Abstract
Background
Lung cancer remains one of the most lethal carcinomas worldwide because of its late diagnosis. One of the DNA modifications is methylation, one of the primary alterations of tumor development, consisting of fascinating indicators for cancer diagnosis. This study investigated ZMYND-8 and RARβ2 gene methylation in NSCLC as a new epigenetic tool.
Methods
First, to find out the potential diagnostic capability of ZMYND-8 and RARβ2 genes methylation, we entirely surfed DNA methylation microarrays from the Cancer Genome Atlas (TCGA) data of NSCLC samples. Additionally, we took advantage of using q-MSP in several pieces comprising NSCLC tumors and neighboring normal tissues; ZMYND-8 and RARβ2 genes methylation grades were acquired.
Results
Our finding displayed significant hypomethylation of ZMYND-8 and hypermethylation of RARβ2 in NSCLC samples compared to neighboring standard specimens, which significantly correlated with the clinical stage of malignancy. In addition, the incredible precision of ZMYND-8 and RARβ2 methylations as reliable cancer diagnosis indicators in NSCLC was confirmed, drawing the ROC curve analysis with an AUC value of 0.751 and 0.8676, respectively, for ZMYND-8 and RARβ2. Additional studies of other dominant cancer entities in TCGA displayed that RARβ2’s higher methylation degree and ZMYND-8 lower methylation degree are prevalent changes in tumor evolution which could be possibly considered as a potential diagnostic biomarkers for lung cancer.
Conclusion
Based on this study, ZMYND-8 and RARβ2 methylation are reliable biomarkers for lung cancer.
Similar content being viewed by others
Background
Global statistics show that lung cancer stands in the second position as the leading cause of death after cardiovascular diseases for both sexes, with annual 200,000 new cases and 160,000 deaths [1]. Lung cancer is known at a later stage as a result of late diagnosis, which leads to a lower ratio of five years survival rate (15%). There are two main types of lung tumors, including small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC) (Respectively 20% and 80%) [2]. One of the most critical approaches to lung cancer is timely diagnosis to implement more efficient therapies. Carcinogenesis is a collaborative interaction of genetic and epigenetic determinants resulting in the disorganization of important oncogenes, like DNA repair genes and tumor suppressor genes [3, 4].
Epigenetic alterations, including histone modifications, DNA methylation in non-coding RNA expression, play an essential role in the final phenotype of an individual cell up to the whole body; therefore, they do for the probability of cancer malignancy [5]. As a vital element in tumorigenesis, DNA methylation happens at the initial stages of cancer creation [6].
Promoter’s methylation in various tumor suppressor genes happens in the beginning stages of lung cancer formation. Adding a methyl group to the fifth place of the cytosine placed 5′ to guanosine in a CpG dinucleotide is called DNA methylation. Also, a stretch of DNA that holds excellent CpG contents is called A CpG island. Greater degrees of methylation in CpG islands of promoters bring about a structural change of the chromatin, stopping RNA polymerase and other regulatory proteins from accessing the region, therefore preventing gene transcription. The expression of the genes contributes to all stages of normal cell function was decreased by hypermethylation which led to malignancy initiation and development [7]. The bromodomain protein encoded by zinc finger MYND-type containing 8 (ZMYND-8) is a multifunctional transcription factor that acts in several different situations, including being an essential chromatin-modifying factor in many cancers and cause of mutation aberrant expression in multiple cancers [8,9,10]. ZMYND-8 regulates the expression of all transretinoic acid (ATRA)-responsive genes through specific recognition of H3K36me2/H4K16ac histon. Also, ZMYND-8 is essential in modulating chromatin integrity and DNA repair [11]. ZMYND-8 is a central epigenetic regulator that contributes to tumor suppression in many different types of cancer [12]. Modulating histone methylation and acetylation in the enhancer regions by ZMYND-8 is significant, as the dysregulation of this process may cause over-activation of transcription and contribute to tumorigenesis [9].
Retinoic acid (RA) induces growth inhibition and apoptosis mainly by regulating gene expression through its nuclear receptors, known as retinoic acid receptors (RARs) and retinoid X receptors (RXRs). Kim et al. [13] RAR and RXR proteins are encoded by three different categories of genes, including RARα, RARβ, and RARγ which have distinct functions. Heterodimers are formed by RARs and RXRs that fasten to particular RA-responsive factors (RAREs) to regulate aimed genes expression [14].
The retinoic acid receptor beta (RARβ) is extensively expressed in epithelial cells, obtains four other spliced forms, and the beta-2 form seems to keep anti-tumor activity. Based on some studies performed on transgenic mice, the expression of non-coding RARβ2 transcripts leads to tumor development contrary to control ones [14]. Additionally, several studies reporting the RARβ gene lacks expression in human carcinomas, such as H146, CALU-6, SK-MES1, H661, NCI-H23, and NCI-H125, signifying a probable link between aberrant expression of the RARβ and lung cancer evolution [15, 16]. In a recent study, RARβ could play either anti-tumor or tumor progression roles depending on how different expressed variants are joined [16].
Because of the importance of ZMYND-8 and RARβ2 genes in tumor suppression and development, the present study aimed at investigating the genes mentioned above methylation in both tumor tissue and tumor tissue margin samples of lung carcinoma.
Methods
Investigation of ZMYND-8 and RARβ2 methylation in lung cancer dataset (TCGA-STAD)
For evaluating the methylation degree of ZMYND-8 and RARβ2 genes among accessible high-performance analyses for NSCLC, we utilized The Cancer Genome Atlas Stomach Adenocarcinoma (TCGA-STAD) database. TCGA is a project sponsored by people offering a complete “atlas” of cancer gene profiles from prominent companions, including over 30 human cancers [17]. Methylation beta is worth for CpG investigators covering with ZMYND-8 and RARβ2 promoters obtained from TCGA-STAD resources were achieved using Xena Functional Genomics browser (https://xena.ucsc.edu/). To compare the methylation status of ZMYND-8 and RARβ2 genes between lung cancer tissues and normal tissues, the mean beta measurements of all CpG investigators were computed to reach a steady signal, and then these measurements were studied. What's more, the methylation grade of each CpG investigator, comprising cg13699808 and cg23662675 probes for the ZMYND-8 gene and cg26124016, cg02499249, and cg27486427 probes for the RARβ2 gene were studied to determine potentially suitable CpG locations for ZMYND-8 and RARβ2 DNA methylation.
Validation of ZMYND-8 and RARβ2 methylation in NSCLC samples
Preparation of patient samples
In this work, with a case–control plan, tissue samples of 50 patients with lung cancer and 50 healthy ones from Imam Reza Hospital were engaged and gathered from 2020 to 2021 (Table 1). This study's members were Azerbaijani people living in the northwest of Iran. The subjects with hemoptysis, prior radiotherapy or chemotherapy, tuberculosis, or patients who refused to participate in this study were excluded. After the inscribed intelligible consent was taken from all study members, the lung tissues of contributors were collected by the bronchoscopy and needle biopsy techniques as the routine parts of the patient diagnostic approach and, immediately after sampling, transferred to liquid nitrogen. The ethical confirmation of this study was issued by Tabriz University of Medical Sciences Research Ethical Committee (Ethical Code is IR.TBZMED.REC.1400.574).
Genomic DNA and bisulfite modification isolation
All included samples were crushed in liquid nitrogen mechanically, immediately after grounding, moved into a lysis buffer subsequently homogenized with a needle and syringe. Genomic DNA extraction was completed based on AllPrep DNA/RNA/Protein kit (Qiagen, Hilden, Germany) procedures. DNA purity and concentration were established by reading the absorption at the A260/A280 fraction through NanoDrop spectrophotometer (ThermoFisher Scientific Life Sciences, USA). The DNA Methylation Kit (Zymo Research cat no:D5001) was used for Bisulfite treatment [18].
Quantitative methylation-specific PCR
Methylation of the ZMYND-8 and RARβ2 promoters CpG islands was examined by quantitative methylation-specific PCR (q-MSP) in the Step One Plus Real-Time PCR machine (Applied Biosystems, USA) using BioFACT™ 2X Real-Time PCR Master Mix (Korea). The CpG islands sequences associated with ZMYND-8 and RARβ2 promoters were recovered from the UCSC genome explorer (https://genome.ucsc.edu/). The primer designing tool for ZMYND-8 and RARβ2 methylation-targeting primers was MethPrimer online (http://www.urogene.org/methprimer/). The amplification program was as follows: early denaturation at 95 °C for 15 min, 45 consecutive periods of denaturation for 10 s, the 30 s splicing at 60 °C, and 20 s incubation at 72 °C; as the ending stage of qPCR, a melting curve analysis was then performed [19]. Primer patterns used for the q-MSP test are shown in Table 2.
ROC curve and Kaplan–Meier survival analysis
To inspect ZMYND-8 and RARβ2 methylation sites as a reliable diagnostic biomarker and assess its testing precision for the distinction of NSCLC cases and healthy ones, the area below the curve (AUC) of the receiver operating characteristic (ROC) curvature was assessed according to the DNA methylation grade from TCGA-STAD resource and standard specimens. In addition, the Kaplan–Meier survival test on the TCGA-STAD methylation database was accomplished to verify whether ZMYND-8 and RARβ2 methylation is associated with the total survival of NSCLC cases.
Statistical analysis
All statistical analyses were drawn using GraphPad 6 Prism (GraphPad Software, San Diego, CA). To extract variances of ZMYND-8 and RARβ2 methylation grades between tumor tissues and neighboring normal tissues, Paired Student's t test was accomplished. The statistical analysis of the TCGA dataset was drawn through paired and unpaired t test, Mann–Whitney U test, and Log-rank (Mantel-Cox) test. P values < 0.05 were assumed statistically significant, and mean ± standard error of the experiments of data was offered.
Results
ZMYND-8 and RARβ2 methylation in NSCLC samples reclaimed from TCGA-STAD dataset
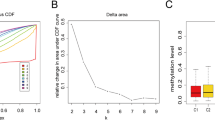
For holistic study, methylation grade of ZMYND-8 and RARβ2 genes in GC, microarray resources using the TCGA-STAD dataset were hunted and analyzed. DNA methylation outlines of 277 lung tumor tissues and 168 noncancerous lung samples were recovered from the TCGA-STAD methylation database (The Illumina HumanMethylation27 Bead Chip), consisting of cg13699808 and cg23662675 probes for ZMYND-8 gene, cg26124016, cg02499249, and cg27486427 probes for the RARβ2 gene. The outcomes from TCGA-STAD revealed the significant hypomethylation of ZMYND-8 in NSCLC (P-value < 0.0001) (Fig. 1) and hypermethylation of RARβ2 in NSCLC (P-value < 0.0001) (Fig. 2).
A ZMYND-8 methylation pattern of TCGA datasets. Comparison of ZMYND-8 overall methylation levels between NSCLC and normal samples using TCGASTAD methylation cohort. ZMYND-8 shows significantly hypomethylated in NSCLC tumors; ****P < 0.0001. B ZMYND-8 methylation pattern of tissue samples using q-MSP. The obtained results showed that these gene is significantly hypomethylated in NSCLC tumors in comparison with normal adjacent tissues; ***P < 0.001
A RAR-B2 methylation pattern of TCGA datasets. Comparison of RAR-B2 overall methylation levels between NSCLC and normal samples using TCGASTAD methylation cohort. RAR-B2 shows significantly hypermethylated in NSCLC tumors; ****P < 0.0001. B RAR-B2 methylation pattern of tissue samples using q-MSP. The obtained results showed that these gene is significantly hypermethylated in NSCLC tumors in comparison with normal adjacent tissues; ***P < 0.001
Hypomethylation of ZMYND-8 in NSCLC specimens
Q-MSP assay was carried out on a core set of samples, including NSCLC and healthy samples, to confirm the methylation grade of ZMYND-8 achieved from the TCGA-STAD database. As presented in Fig. 1, q-MSP findings also displayed that ZMYND-8 was meaningfully (P = 0.001) hypomethylated in malignancyspecimens compared to neighboring healthy tissues, which was by results attained from TCGA-STAD resources.
We examined the relationship between ZMYND-8 methylation grades in NSCLC samples and obtained clinical and pathological data from patients. Our findings indicated a significant association between ZMYND-8 methylation grades and the clinical grade of cancer (P = 0.0024) and lymph node metastasis (P = 0.043). However, there was no correlation between age, gender, tumor location, and ZMYND-8 methylation. The acquired data are exhibited in Table 3.
RARβ2 hypermethylation of NSCLC specimens
Q-MSP test was accomplished on a core set of samples comprising NSCLC and neighboring standard samples to authenticate the methylation grade of RAR-B2 acquired from TCGA-STAD databases. As shown in Fig. 2, q-MSP discoveries similarly exhibited that RAR-B2 was considerably hypermethylated (P = 0.001) in NSCLC tissues compared to neighboring normal tissues, which was by outcomes achieved from TCGA-STAD resources.
We also analyzed the relation of RARβ2 methylation degrees in NSCLC samples with patients’ clinical and pathological data. Our findings indicated a noteworthy correspondence between RARβ2 methylation degrees and the clinical phase of malignancy (P = 0.0021); conversely, no correlation with other factors. The data are offered in Table 3.
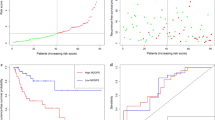
Great prognostic importance of ZMYND-8 and RAR-B2 methylation in NSCLC
To evaluate the possibility and precision of ZMYND-8 and RARβ2 methylations as a diagnosis tool, a receiver operating characteristic curve analysis was carried out. As indicated in Fig. 3, ZMYND-8 and RARβ2 methylation show a great capability as a diagnostic biomarker (AUC = 0.751, P < 0.0001 and AUC = 0.8676, P < 0.0001, in that order) to differentiate NSCLC specimen from normal ones. Though, Kaplan–Meier survival analysis unexpectedly indicated that ZMYND-8 hypomethylation is significantly associated with the higher survival ratio of NSCLC patients (Fig. 4), which introduces provocative stuff for further practical studies.
Discussion
Deactivating tumor suppressor genes or activating the oncogenes is one of the most dependable approaches to studying malignancy transformation because of the epigenetic alterations, such as abnormal cytosine methylation in the CpG dinucleotides. A line of research has stated DNA methylation changes in various genes in lung malignancies, containing the ZMYND-8 and RARβ2 genes, representing a high degree of methylation [20,21,22].
With regarding time as a very critical determinant parameter in the process of diagnosis and treatment of all types of cancers and particularly for lung carcinomas, as mentioned above, in the present study, RARβ2 and ZMYND-8 methylation grade was screened and analyzed to figure out either prognostic or diagnostic tools for NSCLC.
At first, ZMYND-8 methylation as a possible and practicable biomarker for NSCLC was studied by using the TCGA-STAD databases. Based on the microarray methylation screening data, ZMYND-8 was hypomethylated in NSCLC tumors in comparison with healthy tissues, which was validated through the q-MSP technique on a set of core samples, showing the positive association between ZMYND-8 hypomethylation and clinical phase of tumor and lymph node metastasis. Consequently, the ROC curve analysis showed that ZMYND-8 methylation could be used as a diagnostic marker for distinguishing NSCLC cases from healthy ones (AUC = 0.751). Even though, as reported by Kaplan–Meier survival analysis, ZMYND-8 hypomethylation was linked with longevity in NSCLC patients, it rests as debatable stuff for further practice on ZMYND-8 roles in NSCLC progression.
Previous studies indicated that ZMYND-8 mutations or abnormal expression had been known in many human tumors, including ovarian, acute erythroid leukemia, breast, and prostate [10]. There is several evidence for ZMYND-8 function as a tumor-suppressive and oncogenic of several types of malignancy.
Abnormal expression and mutations of ZMYND-8 are related to tumor progression and growth in breast, prostate, colorectal, and cervical cancers. ZMYND-8 have a pro-oncogenic function in prostate and breast malignancy, and it stimulates angiogenesis in prostate and breast tumor. In contrast, ZMYND-8 low expression was reported in breast and prostate tumors. ZMYND-8 has a tumor suppressor function in prostate and breast malignancy, and it prevents tumor development by stimulating differentiation, suppression invasiveness, cell-cycle progression, growth, and metastasis [11]. In another study, Adhikary et al. found that ZMYND-8 suppressing in HeLa cells led to the overexpression of 331 genes and low expression of 438 genes [11].
In a high-grade serious ovarian tumor, the place of the ZMYND-8 gene is within a region with recurrent alterations of somatic copy number [23]. Also, Basu et al. [24] revealed that in HeLa and MCF7 breast cancer cells, ZMYND-8 expression increased by activation of H3K27me3 to H3K27ac via ATRA. Chen et al. [25] revealed that the epigenetic reader zinc finger MYND-type containing 8 (ZMYND-8) is activated by HIF-1 and HIF-2 in breast malignancy cells and also highly expressed in human breast malignancy and is involved with poor survival of patients with breast tumor. In another study, Chen et al. indicated that ZMYND-8 up-regulation was closely involved with poor survival in 174 colorectal malignancy patients [26]. Kuroyanagi et al. [27] suggested that ZMYND-8 may promote angiogenesis in malignancy, especially in hypoxic situations. These findings show that ZMYND-8 may be related with growth and development of cancer.
On the other hand, some evidence shows that ZMYND-8 acts as a tumor suppressor. Basu et al. indicated that silencing of ZMYND-8 in MCF7 and HeLa breast tumor cells increases the proliferation of tumor cells about twofolds. In contrast, high expression of ZMYND-8 decreases the growth of tumor cells about 2.5–3-folds. They also indicated that suppression of the ZMYND-8 expression led to the up-regulation of Ki67 and Proliferating Cell Nuclear Antigen (PCNA) by about 14- and fourfolds, respectively, in HeLa cells; about eight- and threefolds and in MCF7 breast tumor cells [28]. Also, they indicated that suppression of the ZMYND-8 gene in HeLa and MCF7 breast cancer cells led to a 1.6–twofold increase in the invasiveness and increased ZMYND-8 expression level and reduce 1.3–1.5-fold in the invasiveness of the HeLa and MCF7 breast tumor cells [28]. Also, Shen et al. found that suppression of ZMYND-8 expression can increase tumor development in a mammary fat pad xenograft model of ZR-75-30 breast tumor cells [9]
According to a recent study, the ZMYND-8 protein is involved with metastasis corresponding regulatory system, which functions as a transcription suppressor factor in prostate cancer, and ZMYND-8 knockdown increased the cellular invasiveness in vitro and in vivo [29]. Similarly, higher expression of ZMYND-8 in an aggressive breast cancer cell line led to lower tumor progression in mice and humans [28]. Also, several other studies reported tumor-suppressing tumorigenesis inhibition activity of ZMYND-8 in cervical, prostate, breast cancers, etc. [9, 30]. Even though, all of these results show that ZMYND-8 is essential in malignancy control, they are contradictory, and the essential role of ZMYND-8 in tumors is still unclear.
RARβ2 methylation is another potential biomarker for NSCLC that was browsed in the TCGA-STAD data source. Based on the three microarray methylation screening data, RARβ2 indicates hypermethylation in NSCLC tumors, which was validated through the q-MSP technique on a set of core samples, showing the positive association between RARβ2 hypermethylation and clinical phase of tumor and lymph node metastasis. Consequently, the ROC curve analysis further approved the high capability and fine-tuning of RARβ2 methylation as a diagnostic biomarker for distinguishing NSCLC cases from healthy ones (AUC = 0.867).
RARβ is a nuclear retinoic acid receptor protein; when retinoid binds to RARβ, it regulates different cellular processes, including cell growth, differentiation, and apoptosis [31]. Because the RARβ gene is silenced in most NSCLC, therefore, results in a higher risk of lung cancers [32]. Lack of functionality in RARβ plays an excellent role in tumorigenicity of various cancers together with NSCLC [33]. High expression of the RARβ could promote antitumor activities in A549 and H460 cell lines treated with curcumin [34]. However, the recent study indicated that this gene in lung cancer could have either tumor-suppressing or tumor-promoting activities [35]. RARβ acts in a cell-specific manner, which means that in A549 parental cells, it works as a tumor suppressor gene, whereas in A549, cancer stem cells (CSCs) do a completely contradictory function as a tumor-promoting [36].
RARβ2 gene encodes the vitamin A (retinoic acid) protein as a severe factor during various cell processes, including embryogenesis, homeostasis, cell growth, and differentiation. It has been revealed that the RARβ2 gene is methylated in around 60% of NSCLC cells, which is about 9% in healthy lung samples [37, 38]. Ponomaryova et al. [39] by engaging a more significant number of patients, show an increased degree of RARβ2 methylation in lung cancer patient blood samples. Also, there is correlation between RARβ2 methylation degree and clinical stage of disease compared with healthy control samples. However, based on previous reports, an individual gene methylation screen in cirDNA from a blood sample could not accurately diagnose lung cancer [38, 40]. Combining these variants through a machine learning model could lead to discrimination of NSCLC cases from healthy persons.
Fujiwara et al. [41] who evaluate the methylation grade by routine methyl-specific PCR stated a relationship between RARβ2 gene methylation grades in blood sample cirDNA and lung cancer clinical stage. Also, Ponomaryova et al. [42] found that RARβ2 and Ras association domain family member 1 (RASSF1) methylation grades increased considerably in circulatory cirDNA of stage I–II patients in comparison to healthy cases and did not heighten in stage III patients (P > 0.05).
Toyooka et al. [43, 44] indicated that methylation rate of the RARβ2 gene promoter in NSCLC and SCLC was about 35% and 55%, respectively. Abnormal RARβ2 methylation was discovered in up to 14% of non-tumoral lung tissues of lung cancer patients and phlegm of the control group [44, 45].
Also, Chan et al. [46] found that there was a similarly high degree of RARβ2 methylation in malignant tissue and bronchoalveolar lavage fluid of Chinese patients and control group; this study attributed this finding to racial variances in abnormal methylation. However, Toyooka et al. studied comparative methylation degrees of several genes from four territories (USA, Australia, Japan, and Taiwan) and stated no geographical determinants regarding RARβ2 hypermethylation. Therefore, it seems rational to accept procedural differences to account for the observed disparity in RARβ2 methylation status. Earlier studies on RARβ2 methylation in pulmonary specimens applied common MSP. A more robust technology and procedure like QMSP might distinguish initial epigenetic alterations of cells with an everyday look. Another explanation for varying RARβ2 methylation frequencies relates to the CpG sites examined [44]. However, Topaloglu et al. [47] applied a QMSP test similar to this research; they did not distinguish atypical RARβ2 methylation in bronchoalveolar lavages of patients with NSCLC. In other efforts of the same group, atypical promoter methylation of RARβ has been found in bronchoalveolar lavages taken from patients with lung cancer. They stated a sensitivity of 69% and specificity of 87% for the recognition of lung cancer by applying this combination of genes [48].
In another study, Belinsky et al. [49] figured out that higher grades methylation in the promoter region of the variety of genes in the blood and phlegm samples is linked to lung cancer and even before clinical diagnosis of lung carcinoma. In final, ZMYND-8 and RARβ2 RAR-B2 methylation shows a great capability to early stage detection and diagnostic biomarker to differentiate NSCLC specimen from normal ones.
Conclusion
To sum up, experimentally and bioinformatically, the results from the present study showed that aberrant methylation of ZMYND-8 and RARβ2 genes may be an early event through the NSCLC progression and possesses excellent value as the diagnostic biomarker. However, there is a need to further validate these findings in a larger size of samples and clarify the mechanisms underlying ZMYND-8 and RARβ2 dysregulation through tumorigenesis.
Availability of data and materials
All data and material of this manuscript can be made available by the corresponding author.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- SCLC:
-
Small cell lung cancer
- ZMYND-8:
-
Zinc finger MYND-type containing 8
- RARβ:
-
Retinoic acid receptor beta
- RARs:
-
Retinoic acid receptors
- ROC:
-
Receiver operating characteristic
- PCR:
-
Polymerase chain reaction
References
Zarredar H, Pashapour S, Farajnia S, Ansarin K, Baradaran B, Ahmadzadeh V, Safari F (2019) Targeting the KRAS, p38α, and NF-κB in lung adenocarcinoma cancer cells: the effect of combining RNA interferences with a chemical inhibitor. J Cell Biochem 120(6):10670–10677
Zarredar H, Farajnia S, Ansarin K, Baradaran B, Aria M, Asadi M (2019) Synergistic effect of novel EGFR inhibitor AZD8931 and p38α siRNA in lung adenocarcinoma cancer cells. Anti-Cancer Agents Med Chem Former Curr Med Chem-Anti-Cancer Agents 19(5):638–644
Mastoraki S, Lianidou E (2017) DNA and histone methylation in lung cancer. In: Kaneda A, Tsukada YI (eds) DNA and histone methylation as cancer targets. Springer, pp 403–436
Shanehbandi D, Asadi M, Seyedrezazadeh E, Zafari V, Shekari N, Akbari M, Rahbarnia L, Zarredar H microRNA-based biomarkers in lung cancer: recent advances and potential applications. Current Molecular Medicine
Langevin SM, Kratzke RA, Kelsey KT (2015) Epigenetics of lung cancer. Transl Res 165(1):74–90
Di Gioia D, Blankenburg I, Nagel D, Heinemann V, Stieber P (2016) Tumor markers in the early detection of tumor recurrence in breast cancer patients: CA 125, CYFRA 21–1, HER2 shed antigen, LDH and CRP in combination with CEA and CA 15–3. Clin Chim Acta 461:1–7
Tsay J-CJ, Greenberg AK, Rom WN, Massion PP: Preclinical Biomarkers for the Early Detection of Lung Cancer. In: IASLC Thoracic Oncology. edn.: Elsevier; 2018: 59–68. e54
Gong F, Chiu L-Y, Cox B, Aymard F, Clouaire T, Leung JW, Cammarata M, Perez M, Agarwal P, Brodbelt JS (2015) Screen identifies bromodomain protein ZMYND8 in chromatin recognition of transcription-associated DNA damage that promotes homologous recombination. Genes Dev 29(2):197–211
Shen H, Xu W, Guo R, Rong B, Gu L, Wang Z, He C, Zheng L, Hu X, Hu Z (2016) Suppression of enhancer overactivation by a RACK7-histone demethylase complex. Cell 165(2):331–342
Panagopoulos I, Micci F, Thorsen J, Haugom L, Buechner J, Kerndrup G, Tierens A, Zeller B, Heim S (2013) Fusion of ZMYND8 and RELA genes in acute erythroid leukemia. PLoS ONE 8(5):e63663
Chen Y, Tsai Y-H, Tseng S-H (2021) Regulation of ZMYND8 to treat cancer. Molecules 26(4):1083
Gong F, Miller KM (2018) Double duty: ZMYND8 in the DNA damage response and cancer. Cell Cycle 17(4):414–420
Kim Y, Jin D, Lee BB, Cho EY, Han J, Shim YM, Kim D-H (2015) RARβ2 hypermethylation is associated with poor recurrence-free survival in never-smokers with adenocarcinoma of the lung. Clin Epigenet 7(1):1–10
Diaz LA Jr, Bardelli A (2014) Liquid biopsies: genotyping circulating tumor DNA. J Clin Oncol 32(6):579
Schwarzenbach H, Hoon DS, Pantel K (2011) Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer 11(6):426–437
Choi JJ, Reich CF III, Pisetsky DS (2005) The role of macrophages in the in vitro generation of extracellular DNA from apoptotic and necrotic cells. Immunology 115(1):55–62
Tomczak K, Czerwińska P, Wiznerowicz M (2015) The cancer genome atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol 19(1A):A68
Tierling S, Schmitt B, Walter J (2018) Comprehensive evaluation of commercial bisulfite-based DNA methylation kits and development of an alternative protocol with improved conversion performance. Genet Epigenet. https://doi.org/10.1177/1179237X18766097
Bidar N, Rezaei T, Amini M, Jebelli A, Mokhtarzadeh A, Baradaran B (2021) ZNF677 downregulation by promoter hypermethylation as a driver event through gastric tumorigenesis. Exp Mol Pathol 121:104663
Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, Winget M, Yasui Y (2001) Phases of biomarker development for early detection of cancer. J Natl Cancer Inst 93(14):1054–1061
Nagrath S, Sequist LV, Maheswaran S, Bell DW, Irimia D, Ulkus L, Smith MR, Kwak EL, Digumarthy S, Muzikansky A (2007) Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450(7173):1235–1239
Wu C, Hao H, Li L, Zhou X, Guo Z, Zhang L, Zhang X, Zhong W, Guo H, Bremner RM (2009) Preliminary investigation of the clinical significance of detecting circulating tumor cells enriched from lung cancer patients. J Thorac Oncol 4(1):30–36
Network CGAR (2011) Integrated genomic analyses of ovarian carcinoma. Nature 474(7353):609
Basu M, Khan MW, Chakrabarti P (1860) Das C (2017) Chromatin reader ZMYND8 is a key target of all trans retinoic acid-mediated inhibition of cancer cell proliferation. Biochim Biophys Acta Gene Regul Mech 4:450–459
Chen Y, Zhang B, Bao L, Jin L, Yang M, Peng Y, Kumar A, Wang JE, Wang C, Zou X (2018) ZMYND8 acetylation mediates HIF-dependent breast cancer progression and metastasis. J Clin Investig 128(5):1937–1955
Chen J, He Q, Wu P, Fu J, Xiao Y, Chen K, Xie D, Zhang X (2020) ZMYND8 expression combined with pN and pM classification as a novel prognostic prediction model for colorectal cancer: based on TCGA and GEO database analysis. Cancer Biomark 28(2):201–211
Kuroyanagi J, Shimada Y, Zhang B, Ariyoshi M, Umemoto N, Nishimura Y, Tanaka T (2014) Zinc finger MYND-type containing 8 promotes tumour angiogenesis via induction of vascular endothelial growth factor-A expression. FEBS Lett 588(18):3409–3416
Basu M, Sengupta I, Khan MW, Srivastava DK, Chakrabarti P, Roy S, Das C (2017) Dual histone reader ZMYND8 inhibits cancer cell invasion by positively regulating epithelial genes. Biochem J 474(11):1919–1934
Li N, Li Y, Lv J, Zheng X, Wen H, Shen H, Zhu G, Chen T-Y, Dhar SS, Kan P-Y (2016) ZMYND8 reads the dual histone mark H3K4me1-H3K14ac to antagonize the expression of metastasis-linked genes. Mol Cell 63(3):470–484
Vickers NJ (2017) Animal communication: When i’m calling you, will you answer too? Curr Biol 27(14):R713–R715
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ (2006) Cancer statistics, 2006. CA Cancer J Clin 56(2):106–130
Eramo A, Lotti F, Sette G, Pilozzi E, Biffoni M, Di Virgilio A, Conticello C, Ruco L, Peschle C, De Maria R (2008) Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ 15(3):504–514
Zhang X-k, Liu Y, Lee M-O, Pfahl M (1994) A specific defect in the retinoic acid response associated with human lung cancer cell lines. Can Res 54(21):5663–5669
Jiang A, Wang X, Shan X, Li Y, Wang P, Jiang P, Feng Q (2015) Curcumin reactivates silenced tumor suppressor gene RARβ by reducing DNA methylation. Phytother Res 29(8):1237–1245
Collins LG, Haines C, Perkel R, Enck RE (2007) Lung cancer: diagnosis and management. Am Fam Physician 75(1):56–63
Halim NHA, Zakaria N, Das KT, Lin J, Lim MN, Fakiruddin KS, Yahaya BH (2021) The effects of lentivirus-mediated gene silencing of RARβ on the stemness capability of non-small cell lung cancer. J Cancer 12(12):3468
Hsu HS, Chen TP, Hung CH, Wen CK, Lin RK, Lee HC, Wang YC (2007) Characterization of a multiple epigenetic marker panel for lung cancer detection and risk assessment in plasma. Cancer 110(9):2019–2026
Zhang Y, Wang R, Song H, Huang G, Yi J, Zheng Y, Wang J, Chen L (2011) Methylation of multiple genes as a candidate biomarker in non-small cell lung cancer. Cancer Lett 303(1):21–28
Ponomaryova AA, Rykova EY, Cherdyntseva NV, Skvortsova TE, Dobrodeev AY, Zavyalov AA, Tuzikov SA, Vlassov VV, Laktionov PP (2011) RARβ2 gene methylation level in the circulating DNA from blood of patients with lung cancer. Eur J Cancer Prev 20(6):453–455
Fleischhacker M, Schmidt B (2007) Circulating nucleic acids (CNAs) and cancer—a survey. Biochim Biophys Acta Rev Cancer 1775(1):181–232
Fujiwara K, Fujimoto N, Tabata M, Nishii K, Matsuo K, Hotta K, Kozuki T, Aoe M, Kiura K, Ueoka H (2005) Identification of epigenetic aberrant promoter methylation in serum DNA is useful for early detection of lung cancer. Clin Cancer Res 11(3):1219–1225
Ponomaryova AA, Rykova EY, Cherdyntseva NV, Skvortsova TE, Dobrodeev AY, Zavyalov AA, Bryzgalov LO, Tuzikov SA, Vlassov VV, Laktionov PP (2013) Potentialities of aberrantly methylated circulating DNA for diagnostics and post-treatment follow-up of lung cancer patients. Lung Cancer 81(3):397–403
Toyooka S, Toyooka KO, Maruyama R, Virmani AK, Girard L, Miyajima K, Harada K, Ariyoshi Y, Takahashi T, Sugio K (2001) DNA methylation profiles of lung tumors1. Mol Cancer Ther 1(1):61–67
Toyooka S, Maruyama R, Toyooka KO, McLerran D, Feng Z, Fukuyama Y, Virmani AK, Zochbauer-Muller S, Tsukuda K, Sugio K (2003) Smoke exposure, histologic type and geography-related differences in the methylation profiles of non-small cell lung cancer. Int J Cancer 103(2):153–160
Gilliland FD, Harms HJ, Crowell RE, Li Y-F, Willink R, Belinsky SA (2002) Glutathione S-transferase P1 and NADPH quinone oxidoreductase polymorphisms are associated with aberrant promoter methylation of P16INK4a and O6-methylguanine-DNA methyltransferase in sputum. Can Res 62(8):2248–2252
Chan EC, Lam SY, Tsang KW, Lam B, Ho JC, Fu KH, Lam WK, Kwong YL (2002) Aberrant promoter methylation in Chinese patients with non-small cell lung cancer: patterns in primary tumors and potential diagnostic application in bronchoalevolar lavage. Clin Cancer Res 8(12):3741–3746
Topaloglu O, Hoque MO, Tokumaru Y, Lee J, Ratovitski E, Sidransky D, Moon C-s (2004) Detection of promoter hypermethylation of multiple genes in the tumor and bronchoalveolar lavage of patients with lung cancer. Clin Cancer Res 10(7):2284–2288
Grote HJ, Schmiemann V, Geddert H, Rohr UP, Kappes R, Gabbert HE, Böcking A (2005) Aberrant promoter methylation of p16INK4a, RARB2 and SEMA3B in bronchial aspirates from patients with suspected lung cancer. Int J Cancer 116(5):720–725
Belinsky SA, Liechty KC, Gentry FD, Wolf HJ, Rogers J, Vu K, Haney J, Kennedy TC, Hirsch FR, Miller Y (2006) Promoter hypermethylation of multiple genes in sputum precedes lung cancer incidence in a high-risk cohort. Can Res 66(6):3338–3344
Acknowledgements
We would like to appreciate the cooperation of the Clinical Research Development Unit of Imam Reza General Hospital, Tabriz, Iran in conducting this research.
Funding
This study was supported by a grant from the research deputy of the Department of Tuberculosis and Lung Diseases Research Center, University Tabriz University of Medical Sciences, Tabriz, Iran.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. Conceptualization was done by MP, MA, and MR; methodology was done by MP, AC and MR; data analysis and investigation were done by AS, HB, and SB; writing original draft preparation was done by MP and HZ; writing, review and editing were done by HZ, SHH, and MR; funding acquisition was done by MR; and supervision was done by SHH and MR.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical confirmation of this study was issued from Tabriz University of Medical Sciences Author Statement.
Consent for publication
Not applicable.
Competing interests
The author declare they have not any of conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pourasghariazar, M., Zarredar, H., Asadi, M. et al. Comparative evaluation of ZMYND-8 and RARβ2 genes promoters’ methylation changes in tumor and tumor margin tissues of patients with lung cancer. Egypt J Med Hum Genet 24, 20 (2023). https://doi.org/10.1186/s43042-023-00399-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00399-w