Abstract
Background
Vascular endothelial growth factor (VEGF) is a signal protein, induces cell proliferation, and enhances the permeability of the endothelial cells. VEGF-A gene is highly polymorphic, with different near-gene variants at varied frequencies linked with altered VEGF protein expression, type 2 diabetes mellitus (T2DM) susceptibility, and associated microvascular complications. The present study aimed to investigate the role of two genetic variants of VEGF-A, − 583C > T (rs3025020) and + 936 C/T (rs3025039), for predicting mixed microvascular complications in T2DM. This case–control study was performed on 26 T2DM patients with mixed microvascular complications and 26 apparently healthy individuals, as a control group. Clinical, neurological, funds examinations, and biochemical laboratory investigations were conducted on all groups. The serum level of VEGF-A was measured using ELISA. Genotyping of VEGF-A was performed by real-time PCR allelic discrimination system.
Results
Serum level of VEGF-A was significantly increased in T2DM with mixed complications. T allele of VEGF-A rs3025020 showed higher frequency among T2DM patients with mixed complications than in control group [OR 2.67; 95% CI 1.03–6.91; p = 0.04], while CT genotype and T allele of VEGF-A rs3025039 had a high frequency in mixed complication group [OR 4.08; 95% CI 1.32–17.44; p = 0.01 and OR 4.02; 95% CI 1.52–10.63; p = 0.004, respectively].
Conclusion
VEGF-A increased the level contributed in the pathogenesis of mixed diabetic microvascular complications. T allele of VEGF-A rs3025020, CT genotype, and T allele of VEGF-A rs3025039 had the highest frequency in mixed diabetic microvascular complications, so they were considered risk genes for mixed diabetic microvascular complications.
Similar content being viewed by others
Background
Microvascular complications are highly prevalent in type 2 diabetes mellitus (T2DM) patients: 38% of the patients present with any stage of chronic kidney disease (CKD) [1], almost 30% have retinopathy (DR) [2], and > 30% have peripheral neuropathy (PN) [3].
Microvascular complications are common in tissues where glucose uptake is independent of insulin activity as these tissues are exposed to glucose levels that directly correlate with blood glucose levels. These metabolic insults result in alterations in blood flow, endothelial permeability, extravascular protein precipitation, and coagulation, leading to organ dysfunction and microvascular complications [4].
Developing microvascular complications is explained by a variety of theories, including generation of reactive oxygen species and oxidative stress, stimulation of polyol pathway, production of advanced glycation end products, initiation of flux through the hexosamine pathway, modified expression and action of growth factors such as vascular endothelial growth factor (VEGF), and triggering of protein kinase C (PKC) [5].
VEGF is a mitogen substance in endothelial cells. It is also known as vasopermeable and vasculotropin factor which is a homodimer glycoprotein, about 45 kDa [6]. Derivatives of VEGF including VEGF-A, VEGF-B, VEGF-C, and VEGF-D and two similar compounds of VEGF coded by Parapoxvirus (VEGF-E and VEGF-F), and placenta growth factor (PIGF) were involved in the tissue of myocardium, lungs, spleen, and liver. Each VEGF derivative is functionally and structurally a different substance that is coded by a different gene [7].
VEGF-A gene encodes VEGF and is situated on chromosome 6 (6p21.3) with seven introns and eight exons and molecular length of 14 kb [8]. Numerous genetic variations in the VEGF-A gene have been identified, some of which influence VEGF secretion and modulate VEGF expression [9]. VEGF-A gene polymorphism is associated with several diseases including autoimmune disease [10], metabolic syndrome [11], microvascular complications of diabetes [12], recurrent spontaneous miscarriage [13], polycystic ovary [14], necrotizing enterocolitis [15], and cancers [16].
In a hypoxic state, VEGF-A expression rises. It is important in the pathogenesis of diabetes and associated consequences, especially those related to poor vascularization and hypoxia. In this line, it was discovered that inhibiting VEGF-A signaling caused hypertension, proteinuria, and kidney damage in diabetic patients [12].
VEGF-A SNPs comprised numerous variants such as rs699947, rs833061, rs1570360, rs699947, rs2010963, rs3025020, and rs3025039. Many studies reported that VEGF-A rs3025020 and rs3025039 had a tendency to be a risk factor for developing microvascular complications in diabetic patients.
Therefore, the current study aimed to investigate the role of VEGF-A, -583C > T (rs3025020), and + 936 C/T (rs3025039) gene polymorphisms in predicting mixed microvascular complications in T2DM patients.
Methods
This hospital-based case–control study was conducted in Clinical Pathology Department, Faculty of Medicine Menoufia University from November 2020 to May 2021. Twenty-six T2DM patients with mixed microvascular complications (more than one complication) were selected from the Internal Medicine Outpatient Clinics and Inpatient Departments. Moreover, 26 apparently healthy individuals, age- and gender-matched with patients’ group, were included as a control group. Informed written consent was attained from all subjects, and the study was approved by the Research Ethics Committee of Medical Research, Faculty of Medicine, Menoufia University.
All patients enrolled in the study had T2DM (diagnosed based on clinical and laboratory features, as per the 2020 WHO criteria for diabetes classification and diagnosis). Those with other types of diabetes and autoimmune diseases were excluded. None of the patients ever had ketoacidosis. All groups were subjected to the following examinations and testing:
Clinical Examination: Neurological and fundus examination were included.
Laboratory investigations:
Blood Sample: 5 ml of venous blood was aseptically collected and divided as follows: 2 ml was collected into an ethylenediaminetetraacetic acid (EDTA) tube and then divided into two aliquots for HbA1C assay and VEGF-A genotyping. The remaining 3 ml was collected in a plain tube for biochemical laboratory investigations.
Urine Specimen: Random urine samples were collected to estimate urine creatinine and albumin and calculate albumin/creatinine ratio (ACR).
Laboratory Tests: Fasting blood glucose (FBG), lipid profile (triglycerides (TG)), total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), blood urea nitrogen (BUN), creatinine, and uric acid were measured using AU680 analyzers (Beckman Coulter, Indianapolis, USA). Glycated hemoglobin (HbA1C%) was assayed by Roche Diagnostics (Mannheim, Germany). eGFR was calculated according to the Modification of Diet in Renal Disease (MDRD) formula (GFR (mL/min/1.73 m2) = 186 × [serum creatinine] − 1.154 × [age] − 0.203 × [1.212 if black] × [0.742 if female] [17]. For ACR, creatinine was assayed by AU680. Albumin level was determined by an immunoturbidimetric method using the HEALES albumin test kit (HEALES, Shenzhen Huisong Technology Development, China); then, urinary ACR (milligram/gram (mg/g)) was calculated [18].
Serum VEGF Assay: Detection of serum VEGF-A levels was performed through the use of a human vascular endothelial growth factor A (VEGF-A) ELISA Kit (Sunlong Biotech Co., Ltd., China) according to the manufacturer's instructions.
VEGF-A genotyping using real-time PCR technique
-
1.
Genomic DNA Extraction [19]: Total genomic DNA was isolated from peripheral blood lymphocytes of all patients using Thermo Scientific Gene JET Whole Blood Genomic DNA Purification Mini Kit (Thermo Fisher Scientific, USA). Then, DNA concentration and purity were measured spectrophotometrically through the use of the Nanodrop (Implen NanoPhotometerTM N60 UV/VIS spectrophotometer, Rödermark, Germany). The extracted DNA was stored at − 80 °C until performing the genotyping.
-
2.
TaqMan SNP Assay [20]: Allelic discrimination method was utilized for VEGF-A genotyping. TaqMan assays were ordered from TaqMan probes supplied by Thermo Fisher Scientific, USA: rs3025020 (C_1647366_10) fluorescent-labeled probes [VIC/VAM] GCCTCTGGAGGGGAGCCCCCTATTC[C/T]GGCCCAACCCATGGCACCCACAGAG and rs3025039 (C_16198794_10) fluorescent-labeled probes [VIC/VAM] GCATTCCCGGGCGGGTGACCCAGCA[C/T] GGTCCCTCTTGGAATTGGATTCGCC. The reaction was performed using an ABI 7500 real-time PCR system (Applied Biosystems, Foster City, California, USA). 20 μl reaction volume was prepared by adding 1.25 μl of the probe, 10 μl of Master Mix, and 0.75 μl of DNAase-free water to 8 μl of DNA template from each sample and 8 μl of nuclease-free water for the negative control. PCR conditions were as follows: Initial denaturation was done at 95 °C for 15 min, followed by 50 cycles of denaturation at 94 °C for 1 min, primer annealing at 60 °C for 1 min, then primer extension at 74 °C for 2 min, and the final extension step at 72 °C for 1 min. The allele distribution and amplification plots are demonstrated in Figs. 1 and 2.
Statistical analysis
Statistical Package for Social Sciences, version 19 (SPSS Inc., Chicago, USA), was utilized for analyzing data. Qualitative data (frequency and percentage) were expressed using chi-square test, while quantitative data were expressed using mean, standard deviation (SD), and median. Mann–Whitney test was used for two nonparametric variables between two groups. Difference between more than two groups that are normally distributed and not normally distributed was demonstrated using analysis of variance (ANOVA) and Kruskal–Wallis tests, respectively, followed by post hoc test. Spearman correlation evaluates the strength and direction of association between number of minor alleles of both genetic variants and measured parameters. Odds ratio measures the risk of carrying minor allele as a predictor for complications. Receiver operating characteristic (ROC) curve is created by plotting sensitivity (TP) on Y axis versus 1—specificity (FP) on X axis at various cutoff values. The diagnostic performance of a test is measured by the area under the ROC curve (AUC). A p value < 0.05 was considered significant.
Results
The demographic clinical data of the studied groups (Table 1) demonstrated that the groups were age- and gender-matched. In T2DM patients, the duration of disease ranged from 3 to 20 years. 88.5% of patients had neurological symptoms, while 57.6% had fundus affection.
Laboratory investigations of the studied groups (Table 2) indicated that FBG, HbA1c%, total cholesterol, LDL-c, albumin/creatinine ratio, creatinine, BUN, and uric acid were statistically significantly higher, while eGFR and HDL-c were statistically significantly lower in T2DM patients with mixed microvascular complications than in control group (p < 0.001). Furthermore, VEGF-A was significantly increased in mixed complications group in comparison with control group (p 0.003). Moreover, there was no statistically significant difference between the two groups regarding TG (p 0.08).
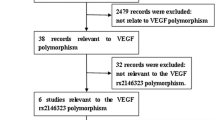
Regarding VEGF-A rs3025020 and rs3025039 polymorphism analysis (Table 3), there was no significant difference in rs3025020 genotypes distribution among the studied groups. T allele had a significantly high frequency in T2DM patients with mixed complications [OR 2.67; 95% CI 1.03–6.91; p = 0.04]. According to VEGF-A rs3025039 distributions, C/T genotype and T allele had a significantly high frequency in T2DM patients with mixed complications [OR 4.08; 95% CI 1.32–17.44; p = 0.01 and OR 4.02; 95% CI 1.52–10.63; p = 0.004, respectively] (Fig. 3).
Regarding relationship between rs3025020 and rs3025039 genotypes and different studied parameters in both T2DM patients with mixed diabetic complications (Table 4) and control groups (Table 5), there was a significant difference between both rs3025020 and rs3025039 genotypes in mixed complications group and age of patients (p = 0.01 in both genes). Moreover, there was a significant difference between rs3025039 genotypes and T2DM duration (p = 0.04). No significant statistical differences between different genotypes and serum VEGF-A level in different groups were detected.
ROC curve analysis of serum level of VEGF-A (Fig. 4) for differentiation between mixed complication DM cases and controls revealed that AUC was 0.55 and P value was 0.53, at cutoff point 117.5, sensitivity 64.5, specificity 50%, and total accuracy 57.7%.
Discussion
T2DM is a chronic persistent hyperglycemia that results in an increase in glycosylation products. These products cause vascular tissue alterations and promote atherosclerosis by generating inflammation and damage to arterial walls. Atherosclerosis damages smaller blood arteries, leading to microvascular problems such as diabetic peripheral neuropathy, retinopathy, and nephropathy [21].
VEGF is a secreted mitogen that is extremely specific for vascular endothelial cells and has been linked to cell proliferation and migration. VEGF has long been thought to be a key determinant and regulator of angiogenesis, vasculogenesis, and vascular permeability as a multifunctional cytokine. A number of studies have confirmed that VEGF-A plays a key role in the pathogenesis of diabetic microvascular complications [22]. In the current study, the role of VEGF-A and two genetic variants, -583C > T (rs3025020) and + 936 C/T (rs3025039), was investigated for prediction of mixed microvascular complications in type 2 diabetic patients.
This study reported a significant difference in biochemical investigations between diabetic and control groups. T2DM patients with mixed microvascular complications had poor glycemic control as reflected in their high FBG and HbA1c%. Furthermore, diabetic patients had poor lipid control, with high level of kidney functions, ACR, and significant decrease in eGFR and HDL-c. These results were in agreement with those of Omar et al. [23] who reported significant difference in biochemical results between diabetic and control groups. T2DM patients had a high FBG and HbA1c%, demonstrating that HbA1c is a good indicator of glycemic status. Impaired glycemic control in DM plays a crucial role in rapid progression of microvascular complications caused by variable hemodynamic, metabolic, or endothelial dysfunctions.
Furthermore, Sellami et al. [24] indicated that T2DM patients had higher FBG, HbA1c, total cholesterol, and LDL-C than control group.
Serum level of VEGF-A was significantly increased in T2DM patients with mixed microvascular complications in comparison with the control group. This result was confirmed by Mahdy et al. [25] who found a considerable rise in serum VEGF in diabetic patients with various micro- and macrovascular complications compared to the uncomplicated diabetic patients and control subjects. Biswas et al. [26] discovered that elevated VEGF-A level was a risk factor for the presence and severity of vascular complications in diabetic patients, and VEGF-A concentrations tend to increase with the progression of mixed diabetic microvascular complications. In addition, Zhang et al. [27] reported that hyperglycemia, inflammation, and VEGF have all been associated with microvascular disorders in T2DM patients, and higher circulating levels of VEGF have played a role in the pathogenesis of T2DM microangiopathy. Sharma et al. [28] detected increased serum VEGF-A level in diabetic groups compared to control subjects, and the level further increased with increasing duration of disease.
There was no significant difference in VEGF-A rs3025020 genotypes distribution among the studied groups. T allele had a significantly high frequency in T2DM patients with mixed complications. Regarding VEGF-A rs3025039 distributions, C/T genotype and T allele had a significantly high frequency in T2DM patients with mixed complications. These results were in agreement with those of Sun et al. [29] who confirmed that VEGF-A rs3025039 was associated with susceptibility to diabetic nephropathy in T2DM patients. A possible explanation is that such polymorphism in the VEGF gene boosted its expression, which was hypothesized to play a critical role in podocyte injury by operating in a unique autocrine signaling manner to produce diabetic podocytopathy and the genesis of albuminuria associated with diabetic nephropathy. Moreover, Arredondo-Garc et al. [30] concluded that the VEGF-A rs3025039 genetic variants were related to diabetic neuropathy in Mexican T2DM patients. Kafeel et al. [31] confirmed significant association of C/T VEGF-A genetic variant at the + 936 position (rs3025039) with an increased diabetic retinopathy risk among the Asian population. Imbaby et al. [32] reported that T2DM patients showed a statistically significant higher frequency of VEGF-936 (rs3025039) C/T genotype compared to controls and lower CC genotype frequency, but this was not statistically significant. Furthermore, the frequency of T allele was higher among patients than controls, but this was not statistically significant. However, Yari et al. [33] studied the relationship between VEGF rs3025039 gene variant and the risk of T2DM and showed no significant association between VEGF rs3025039 variant and T2DM.
Studying the relationship between rs3025020 and rs3025039 genotypes and different studied parameters in both mixed diabetic complications and control groups showed significant difference between rs3025020 and rs3025039 genotypes in mixed complications group and age of patients. Additionally, there was a significant difference between rs3025039 genotypes in mixed complications group and T2DM duration. However, there was no significant difference with other studied parameters in mixed complications and control groups. Handoko et al. [34] indicated that the length of sickness had an effect on the microvascular complications in T2DM patients. This was in accordance with a study conducted by Abu Al-Halaweh et al. [35] who observed substantial link between microvascular problems and diabetes duration. However, Nanayakkara et al. [36] stated that diabetes duration and age at diagnosis were independently linked to a higher incidence of microvascular problems, and vice versa.
In the present study, ROC analysis of VEGF-A yields minimal clinical significance between groups, as it revealed that AUC was 0.55, statistically insignificant with p value 0.53, and the best cutoff point was 117.5 pg/ml. At this cutoff, the sensitivity was 64.5, specificity was 50%, and total diagnostic accuracy was 57.7%. These results were quite different from those stated by Ahuja et al. [37] as their results indicated that ROC for serum VEGF-A levels was significant in distinguishing between cases and controls and had high accuracy in discriminating between subjects with and without retinopathy. The AUC for discrimination was 0.858 and 0.791 for cases and controls, respectively, with over 90% sensitivity and specificity at various cutoff levels. This agreement could be explained by the smaller number of cases in our study and the other factors that could affect VEGF-A serum level.
In a previous study reported by El-Deeb et al. [38], there was a difficulty in selecting diabetic patient with microvascular complication at specific single organ site like diabetic patient with only diabetic nephropathy or only diabetic retinopathy, etc. We did not face this limitation as our cases were diabetic patients with mixed microvascular complications. However, despite the comprehensive analysis of the association between VEGF-A gene polymorphisms and mixed diabetic microvascular complications risk, our analysis still had limitations. First, the mixed diabetic microvascular complications etiology is complex and multifactorial. The relationships between VEGF-A gene polymorphisms and other risk factors were not analyzed in our study, such as environmental factors, diet, and exercise. Second, other VEGF gene polymorphisms were not analyzed in this study.
Conclusion
VEGF-A increased the level contributed in the pathogenesis of mixed diabetic complications. Moreover, CT genotype, T allele of rs3025039, and T allele of rs3025020 had a significantly high frequency in T2DM patients with mixed complications. Therefore, VEGF-A serum level and VEGF-A rs3025039 and rs3025020 genetic variants could predict mixed microvascular diabetic complications.
Further studies including a larger sample size, haplotyping analysis of VEGF-A rs3025039 and rs3025020, and more VEGF-A gene SNPs are necessary to achieve more conclusive results about the association between VEGF-A gene polymorphisms and mixed diabetic microvascular complications susceptibility.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- ACR:
-
Albumin/creatinine ratio
- eGFR:
-
Estimated glomerular filtration rate
- FBG:
-
Fasting blood glucose
- HbA1c:
-
Glycated hemoglobin A1C
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- T2DM:
-
Type 2 diabetes mellitus
- VEGF:
-
Vascular endothelial growth factor
References
Chen Y, Lee K, Ni Z, He JC (2020) Diabetic kidney disease: challenges, advances, and opportunities. Kidney Dis 6:215–225. https://doi.org/10.1159/000506634
Voigt M, Schmidt S, Lehmann T, Kohler B, Kloos C, Voigt UA et al (2018) Prevalence and progression rate of diabetic retinopathy in type 2 diabetes patients in correlation with the duration of diabetes. Exp. Clin. Endocrinol. Diabetes 126:570–576. https://doi.org/10.1055/s-0043-120570
Salvotelli L, Stoico V, Perrone F, Cacciatori V, Negri C, Brangani C (2015) Prevalence of neuropathy in type 2 diabetic patients and its association with other diabetes complications: the Verona Diabetic Foot Screening Program. J. Diabetes Complicat 29:1066–1070. https://doi.org/10.1016/j.jdiacomp.2015.06.014
Sugahara M, Pak WL, Tanaka T, Tang SCW, Nangaku M (2021) Update on diagnosis, pathophysiology, and management of diabetic kidney disease. Nephrology 26:491–500. https://doi.org/10.1111/nep.13860
Khalil H (2017) Diabetes microvascular complications-A clinical update. Diabetes Metab Syndr Clin Res Rev 11:133–139. https://doi.org/10.1016/j.dsx.2016.12.022
Robciuc MR, Kivela R, Williams IM, de Boer JF, Dijk THV, Elamaa H et al (2016) VEGFB/VEGFR1-induced expansion of adipose vasculature counteracts obesity and related metabolic complications. Cell Metab 23:712–24. https://doi.org/10.1016/j.cmet.2016.03.004
Eichmann A, Simons M (2012) VEGF signaling inside vascular endothelial cells and beyond. Curr Opin Cell Biol 24:188–193. https://doi.org/10.1016/j.ceb.2012.02.002
Al-Habboubi HH, Sater MS, Almawi AW, Al-Khateeb GM, Almawi WY (2011) Contribution of VEGF polymorphisms to variation in VEGF serum levels in a healthy population. Eur Cytokine Netw 22:154–158. https://doi.org/10.1684/ecn.2011.0289
Hamid HM, Abdalla SE, Sidig M, Adam I, Hamdan HZ (2020) Association of VEGFA and IL1β gene polymorphisms with preeclampsia in Sudanese women. Mol Genet Genom Med 8:1119–1121. https://doi.org/10.1002/mgg3.1119
Apte RS, Chen DS, Ferrara N (2019) VEGF in signaling and disease: beyond discovery and development. Cell 176:1248–1264. https://doi.org/10.1016/j.cell.2019.01.021
Kim YR, Hong SH (2015) Association between the polymorphisms of the vascular endothelial growth factor gene and metabolic syndrome. Biomed Rep 3:319–326. https://doi.org/10.3892/br.2015.423
Zhang Q, Fang W, Ma L, Wang ZD, Yang YM, Lu YQ (2018) VEGF levels in plasma in relation to metabolic control, inflammation, and microvascular complications in type-2 diabetes: a cohort study. Medicine. 97(15):415. https://doi.org/10.1097/MD.0000000000010415
Almawi WY, Saldanha FL, Mahmood NA, Al-Zaman I, Sater MS, Mustafa FE (2013) Relationship between VEGFA polymorphisms and serum VEGF protein levels and recurrent spontaneous miscarriage. Human Repro 28:2628–2635. https://doi.org/10.1093/humrep/det308
Ben Salem A, Megdich F, Kacem O, Souayeh M, Hachani Ben Ali F, Hizem S et al (2016) Vascular endothelial growth factor (VEGFA) gene variation in polycystic ovary syndrome in a Tunisian women population. BMC Genom 17(9):748. https://doi.org/10.1186/s12864-016-3092-5
Gao X, Ma F, Hao H, Dai Y, Liu W, Xiao X (2019) Association of VEGFA polymorphisms with necrotizing enterocolitis in Chinese Han population. Pediatr Neonatol 60(129):134. https://doi.org/10.1016/j.pedneo.2018.07.002
Goel HL, Mercurio AM (2013) VEGF targets the tumour cell. Nat Rev Cancer 13:871–882. https://doi.org/10.1038/nrc3627
Xie XJ, Yang YM, Jiang JK, Lu YQ (2017) Association between the vascular endothelial growth factor single nucleotide polymorphisms and diabetic retinopathy risk: a meta-analysis. J Diabetes 9:738–753. https://doi.org/10.1111/1753-0407.12480
Arredondo-García VK, Cepeda-Nieto AC, Batallar-Gómez T, Salinas-Santander M, Zugasti-Cruz A, Ramírez-Calvillo L et al (2019) Association of the vascular endothelial growth factor gene polymorphism +936 C/T with diabetic neuropathy in patients with type 2 diabetes mellitus. Arch Med Res. 50:181–186. https://doi.org/10.1016/j.arcmed.2019.07.012
KDIGO 2012. Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013;3(1): 5–14.
Schwab SJ, Christensen RL, Dougherty K, Klahr S (1987) Quantitation of proteinuria with the use of protein-to-creatinine ratios in single urine samples. Arch Intern Med 147(5):943–944
Pavlov AR, Pavlova NV, Kozyavkin SA, Slesarev AI (2004) Recent developments in the optimization of thermostable DNA polymerase for efficient application. Trends Biotechnol 22:253–260. https://doi.org/10.1016/j.tibtech.2004.02.011
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M et al (2009) The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55:611–622. https://doi.org/10.1373/clinchem.2008.112797
Afroz A, Zhang W, Loh AJW, Lee DX, Billah B (2019) Macro- and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr Clin Res Rev 13:2939–2946. https://doi.org/10.1016/j.dsx.2019.07.046
Sun L, Yuan Q, Cao N, Guo W, Yao L et al (2020) VEGF genetic polymorphisms may contribute to the risk of diabetic nephropathy in patients with diabetes mellitus: a meta-analysis. Sci World J. https://doi.org/10.1155/2020/6482307
Omar TA, Zewain SK, Ghonaim MM, Refaat AK, Abou-Elela DH (2021) Role of engulfment and cell motility 1 (ELMO1) gene polymorphism in development of diabetic kidney disease. Egypt J Med Hum Genet 22:49. https://doi.org/10.1186/s43042-021-00167-8
Sellami N, Lamine LB, Turki A, Sarray S, Jailani M, Al-Ansari AK et al (2018) Association of VEGFA variants with altered VEGF secretion and type 2 diabetes: a case-control study. Cytokine 106:29–34. https://doi.org/10.1016/j.cyto.2018.03.003
Mahdy RA, Nada WM, Hadhoud KM, El-Tarhony SA (2010) The role of vascular endothelial growth factor in the progression of diabetic vascular complications. Eye 24:1576–1584. https://doi.org/10.1038/eye.2010.86
Biswas P, Chakraborty AK, Mukherjee A, Pal B, Maji D, De M (2019) Elevated vascular endothelial growth factor level in association with mean platelet volume are emerging risk factors for vascular complications in T2DM patients. Health 11:1542–1553. https://doi.org/10.4236/health.2019.1111116
Sharma S, Satish S, Shetty MS (2021) Vascular endothelial growth factor expression in diabetic nephropathy; a clinicopathological study. J Nephropathol 10(2):e18. https://doi.org/10.34172/jnp.2021.18
Sun X, Zhang H, Liu J, Wang G (2019) Serum vascular endothelial growth factor level is elevated in patients with impaired glucose tolerance and Type 2 diabetes mellitus. J Int Med Res 47:5584–5592. https://doi.org/10.1177/0300060519872033
Kafeel S, Nangrejo KM, Gonzalez-Salinas R (2021) Genetic association of vascular endothelial growth factor (VEGF) gene variants with the risk for diabetic retinopathy: a meta-analysis. Int J Diabetes Dev Ctries 41:180–188. https://doi.org/10.1007/s13410-020-00874-9
Imbaby SA, Badrah M, Abdel Fattah YH (2021) The relation between IL-10 gene (-1082G/A) and VEGF gene 936 C/T polymorphism and diabetic polyneuropathy in a cohort of Egyptian patients with type 2 diabetes. Clin Diabetol 10:2450–7458. https://doi.org/10.5603/DK.a2021.0036
Yari H, Sooltani NJ, Saremi MA (2020) Investigating the relationship between VEGF gene C936T-rs3025039 polymorphism and type-2 diabetes. Pers Med J 5(17):21–24. https://doi.org/10.22034/pmj.2020.43457
Handoko H, Rahardjo SS, Murti B (2018) Predictors of macro and micro-vascular complication in Type 2 diabetes mellitus patients. Indones J Med 3:1–13. https://doi.org/10.26911/theijmed.2018.03.01.01
Abu Al-Halaweh A, Davidovitch N, Almdal TP, Cowan A, Khatib S, Nasser-Eddin L et al (2017) Prevalence of type 2 diabetes mellitus complications among palestinians with T2DM. Diabetes Metab Syndr Clin Res Rev 11:783–787. https://doi.org/10.1016/j.dsx.2017.05.017
Nanayakkara N, Ranasinha S, Gadowski A, Heritier S, Flack JR, Wischer N et al (2017) Age, age at diagnosis and diabetes duration are all associated with vascular complications in type-2 diabetes. J Diabetes Complicat 32:279–290. https://doi.org/10.1016/j.jdiacomp.2017.11.009
Ahuja S, Saxena S, Akduman L, Meyer CH, Kruzliak P, Khanna VK et al (2019) Serum vascular endothelial growth factor is a biomolecular biomarker of severity of diabetic retinopathy. Int J Retin Vitr 5:29. https://doi.org/10.1186/s40942-019-01796
El-Deeb S, El-Saeed GK, Khodeer SA, Dawood AA, Omar TA, Ibrahim RA, ELShemy AM, Montaser BA (2022) Vascular endothelial growth factor with genetic variants rs3025020 and rs3025039 in diabetic micro-vascular complications. Menoufia Med J 35:26–33. https://doi.org/10.4103/mmj.mmj_139_21
Acknowledgements
None.
Funding
This study was self-funded. No financial support.
Author information
Authors and Affiliations
Contributions
TO designed the protocol of work, wrote the abstract, and discussed the manuscript. GE contributed to selecting idea of study and step-by-step supervision of the research. SK wrote introduction and results section of the manuscript. AD collected samples from endocrine unite of internal medicine department and helped in writing introduction of manuscript. SE edited the manuscript. AS contributed to practical part of the study (real-time PCR). BM helped in methodology writing, editing of manuscript, and final revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This research was approved by the Research Ethics Committee at Menoufia Faculty of Medicine according to 1964 Helsinki Declaration, and informed written consent was taken from every participant in the study; the committee’s reference number is 32019PATH51.
Consent for publication
Consent to publish from the patient had been taken.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Omar, T.A., El-Saeed, G.K., Khodeer, S.A. et al. Vascular endothelial growth factor A with two genetic variants for prediction of mixed microvascular diabetic complications. Egypt J Med Hum Genet 23, 93 (2022). https://doi.org/10.1186/s43042-022-00303-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00303-y