Great Br Irel 211(2):144–156
Ferrucci L, Corsi A, Lauretani F et al (2005) The origins of age-related proinflammatory state. Blood 105(6):2294–2299
Sansoni P, Cossarizza A, Brianti V, et al (1993) Lymphocyte subsets and natural killer cell activity in healthy old people and centenarians [see comments]
Weng N-p (2012) Telomeres and immune competency. Curr Opin Immunol 24(4):470–475
Hu B, Huang S, Yin L (2021) The cytokine storm and COVID-19. J Med Virol 93(1):250–256
Tan L, Wang Q, Zhang D et al (2020) Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Sign Transduct Target Ther 5(1):1–3
Weng N-P, Levine BL, June CH, Hodes RJ (1995) Human naive and memory T lymphocytes differ in telomeric length and replicative potential. Proc Natl Acad Sci 92(24):11091–11094
Chen W, Kimura M, Kim S et al (2011) Longitudinal versus cross-sectional evaluations of leukocyte telomere length dynamics: age-dependent telomere shortening is the rule. J Gerontol Ser A: Biomed Sci Med Sci 66(3):312–319
Lin Y, Damjanovic A, Metter EJ et al (2015) Age-associated telomere attrition of lymphocytes in vivo is co-ordinated with changes in telomerase activity, composition of lymphocyte subsets and health conditions. Clin Sci 128(6):367–377
Aviv A (2020) Telomeres and COVID-19. FASEB J 34(6):7247–7252
Mahmoodpoor A, Sanaie S, Roudbari F, Sabzevari T, Sohrabifar N, Kazeminasab S (2022) Understanding the role of telomere attrition and epigenetic signatures in COVID-19 severity. Gene 811:146069
Benetos A, Lai T-P, Toupance S et al (2021) The nexus between telomere length and lymphocyte count in seniors hospitalized with covid-19. J Gerontol: Ser A 76(8):e97–e101
Dos Santos GA, Pimenta R, Viana NI et al (2021) Shorter leukocyte telomere length is associated with severity of COVID-19 infection. Biochem Biophys Rep 27:101056
Berglund K, Reynolds CA, Ploner A et al (2016) Longitudinal decline of leukocyte telomere length in old age and the association with sex and genetic risk. Aging (Albany NY) 8(7):1398
Mayer S, Brüderlein S, Perner S et al (2006) Sex-specific telomere length profiles and age-dependent erosion dynamics of individual chromosome arms in humans. Cytogenet Genome Res 112(3–4):194–201
Gutierrez-Rodrigues F, Alves-Paiva RM, Scatena NF, Martinez EZ, Scheucher PS, Calado RT (2022) Association between leukocyte telomere length and sex by quantile regression analysis. Hematol Transfus Cell Ther 44:346–351
Astuti Y, Wardhana A, Watkins J, Wulaningsih W (2017) Cigarette smoking and telomere length: a systematic review of 84 studies and meta-analysis. Environ Res 158:480–489
Patanavanich R, Glantz SA (2020) Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res 22(9):1653–1656
Retuerto M, Lledó A, Fernandez-Varas B et al (2022) Shorter telomere length is associated with COVID-19 hospitalization and with persistence of radiographic lung abnormalities. Immun Ageing 19(1):1–9
Huang D, Lin S, He J, Wang Q, Zhan Y (2022) Association between COVID-19 and telomere length: a bidirectional Mendelian randomization study. J Med Virol 94(11):5345–5353
Acknowledgements
Not applicable.
Funding
This work was supported by Tabriz University of Medical Sciences [Grant code 65846].
Author information
Authors and Affiliations
Contributions
AM and SS conceived and designed the study and revised the manuscript. ME, NB and MT helped sample collection. FR revised the manuscript. NS analyzed, interpreted the data and drafted the manuscript. BE and SK performed the research, drafted and provided final approval of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Tabriz University of medical sciences (IR.TBZMED.REC.1399.542). All participants signed the informed consent.
Consent for publication
Consent to publish had been obtained from all participants, and all authors agree to publish this paper.
Competing interests
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Table S1: Clinical characteristics were compared between two groups of patients with moderate and severe COVID-19, and revealed that there was no significant difference regarding age, gender, comorbidities, and smoking.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmoodpoor, A., Sanaie, S., Eskandari, M. et al. Association between leukocyte telomere length and COVID-19 severity. Egypt J Med Hum Genet 24, 37 (2023). https://doi.org/10.1186/s43042-023-00415-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00415-z