Abstract
Introduction
The benefit of the femoral canal bone plug during total knee arthroplasty (TKA) in reducing blood loss has never been proven. The aim of this meta-analysis was to determine whether the femoral canal bone plug significantly reduces blood loss in primary TKA.
Method
All studies published before December 2021 were searched. The inclusion criteria were randomized controlled trials comparing blood loss between TKA with plugged and unplugged femoral intramedullary canal, respectively. The primary outcome was postoperative hemoglobin reduction.
Results
Five studies with a total of 717 patients (361 in the plugged group, 356 in the unplugged group) met the criteria for inclusion in the meta-analysis. The mean difference in hemoglobin level between the two groups was 0.92 g/dL, with significantly less hemoglobin reduction in the plugged group (95% confidence interval [CI] − 1.64 to − 0.21, p = 0.01). The patients in the plugged group also had a significantly lower risk of receiving a blood transfusion (risk ratio 0.58, 95% CI 0.47–0.73, p < 0.00001).
Conclusions
This meta-analysis demonstrates that using a femoral canal bone plug can significantly reduce blood loss and lower the risk ratio of blood transfusion in patients undergoing TKA.
Similar content being viewed by others
Introduction
Total knee arthroplasty (TKA) is associated with the potential for postoperative blood loss due to extensive soft tissue dissection, uncovered metaphyseal bone cuts, and neglected small vessel injuries [1]. Several studies have reported total blood loss ranging from 600 to 1790 mL and a postoperative transfusion rate of 11–21% [2,3,4]. As in any modern surgery, blood transfusion should be avoided because it might cause rare but severe complications, such as immunological reactions, infections, hemolysis, renal failure, and death [5, 6].
The conventional TKA technique requires drilling of the femoral intramedullary canal for insertion of an intramedullary cutting guide, which is a potential source of blood loss through the opened medullary hole. It was believed that sealing the drill hole with a bone plug or bone cement could help reduce blood loss, hence reducing the need for blood transfusion.
Several studies have compared the amount of blood loss between TKA with and without femoral canal bone plug, but the results remain equivocal [4, 7,8,9,10]. Here we report the results of a meta-analysis aimed to verify the efficacy of the femoral canal bone plug in reducing blood loss and transfusion rate in TKA.
Methods
Search strategy
This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Queen Savang Vadhana Memorial Hospital, The Thai Red Cross Society No. 005/2022. This study was registered at the International Database of Prospectively Registered Systematic Reviews in Health and Social Care (PROSPERO), identification no. CRD42016045758. No informed consent was obtained from the participants included in the study.
We searched the PubMed, Scopus, Cochrane Library, Ovid, EMBASE databases, as well as offline sources, for relevant studies published before December 2021. The search terms were “plug,” “seal,” “total knee replacement,” and “total knee arthroplasty.” We also searched unpublished and ongoing studies in the clinicaltrials.gov and PROSPERO databases for investigations that had similar or different surgical or perioperative protocols but which could affect blood loss.
Inclusion criteria were randomized controlled trials (RCTs) that compared the amount of blood loss in TKA between patients with and without femoral canal bone plugs (‘plugged’ and ‘unplugged’ groups, respectively). Studies without a control group, studies with incomplete data, and retrospective studies were excluded.
The primary outcome was postoperative hemoglobin reduction. The secondary outcomes were blood transfusion rate, total drained blood, and drained blood at 24 h after surgery.
Study identification and selection
Two authors (YK and SN) independently reviewed study identification and selection. Any disagreement was discussed and resolved. Cochrane Reviewers’ Handbook [11] was applied to assess the methodological qualities. Included studies are described in Table 1.
Statistical analysis
Data analysis was performed with RevMan version 5.0.22 (The Nordic Cochrane Centre, Copenhagen, Denmark). Statistical heterogeneities of all outcomes were assessed with the Chi-square test and I2 test. A fixed-effects model was used when the p value was ≥ 0.1 and the I2 value was ≤ 50% (I2 between 0 and 25% = no statistical heterogeneity, I2 between 25.1 and 50% = low statistical heterogeneity). A random-effects model was used when the p-value was < 0.1 and the I2 value was > 50% (I2 between 50.1–75% = moderate statistical heterogeneity, I2 between 75.1 and 100% = high statistical heterogeneity).
Results
Study identifications
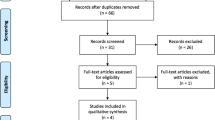
The overall search with selected keywords resulted in the identification of 102 studies, of which only five studies met the inclusion criteria. Four studies used the tourniquet to achieve a bloodless field. All included studies inserted a vacuum drain into the knee and removed it within 72 h; however, no information regarding the use of tranexamic acid was described in all studies. All studies published from 2014 onward used anticoagulant for venous thromboembolism prevention. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram [12] for study identification is shown in Fig. 1. The risk of bias assessments is shown in Fig. 2.
Hemoglobin reduction post-operation (hemoglobin level differences between before and after surgery)
Three studies reported changes in hemoglobin levels before and after surgery, involving 516 patients (255 in the plugged group and 261 in the unplugged group). The change in hemoglobin level was less in the plugged group than in the unplugged group (mean difference 0.92 g/dL; 95% CI − 1.64 to − 0.21, p = 0.01), as shown in Fig. 3). However, most studies did evaluate total blood loss and thus this parameter could not be analyzed.
Total drained blood
All five studies, involving 717 patients (361 in the plugged group and 356 in the unplugged group), reported total drained blood. The mean difference in total drained blood was lower in the plugged group than in the unplugged group (77.99 mL), but the difference was not statistically significant (95% CI − 165.42 to 9.43, p = 0.08) (Fig. 4).
Drained blood at 24-h post-surgery
A total of 516 patients (260 in the plugged group and 256 in the unplugged group) were included in the analysis of drained blood at 24 h. The average difference of drained blood at 24-h post-surgery in the plugged group was 49.06 mL, which was less than in the unplugged group. However, this difference was not statistically significant (95% CI -133.77 to 35.65, p = 0.26) (Fig. 5).
Blood transfusion rate
Blood transfusion was reported in four studies, involving 597 participants (296 in the plugged group and 301 in the unplugged group). All studies had a similar transfusion protocol, including a hemoglobin level of < 8 g/dL or presentation of anemic symptoms). The analysis demonstrated that the plugged group had a statistically lower risk of receiving blood transfusion (risk ratio = 0.58, 95% CI 0.47–0.73, p < 0.00001) (Fig. 6).
Discussion
Total knee arthroplasty is currently one of the most common orthopedic procedures performed in the elderly. Historical reports of blood loss in TKA range from 600 to 1790 mL [2, 3]. Several studies have focused on the amount of blood loss and how to minimize it. Strategies to reduce allogeneic blood transfusion in TKA include a tourniquet, autologous blood transfusion, intraoperative blood saving, and hypotensive anesthesia. Medications such as erythropoietin can help increase preoperative hemoglobin levels. Currently, tranexamic acid, with its antifibrinolytic property, has become the most widely used medication to reduce postoperative blood loss [13, 14].
Femoral canal intramedullary plug is a quick and straightforward surgical technique. However, its efficacy in reducing blood loss in TKA has never been definitively proven. While many studies have reported reduced blood loss with the use of femoral plugs, others report the reverse. The first RCT on blood loss reduction by femoral canal plug was reported by Raut and colleagues [15] in 1993. These researchers showed that the plugged group suffered significantly less blood loss than the unplugged group (mean blood loss: 752 vs. 1002 mL, respectively). However, the data in this study did not provide the standard deviation of the data, and contact with the corresponding author did not result in additional data. Therefore, we excluded this study from our meta-analysis.
Some retrospective studies comparing TKA with and without femoral canal bone plugs have been published. Protzman et al. [16] retrospectively reported 55 patients who underwent TKA, with 26 in the plugged group and 29 in the unplugged group. The mean blood loss was 960.8 mL in the plugged group and 1065.9 mL in the unplugged group, and the difference was not significant. In contrast, Batmaz et al. [17] retrospectively reviewed the outcomes of 288 patients who had TKA, 96 in the plugged group and 192 in the unplugged group. These authors found that the plugged group had a significantly higher postoperative hemoglobin level than the unplugged group (10.01 vs. 9.02 g/dL, respectively), while the preoperative hemoglobin levels were similar (12.5 vs. 12.7 g/dL). They also found that total blood loss was significantly lower in the plugged group than in the unplugged group (729.84 vs. 979.7 mL). To provide reliable results on this issue, the inclusion criteria of the present study were RCTs which compared the amount of blood loss in TKA between patients with and without femoral canal bone plugs. Also, studies without a control group, with incomplete data, or retrospective studies had to be excluded.
We chose four parameters for data analysis in our meta-analysis, namely, hemoglobin reduction, total drained blood, drained blood at 24-h post-surgery, and blood transfusion rate. Although we intended to include the total blood loss as an investigated parameter, no data were available in most of the studies. Hemoglobin reduction was chosen as the primary outcome because it correlated with the total blood loss by direct calculation [18]. In contrast, the drained blood was apparent, but did not represent total blood loss.
The resected bone piece is commonly used for the femoral canal bone plug [19]. Some surgeons also use bone cement to seal the femoral canal opening. Torres-Claramunt et al. [9] allocated TKA patients into three groups: those receiving bone plug or bone cement, and those with no bone plug. We only analyzed results from the plugged and unplugged groups to keep the protocol of all studies in the meta-analysis similar. Although some contemporary femoral component designs have closed boxes that can cover the intramedullary canal and act like a plug, all of the implants used in the included studies were used in the open box system.
The results of the present meta-analysis demonstrate that the plugged group had a significantly lower hemoglobin reduction and a lower transfusion rate than the unplugged group. However, the total drained blood and drained blood at 24 h postoperatively were similar between the two groups. These results demonstrate that significant amounts of blood loss were hidden, a finding supported by other studies which reported that the blood loss was similar in TKA with a drain or TKA without a drain.
There were a number of limitations to this meta-analysis. First, very few studies were available for analysis. Second, some studies did not mention the transfusion criteria with regard to symptoms of anemia. Lastly, the included studies did not mention other variable factors that might affect postoperative blood loss, such as anticoagulants for preventing venous thromboembolism.
Conclusions
This meta-analysis demonstrates that a femoral canal plug could reduce postoperative blood loss and transfusion rate in unilateral primary TKA.
Availability of data and materials
The datasets generated in the current study are not publicly available but are available from the corresponding author.
References
Callaghan JJ, O’Rourke MR, Liu SS (2005) Blood management: issues and options. J Arthroplasty 20(4 Suppl 2):51–54
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Jt Surg Am 81(1):2–10
Safdari MR (2017) Blood loss prevention in total knee arthroplasty (TKA): a systematic review. Rev Clin Med 4(3):102–123
Li X, Qi XB, Han X, Wang W, Liu JN, Guo JC, et al (2017) Effects of sealing the intramedullary femoral canal in total knee arthroplasty: a randomized study. Medicine (Baltimore) 96(29):1–4
Cardone D, Klein AA (2009) Perioperative blood conservation. Eur J Anaesthesiol 26:722–729
Lemaire R (2008) Strategies for blood management in orthopaedic and trauma surgery. J Bone Jt Surg Br 90:1128–1136
Ko PS, Tio MK, Tang YK, Tsang WL, Lam JJ (2003) Sealing the intramedullary femoral canal with autologous bone plug in total knee arthroplasty. J Arthroplasty 18(1):6–9
Kumar N, Saleh J, Gardiner E, Devadoss VG, Howell FR (2000) Plugging the intramedullary canal of the femur in total knee arthroplasty: reduction in postoperative blood loss. J Arthroplasty 15(7):947–949
Torres-Claramunt R, Hinarejos P, Pérez-Prieto D, et al (2014) Sealing of the intramedullar femoral canal in a TKA does not reduce postoperative blood loss: a randomized prospective study. Knee 21(4):853–857
Tanasubsinn N, Tanavalee A, Boonyanuwat W, Ngarmukos S (2017) Effect of bone plugging at the distal femoral drilled hole in total knee arthroplasty on early clinical outcomes. Thai J Orthop Surg 1:3–8
Alerson P, Green S, Higgins JPT (2004) Assessment of study quality: Cochrane reviewers’ handbook 4.2.1. Wiley, Chichester
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2010) Preferred Reporting items for systematic review analyses: the PRISMA statement. Int J Surg 8(5):336–341
Ido K, Neo M, Asada Y, Kondo K, Morita T, Sakamoto T et al (2000) Reduction of blood loss using tranexamic acid in total knee and hip arthroplasties. Arch Orthop Trauma Surg 120:518–520
Sukeik M, Alshryda S, Haddad FS, Mason JM (2011) Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Jt Surg Br 93(1):39–46
Raut VV, Stone MH, Wroblewski BM (1993) Reduction of postoperative blood loss after press-fit condylar knee arthroplasty with use of a femoral intramedullary plug. J Bone Jt Surg Am 75(9):1356–1357
Protzman NM, Buck NJ, Weiss CB (2013) Autologous bone plugs in unilateral total knee arthroplasty. Indian J Orthop. 47(2):182–187
Batmaz AG, Kayaalp ME, Oto O, Bulbul AM (2016) Sealing of femoral tunnel with autologous bone graft decreases blood loss. Acta Chir Orthop Traumatol Cech 83(5):348–350
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280
Vulcano E, Regazzola GM, Murena L, Ronga M, Cherubino P, Surace MF (2015) Femoral bone plug in total knee replacement. Orthopedics 38(10):617–618
Acknowledgements
The authors are particularly grateful to Ms. Warayapa Mingsiritham for her assistance in preparing the manuscript.
Funding
This study has no funding support.
Author information
Authors and Affiliations
Contributions
AT established the design and implemented the research and analysis of the results. YK processed IRB documents. YK and SN independently reviewed study identification and selection. AT, SN, and YK wrote the manuscript together.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Queen Savang Vadhana Memorial Hospital, The Thai Red Cross Society No. 005/2022. This study was registered at the International Database of Prospectively Registered Systematic Reviews in Health and Social Care (PROSPERO), identification no. CRD42016045758. No informed consent was obtained from the participants included in the study.
Consent for publication
All authors declare that this manuscript is licensed for publication under The Knee Surgery and Related Research Journal.
Competing interests
All authors (YK, SN, and AT) declare no conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khanasuk, Y., Ngarmukos, S. & Tanavalee, A. Does the intramedullary femoral canal plug reduce blood loss during total knee arthroplasty?. Knee Surg & Relat Res 34, 31 (2022). https://doi.org/10.1186/s43019-022-00160-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-022-00160-4