Abstract
Background
Stratification analysis studies showed that ethnicity has a significant association regarding MTHFR C677T variant and congenital heart diseases (CHDs) risk, and many published studies have controversial conclusions toward this association.
Methods
In this study, the association between the MTHFR C677T variant and the risk for CHDs was evaluated in 91 children with CHD and 95 healthy controls, as new cases, by using restriction fragment length polymorphism (RFLP) technique. Besides that, 2 case–control studies in the Egyptian population published before 2021 were included in this meta-analysis. The association was assessed by the odds ratio (OR) with a 95% confidence interval (CI) based on 294 alleles in CHD cases and 286 alleles in controls.
Results
The overall meta-analysis showed a significant association between MTHFR C677T variant and CHDs risk in Egyptian children with heterogeneity (Heterogeneity = 0.001) in all the genetic models with the highly significant association in T versus C allele (pooled OR 1.89, 95% CI 1.31–2.74; p value < 0.0004). The consistency of the genotypes was detected by Hardy–Weinberg equilibrium (HWE).
Conclusions
Our results support the MTHFR -677T allele as a susceptibility factor for CHDs in the Egyptian pediatric patients.
Similar content being viewed by others
Background
A congenital heart defect is a common heart disease leading to a high mortality rate in newborns [1]. With an estimated prevalence rate of 8.6–10.3 per 1000 live births and growing, congenital heart disease (CHD) is the most prevalent birth defect [2]. Folic acid considers a key player in the development of the cardiovascular system, where reduced maternal folic acid leads to elevated homocysteine in the blood as a toxic material, which has been described as a potential risk factor for CHDs [3,4,5].
The 5,10-methylenetetrahydrofolate reductase (MTHFR), encoded by the MTHFR gene, is an important enzyme in homocysteine metabolism, converting 5,10-methylenetetrahydrofolate into 5-methyltetrahydrofolate in the process of methyltetrahydrofolate, and the MTHFR C677T variant reduces the activity of the MTHFR enzyme increasing plasma homocysteine level. The homozygous 677TT and heterozygous 677CT genotypes lead to approximately 30% and 65% of the enzyme activity reduction in MTHFR, respectively, compared with the 677CC genotype [6].
Although there are enormous studies that have been pointed to a relationship between C677T and the risk of CHD, the conclusion is still inconsistent, especially regarding the participants’ ethnicity, sample size, and limited statistical analysis. On the Egyptian population, there are three distinct case–control studies that were done and published on the PubMed database [7,8,9]. Thus, to provide more consistency and comprehensive results, an updated meta-analysis approach was applied in the current study for all published data (until Jan 2021) and our cases data of Egyptian conotruncal heart and cardiac septal defects patients including 900 alleles (454 patients alleles and 446 controls one) to evaluate the association between MTHFR C677T variant and CHD susceptibility.
Methods
Samples collection
Our prospective study included 91 children with CHDs and 95 controls. Participants were recruited from the Clinical Genetics Clinic, National Research Centre. The study was approved by the Ethics Committee of National Research Centre (NRC) under Decision No. 19257, and a written informed consent was obtained from the parents. Patients with known syndromic CHDs were excluded. All participants were examined for general appearance and genetic syndromes. Full anthropometric measurements including weight, length, and skull circumference were recorded. Full clinical and cardiac examinations were conducted for each case including personal and family history, pedigree analysis, and clinical examination for all systems with special emphasis on heart evaluation. Cardiac investigations were done including chest x-ray, Echocardiogram, and ECG for each case. Conotruncal heart and cardiac septal defects were diagnosed based on clinical evaluation and cardiac investigations. Our control group was selected as healthy children who were not appearing observational syndromic features by clinicians' examination or cardiac anomalies by ECHO investigation.
MTHFR C677T genotyping by PCR–RFLP
Venous blood was collected into EDTA vacutainer tubes and was stored in − 80C. DNA was extracted by iNtRON G-spin total DNA extraction kit (50 preps), catalogue number 17045, Korea (https://www.intronbio.com/eg/). The C677T polymorphism was genotyped by PCR–RFLP. To determine the genotype of the MTHFR gene, genomic DNA was amplified through PCR by using specific primers. The MTHFR C677T primer sequences are as follows: forward, 5′-CATCCCTATTGGCAGGTTACCC -3' and reverse, 5'- GGGAAGAACTCAGCGAACTCAG -3'. The PCR amplifications were performed in a total volume of 35 µL, which consisted of 10 pmol of each primer, Master Mix and template DNA. Thermal cycling conditions were 94°C for 3 min, followed by 35 cycles at 94°C for 30 s, 58°C for 30 s and 72°C for 30 s, and a final extension at 72°C for 3 min. The PCR products were digested with 2–4 units of restriction enzyme, Hinf I at 37°C for 1 h in 10 × Fast Digest Buffer at a final volume of 30 µL. The restriction patterns of the PCR products were determined via separation on 3% ethidium bromide agarose gels according to Table 1.
Identification and eligibility of relevant studies
We conducted an electronic search for relevant articles published before Jan 2021 in PubMed databases with the combination of the following terms: “congenital cardiac/heart defects,” “conotruncal heart defects” “MTHFR,” “polymorphism/mutation or variant,” “C677T” and “Egypt or Egyptian.”
Data extraction of the eligible studies
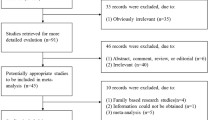
All data were extracted independently by two authors (Fayez, Alaaeldin, and Esmaiel, Nora). And a third investigator reviewed the result. The extraction of eligible study data included the following: a first author, publication year, Egypt country of origin, Arabian ethnicity, number of cases and controls, genotype frequency, counts of alleles in case and control groups, Hardy–Weinberg equilibrium (HWE), PCR–RFLP method only to eliminate method effect, and case–control studies from 2010 to 2021. Animal studies, reviews, short communication, case reports, and mixed population were excluded. To support our results reliability, the studies with deviated genotype frequency distribution according to recalculated HWE score were not eligible to pass in the further statistical analysis.
Statistical analysis
In each of the included studies, we calculated again Hardy–Weinberg equilibrium (HWE) in controls of each included study using a Chi-square goodness of fit test in order to test the hypothesis that the observed genotype frequencies do not differ from their expected values, P ≤ 0.05 as considered significant level. We calculated odds ratios (ORs) and its 95% confidence intervals (95% CIs) to estimate the associations between MTHFR polymorphisms and CHDs susceptibility. The pooled ORs and 95% CIs were calculated in five genetic models: allele model (T versus C), heterozygote model (TC versus CC), homozygote model (TT versus CC), dominant model (TT + TC versus CC), and recessive model (TT versus TC + CC). The significance of the pooled OR was considered statistically significant at P ≤ 0.05. Heterogeneity across the eligible studies was tested using x2-based Cochran’ Q-test in which heterogeneity was considered significant at P < 0.1; When the effects were assumed to be homogeneous, the fixed-effects model was used; otherwise, the random-effects model was more appropriate. All analyses were performed using SPSS software, release 18.0.0
Results
Characteristics of the included participants and studies
The cardiac diagnosis of our clinically examined participants is listed in Table 2. Our literature search identified 3 publications according to the inclusion term criteria. According to recalculated HWE scores as shown in Table 3, we removed Zidan et al. [8] study because its genotype distributions in the control group were deviating from HWE law. Therefore, two out of three retrieved publications were considered in the followed meta-analysis work. Thus, the participants in this meta-analysis study involved pooled 147 (294 alleles) cases and 143 (286 alleles) controls. The included cases involve two categories of CHDs (conotruncal heart defects with septal defects (mixed) and conotruncal heart defects only). In El-Abd et al. [9] and Kotby et al. [7], the equilibrium of the genotype distributions in controls was detected according to Hardy–Weinberg Equilibrium (HWE) test, and all values are shown in Table 3. Consideration of patients' sex and age comparison was not permitted because that the descriptive data of the study population regarding sex and age were not completely cited in all included publications.
The association between MTHFR C677T variant and CHDs risk; T allele is a risk factor for CHDs
Three digestion patterns of the amplified MTHFR C677T fragment in our cases shown in Fig. 1. Through extracted datasets from our participants and 2 studies of the MTHFR C677T polymorphism in Egyptian CHDs children and underestimated T versus C frequency, significant heterogeneity was detected (Pheterogeneity < 0.01), thus the random-effects model was employed. Compared to the C allele, the T allele conferred a pooled OR of 1.89 (95% CI 1.31–2.74 at p value = 0.0004) in the allelic model (Fig. 2). To assess the effect of each study on the pooled OR estimate, a sensitivity analysis was applied. The result showed the pooled ORs for the allelic model were similar before and after elimination of each study (Table 4). Investigating the potential source of heterogeneity was not done to limit the included publications and their characteristic data. Nevertheless, significant associations between MTHFR C677T polymorphism and the risk of CHDs were observed as shown in Table 5.
Digestion patterns of 318 bps amplicon containing C677T site showing (i) normal allele pattern (677CC) with intact 318 bps fragment in cases 5, 6, 7, 9, 10, and 12, (ii) heterozygous mutant allele pattern (C677T) with 318, 227, and 91 bps fragments in cases 2, 3, 4, 11, and 13, (iii) homozygous mutant allele pattern (677TT) with 227 and 91 bps fragments in cases 1 and 8. (M) lane represents ΦX174 DNA/HaeIII Marker
Discussion
CHDs are serious genetic conditions with almost unknown etiology, and there are no established strategies for reducing their public health impact. Single nucleotide polymorphisms (SNPs) in several genes, such as Notch1, GATA4, NKX2-5, TBX5, and others, have been shown to be significantly linked to the risk of CHDs. However, the MTHFR gene is one of the commonly associated potential genes with the risk of CHDs [2].
MTHFR gene encodes a active catalytic 77 kDa protein converting 5,10-methylenetetrahydrofolate into 5-methyltetrahydrofolate, the major circulating form of folate [6]. So, the MTHFR enzyme activity regulates 5-methyltetrahydrofolate synthesis, and hence, the process of remethylation of homocysteine to methionine is affected inducing hyperhomocysteinemia. Specifically, the MTHFR C677T variant leads to increase plasma homocysteine [10, 11], where C677T is one of the common variants in MTHFR gene located at the folate binding site [12]. The folate–homocysteine metabolic pathway has role in neural tube formation and cardiogenesis, where low folate and high homocysteine levels are a closely related to congenital heart defects traits [13]. Therefore, we performed a case–control study including 186 participants and an updated meta-analysis on Egyptian CHD patients. Our selection to encompass our original study with subsequent meta-analysis due to being meta-analysis integrates results from the original and subsequent replication studies increasing the statistical power to detect gene–disease associations.
Kapusta et al. [14] concluded a first report that maternal hyperhomocysteinemia is correlated with an increased risk of CHDs. Hobbs et al. [15] studied mothers whose pregnancies were affected by congenital heart defects, and they found that homocysteine, S-adenosylhomocysteine, and methionine are most important biomarkers predictive of case or control status. Recently, Raina et al. [16] pointed that a significant role of MTHFR C677T in increased risk of CHD. It is importantly that Newborns can be protected from various congenital abnormalities by maternal uptake folic acid supplement, and this including decrease CHD risk by 40–60% [6].
Our recent meta-analysis demonstrated that the MTHFR C677T variant is associated with the risk of congenital heart defects in Egyptian neonatal patients. Across Egyptian CHD patients, several case–control studies were performed on the association of MTHFR variants with CHDs susceptibility, out of the three studies recruited Egyptian CHDs children [7,8,9], showing uninformative results. Although the genotyping bias was detected in two studies out of them, associations between infant MTHFR C677T variant and the risk of CHDs were detected across all genetic inheritance models. The mode of action of the MTHFR C677T variant might be different across ethnicities according to what was reported in Wang [17].
To elucidate the differential effect of C677T variant across multiple ethnicities, we retrieved the recent relevant publications across different ethnicities. Elizabeth et al. [18] reported that an association between the MTHFR C677T variant is high risk in Indians CHD patients especially in South Indians, whereas Raina et al. [16] concluded lack of association for MTHFR C677T with risk of CHD in Jammu & Kashmir Indians. Mamasoula [19] analyzed MTHFR C677T genotyping on 5814 CHD cases and 10,056 controls in the European and Australian populations across meta-analysis study; they found no significant effect of MTHFR C677T genotyping on CHD risk. Wang et al. [20] and Shi et al. [21] concluded that maternal MTHFR C677T increase in risk of given birth of a CHDs children and frequency of maternal TT allele was significantly higher in affected group than control one. In Iranian CHD patients, Noori et al. [22] found that TT allele was considered highest risk for CHDs especially VSD phenotype (OR 10, 95% CI 1–92.2, P = 0.04).
Herein, we intend to include Egyptian children only to exclude the ethnicity effect. Regarding that MTHFR C677T variant is relevant to increase the risk of CHD as concluded in the current study, the previous studies showed that MTHFR C677T variant may lead to hyperhomocysteinemia and consequently reduced folic acid level causing high risk factor for CHDs [23,24,25]. Some studies reported that the MTHFR C677T variant was just associated with a specific phenotype of CHDs [26, 27], suggesting that the results of the current meta-analysis should be interpreted cautiously.
Based on our meta-analysis, we found that the T allele of the MTHFR C677T variant is relevant to increasing the risk of CHDs in all genetic inheritance models, and the association was more significant in the dominant model than the recessive one.
Our selection to gather conotruncal heart and cardiac septal defects in one patients group due to our observation that mixed conotruncal heart and cardiac septal defects patients is comparable with controls in different studies, where in Xuan et al. [28], the authors carried out a meta-analysis for 9329 cases and 15,076 controls which were extracted from 35 publications from year 2001 to 2014 involving different ethnicities. It is worth to mention that our observation revealed that 28 out of 35 publications had been included mixed patients from conotruncal heart and cardiac septal defects; however, the pooled children' genotypes and alleles showed significant association in all C677T model inheritance.
It well known that deviated HWE scores in a human control population can be caused by multiple reasons such as technical problems in genotyping, inbreeding caused by consanguinity, population size effect, natural factors, and hidden population structure, and consistent HWE supports to a real link between the targeted genotypes and the corresponding trait [29]. Herein, except Zidan et al. [8] study, all recalculated HWE scores were consistent supporting potential reliable link between MTHFR C677T and CHD.
Conclusions
Our meta-analysis demonstrated a potentially significant association of the MTHFR C677T variant with CHD risk. The current meta-analysis study has limitations as (1) all 3 studies were collected only from the PubMed database, so other relevant studies might be cited in other databases, (2) the current study included the Egyptian CHDs children only without their mothers, (3) all 3 studies have limited information regarding cases characterization, (4) several gene variants may act together as haplotype block or protein–protein interaction with MTHFR C677T variant, and finally, (5) there are some hidden factors, such as environmental conditions, lifestyle or gender may affect.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available upon request.
References
Garg V, Kathiriya IS, Barnes R et al (2003) GATA4 mutations cause human congenital heart defects and reveal an interaction with TBX5. Nature 424:443–447
Sun M, Wang T, Huang P et al (2021) Association analysis of maternal MTHFR gene polymorphisms and the occurrence of congenital heart disease in offspring. BMC Cardiovasc Disord 21:298. https://doi.org/10.1186/s12872-021-02117-z
Christensen KE, Zada YF, Rohlicek CV et al (2013) Risk of congenital heart defects is influenced by genetic variation in folate metabolism. Cardiol Young 23:89–98
Fredriksen A, Meyer K, Ueland PM et al (2007) Large-scale population-based metabolic phenotyping of thirteen genetic polymorphisms related to one-carbonmetabolism. Hum Mutat 28:856–865
Hu ZB, Shi YY, Mo XM et al (2013) A genome-wide association study identifies two risk loci for congenital heart malformations in Han Chinese populations. Nat Genet 45:818–821
Biselli PM, Guerzoni AR, de Godoy MF et al (2010) Genetic polymorphisms involved in folate metabolism and concentrations of methylmalonic acid and folate on plasma homocysteine and risk of coronary artery disease. J Thromb Thrombolysis 29:32–40
Kotby A, Anwar M, El-Masry O et al (2012) Genetic variants in the methylenetetrahydrofolate reductase gene in Egyptian children with conotruncal heart defects and their mothers. Maced J Med Sci 5:78–84
Zidan HE, Rezk NA, Mohammed D (2013) MTHFR C677T and A1298C gene polymorphisms and their relation to homocysteine level in Egyptian children with congenital heart diseases. Gene 529(1):119–124. https://doi.org/10.1016/j.gene.2013.07.053
El-Abd DM, Said RN, Hanna BM et al (2012) Maternal and offspring methylenetetrahydrofolate reductase gene C677T polymorphism: does it influence the prevalence of congenital heart defects in Egyptian neonates? Comp Clin Pathol 23:317–322
Sayin Kocakap BD, Sanli C, Cabuk F et al (2015) Association of MTHFR A1298C polymorphism with conotruncal heart disease. Cardiol Young 25:1326–1331
Shivkar RR, Gawade GC, Padwal MK et al (2022) Association of MTHFR C677T (rs1801133) and A1298C (rs1801131) polymorphisms with serum homocysteine, folate and vitamin B12 in patients with young coronary artery disease. Indian J Clin Biochem 37:224–231
Goldmuntz E et al (2008) Variants of folate metabolism genes and the risk of conotruncal cardiac defects. Circ Cardiovasc Genet 1:126–132
Zhang R, Huo C, Wang X et al (2018) Two common MTHFR gene polymorphisms (C677T and A1298C) and fetal congenital heart disease risk: an updated meta-analysis with trial sequential analysis. Cell Physiol Biochem 45:2483–2496
Kapusta L et al (1999) Congenital heart defects and maternal derangement of homocysteine metabolism. J Pediatr 135:773–774
Hobbs CA, James SJ, Jernigan S et al (2005) Congenital heart defects and abnormal maternal biomarkers of methionine and homocysteine metabolism. Am J Clin Nutr 81:147–153
Raina JK, Panjaliya RK, Dogra V et al (2022) Association of MTHFR and MS/MTR gene polymorphisms with congenital heart defects in North Indian population (Jammu and Kashmir): a case-control study encompassing meta-analysis and trial sequential analysis. BMC Pediatr 22(1):223. https://doi.org/10.1186/s12887-022-03227-z
Wang W, Wang Y, Gong F et al (2013) MTHFR C677T polymorphism and risk of congenital heart defects: evidence from 29 case-control and TDT studies. PLoS ONE. 8(3):e58041. https://doi.org/10.1371/journal.pone.0058041
Elizabeth KE, Praveen SL, Preethi NR et al (2017) Folate, vitamin B12, homocysteine and polymorphisms in folate metabolizing genes in children with congenital heart disease and their mothers. Eur J Clin Nutr 71(12):1437–1441
Mamasoula C, Prentice RR, Pierscionek T et al (2013) Association between C677T polymorphism of methylene tetrahydrofolate reductase and congenital heart disease: meta-analysis of 7697 cases and 13,125 controls. Circ Cardiovasc Genet 6(4):347–353
Wang L, Yang B, Zhou S et al (2018) Risk factors and methylenetetrahydrofolate reductase gene in congenital heart disease. J Thorac Dis 10(1):441–447
Shi H, Yang S, Lin N et al (2020) Study on maternal SNPs of MTHFR gene and HCY level related to congenital heart diseases. Pediatr Cardiol 42:42–46
Noori N, Miri-Moghaddam E, Dejkam A et al (2017) Are polymorphisms in MTRR A66G and MTHFR C677T genes associated with congenital heart diseases in Iranian population? Casp J Intern Med 8(2):83–90
Burgoon JM, Selhub J, Nadeau M et al (2002) Investigation of the effects of folate deficiency on embryonic development through the establishment of a folate deficient mouse model. Teratology 65:219–227
Wald DS, Law M, Morris JK (2002) Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ 325:1202
Feng Y, Wang S, Chen R et al (2015) Maternal folic acid supplementation and the risk of congenital heart defects in offspring: a meta-analysis of epidemiological observational studies. Sci Rep 5:8506
Marinho C, Alho I, Guerra A et al (2009) The methylenetetrahydrofolate reductase gene variant (C677T) as a susceptibility gene for tetralogy of Fallot. Rev Port Cardiol 28:809–812
Kuehl K, Loffredo C, Lammer EJ et al (2010) Association of congenital cardiovascular malformations with 33 single nucleotide polymorphisms of selected cardiovascular disease-related genes. Birth Defects Res A Clin Mol Teratol 88:101–111
Xuan C, Li H, Zhao JX et al (2014) Association between MTHFR polymorphisms and congenital heart disease: a meta-analysis based on 9,329 cases and 15,076 controls. Sci Rep 4(4):7311
Royo JL (2021) Hardy Weinberg equilibrium disturbances in case-control studies lead to non-conclusive results. Cell J 22(4):572–574
Acknowledgements
First of all, we want to thank our God for his support and help us in this research. The authors are grateful to the patients and family members for their kind participation. They also thank their family and friends in their institution for their helps and support.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NN and AG contributed to the study conception and design. EA collected the clinical data and conducted the investigations. MO and SA supervised the full clinical and manuscript revisions. NN and GM done the Genotyping work. NN and AG performed Material preparation, data collection and analysis. AG wrote the first draft of the manuscript. All authors read and approved the final manuscript. All authors have approved the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of National Research Centre (Date December 2020../No20177). Written informed consent was obtained from the parents.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Esmaiel, N.N., Ashaat, E.A., Al-Ettribi, G.M. et al. Association between MTHFR C677T variant and risk for congenital heart defects in Egyptian children: a case–control study including meta-analysis based on 147 cases and 143 controls. Egypt J Med Hum Genet 24, 29 (2023). https://doi.org/10.1186/s43042-023-00408-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00408-y